4 Respiratory System
Topic: Respiratory System
Text Reference: Chapter 4. Respiratory System
Objectives: Students should be able to…
Identify meanings of key word components of the respiratory system
Prefixes
a- (absence of, without)
an- (absence of, without)
brady- (slow)
dys- (difficult, painful, abnormal, labored)
endo- (within, in)
eu- (normal, good)
hyper- (above, excessive)
hypo- (below, incomplete)
intra- (within, in)
poly- (many, much)
tachy- (fast, rapid)
Combining Forms
adenoid/o (adenoids)
alveol/o (alveolus)
atel/o (imperfect, incomplete)
bronch/o (bronchus)
bronchi/o (bronchus)
capn/o (carbon dioxide)
diaphragmat/o (diaphragm)
epiglott/o (epiglottis)
hem/o (blood)
hemat/o (blood)
laryng/o (larynx)
lob/o (lobe)
muc/o (mucus)
nas/o (nose)
orth/o (straight)
ox/i (oxygen)
pharyng/o (pharynx)
phon/o (sound, voice)
phren/o (diaphragm)
pleur/o (pleura)
pneum/o (lung, air)
pneumon/o (lung, air)
pneumat/o (lung)
pulmon/o (lung)
py/o (pus)
radi/o (x-rays, ionizing radiation)
respir/o (breath, breathing)
rhin/o (nose)
sept/o (septum)
sinus/o (sinus)
somn/o (sleep)
son/o (sound)
spir/o (breathe, breathing)
thorac/o (thorax, chest cavity)
tom/o (to cut, section, slice)
tonsill/o (tonsil)
trache/o (trachea)
Suffixes
-algia (pain)
-ar (pertaining to)
-ary (pertaining to)
-cele (hernia, protrusion)
-centesis (surgical puncture to aspirate fluid)
-eal (pertaining to)
-ectasis (stretching out, dilation, expansion)
-ectomy (excision, cut out)
-emia (in the blood)
-genic (producing, originating, causing)
-gram (the record, radiographic image)
-graph (instrument used to record)
-graphy (process of recording, radiographic imaging)
-ia (condition, diseased state, abnormal state)
-ic (pertaining to)
-itis (inflammation)
-logist (specialist or physician who studies and treats)
-logy (study of)
-meter (instrument used to measure)
-metry (measurement)
-oid (resembling)
-pexy (surgical fixation, suspension)
-plasty (surgical repair)
-pnea (breathing)
-ptysis (spitting, coughing)
-rrhagia (rapid flow of blood, excessive bleeding)
-scope (instrument used for visual examination)
-scopic (pertaining to visual examination)
-scopy (process of visually examining, visual examination)
-spasm (sudden involuntary muscle contraction, spasmodic contraction)
-stenosis (constriction, narrowing)
-stomy (creation of an artificial opening)
-thorax (chest, chest cavity)
-tome (instrument used to cut)
-tomy (cut into, incision)
Apply the rules of medical language to pronounce, break into word parts, and define the following terms.
Label each word part by using the following abbreviations:
P = Prefix
WR = Word Root
CV = Combining Vowel
S = Suffix
CF = Combining Form
Example: osteoarthropathy (ä-stē-ō-är-THROP-ă-thē) – disease of bone and joint
WR CV WR CV S
oste / o / arthr / o /pathy
CF CF
Practice pronouncing and defining these medical terms that are not easily broken into word parts.
asphyxia (ăs-FIK-sē-ă)
aspirate (AS-pĭ-rāt)
epistaxis (ĕp-ĭ-STĂK-sĭs)
influenza (flu) (in-floo-EN-ză)
mucus (MŪ-kŭs)
nebulizer (NEB-yŭ-lī-zĕr)
nosocomial infection (nos-ŏ-KŌ-mē-ăl in-FEK-shŏn)
pleural effusion (PLOOR-ăl ĕ-FŪ-zhŭn)
pulmonary embolism (PE) (PŬL-mō-nĕ-rē EM-bŏ-liĭzm)
pulmonary edema (PŬL-mō-nĕ-rē ĕ-DĒ-mă)
upper respiratory infection
stethoscope (STETH-ŏ-skōp)
sputum (SPŪT-ŭm)
ventilator (VENT-ĭ-lāt-ŏr)
Practice pronouncing and defining these commonly abbreviated terms.
ABGs (arterial blood gases)
AFB (acid-fast bacilli)
ARDS (acute respiratory distress syndrome)
BiPAP (bilevel positive airway pressure)
C&S (culture and sensitivity)
CAP (community-acquired pneumonia)
CF (cystic fibrosis)
CO2 (carbon dioxide)
COPD (chronic obstructive pulmonary disease)
CPAP (continuous positive airway pressure)
CPT (chest physiotherapy)
CT (computed tomography, computerized tomography)
CXR (chest x-ray)
DPI (dry powder inhaler)
flu (influenza)
IPPB (intermittent positive-pressure breathing)
IPF (idiopathic pulmonary fibrosis)
LLL (left lower lobe)
LTB (laryngotracheobronchitis)
LUL (left lower lobe)
MDI (metered-dose inhaler)
NIPPV (non-invasive positive-pressure ventilator)
O2 (oxygen)
OSA (obstructive sleep apnea)
PE(pulmonary embolism or pulmonary edema)
PEP (positive expiratory pressure)
PFM (peak flow meter)
PFTs (pulmonary function tests)
RLL (right lower lobe)
RML (right middle lobe)
RUL (right upper lobe)
SOB (shortness of breath)
SVN (small-volume nebulizer)
TB (tuberculosis)
URI (upper respiratory infection)
VAP (ventilator-associated pneumonia)
Sort the terms from the word lists above into the following categories.
- Disease and Disorder (terms describing any deviation from normal structure and function)
- Diagnostic (terms related to process of identifying a disease, condition, or injury from its signs and symptoms)
- Therapeutic (terms related to treatment or curing of diseases)
- Anatomic (terms related to body structure)
Use terms related to the respiratory system.
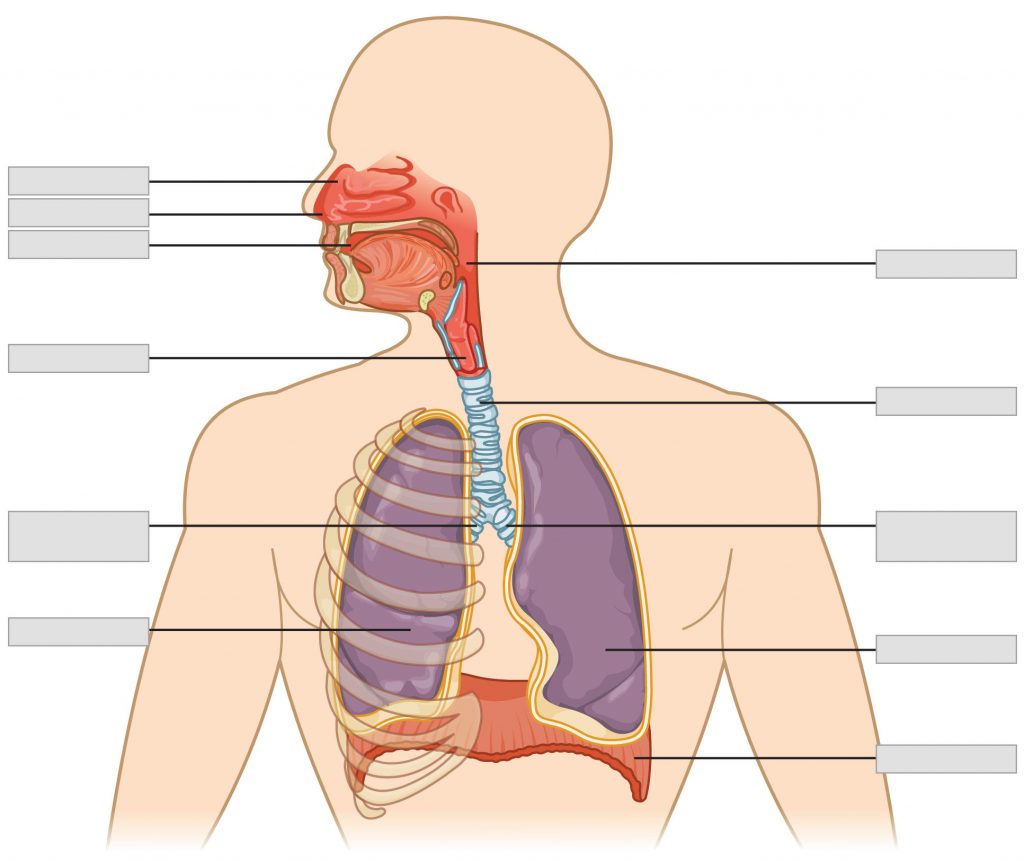
Label the following respiratory system structures.
diaphragm | larynx | left bronchus | left lung | oral cavity | nasal cavity | nostril | pharynx | right bronchus | right lung | trachea
Place the following medical terms in context to complete the scenario below.
allergens | apnea | asthma | breath | diuretic | edema | edema | erythema | exert | heart failure | HEENT | inspiration | lobes | membranes | monitor |
RESPIRATORY SYSTEM – HISTORY & PHYSICAL EXAMINATION
PATIENT NAME: Randy BURNS
AGE: 56
DOB: July 2
SEX: Male
ATTENDING PHYSICIAN: Joyce Mathers, MD, Pulmonology
HISTORY: This 56-year-old male is presenting with a 2-week history of worsening dyspnea not associated with exertion. The patient states that he does not have to ________ himself for his breathing to get difficult. He feels that “he cannot get his breath” sometimes even with lying in bed. He does report developing a cold and runny nose over the last 10 days, but the worsened breathing seemed to have started a few days earlier than this. He reports that the shortness of ________ has progressively gotten worse in the past 2-3 days. Patient does not report any leg or foot ________.
PAST HISTORY: The patient has a life history of asthma triggered by environmental ________ – grass cutting, trees budding in the spring, street dust etc. He has used a puffer when he has symptoms since he was a child. He has a history of congestive ________ (CHF) and sleep ________ for which he uses a CPAP machine nightly.
PHYSICAL EXAMINATION: GENERAL APPEARANCE: The patient appears laboring in breathing. He is quite distressed. VITAL SIGNS: Temperature 97.1, pulse 88, blood pressure 121/86, weight 209 pounds, height 5 feet 8 inches. ________ : Eye exam PERRLA. Normocephalic, atraumatic. Moist mucous ________ . No oropharyngeal ________. No signs of infection. Tongue is coated but tonsils are clear. NECK: Supple. No lymphadenopathy. No bruits. LUNGS: There is marked wheezing on ________ bilaterally. Some minimal evidence of consolidation in the lower ________ bilaterally. No rales or rubs. CARDIAC: Irregular rate and rhythm, variable S1 and S2. EXTREMITIES: Some pedal and ankle ________ noted in low extremities. No cyanosis or clubbing.
ASSESSMENT AND PLAN
1. Acute shortness of breath with a history of allergic ________. Rule out upper respiratory infection (URI). Will order chest x-ray stat.
2. Atrial fibrillation. Patient has a controlled rate. Will administer one dose of Lovenox overnight.
3. Mild symptoms of CHF due to lower extremity edema. Will administer Aldactone to bring this under control. Will ________ the patient’s diuretic volume.
4. Plan to admit patient overnight for observation to await stat CXR result and to monitor the effects of ________ and anticoagulant therapies.
Joyce Mathers, MD Pulmonology
Place the following medical terms in context to complete the scenario below.
antibiotics | atelectasis | basal | COPD | dyspnea | hemoptysis | Oxygen | pleural | q.d. | thoracostomy | wheezing
RESPIRATORY SYSTEM – CONSULTATION REPORT
PATIENT NAME: Wayne SAUNDERS
AGE: 59
DOB: September 7
SEX: Male
DATE OF CONSULTATION: March 29
CONSULTANT: Joyce Mathers, MD, Pulmonology
REASON FOR CONSULTATION: Sudden onset dyspnea and respiratory distress.
HISTORY: This garrulous 59-year-old was seen in the ER today with a complaint of sudden onset ________ and some respiratory distress. Denies any nausea, vomiting, chest pain, ________ , cough, fever or chills.
PAST HISTORY: Is positive for asthma and ________ as patient is a lifelong smoker at 1+ packs per day.
ASSESSMENT: CHEST has good air entry bilaterally. No ________ . Bilateral ________ crackles are noted. Some dullness to percussion on the left. CT scan was ordered and shows a left ________ effusion and acute pneumothorax due to infectious process. Probable comprehensive ________.
MEDICATIONS
1. Adalat 30 mg ________
2. Atenolol 50 mg (half dose) q.d.
3. Flonase 50 mcg one spray on each side q.d.
4. Zoloft 100 mg once q.d.
PLAN
1. Admit patient to the unit for treatment and possible left ________ if indicated by lack of improvement on standard therapy.
2. Treat with a course of ________ for the URI.
3. ________ therapy if indicated by 02 sats.
4. Repeat CT scan in 48 hours.
__________________________________
Joyce Mathers, MD, Pulmonology
Place the following medical terms in context to complete the scenario below.
apex | childhood | dyspnea | expiration | flu shot | hepatotoxis | myoplasmal | kidney | mid-thoracic | pulmonary | rales | rasping | respiratory | rhinorrhea | shadowing | urinalysis | vaccine | x-ray
RESPIRATORY SYSTEM – CONSULTATION REPORT
PATIENT NAME: Mateo DIAZ
AGE: 22
DOB: June 25
SEX: Male
DATE OF CONSULTATION: April 16
CONSULTING PHYSICIAN: Joyce Mathers, MD Pulmonology
HISTORY: This 22-year-old Hispanic gentleman is referred to me for a 2-week history of new rasping cough associated with a dull right ________ intercostal discomfort. He has some associated ________ on exertion but is otherwise well with no presenting symptoms of a cold or ________ infection. No fever, sputum or ________.
PAST HISTORY: He has a history of ________ asthma that seemed to disappear after he hit his mid-20s. He has a history of extensive travel for work and leisure and most recently was on a work trip to Wuhan, China in late December. He receives a ________ annually and did have the most recent ________ in October 2019.
His physical exam is relatively unremarkable. Blood pressure is 120/83, respirations 12. Temperature normal at 37. Chest exam is CTA with no ________, rhonchi or wheezes. Even on a forced exhalation, we could not reproduce the ________ cough symptom.
ASSESSMENT: A PA and lateral chest ________ revealed a new infiltrate and ________ along the left mid-lung margin all the way to the . Spirometry showed normal pressures on forced ________.
PLAN
1. Rule out ________ pneumonia versus other lung infection or infiltrates such as granulomatosis, aspergillosis or sarcoidosis.
2. CBC with differential, chem panel, ESR, ACE, ________ and mycoplasma titres.
3. Repeat full ________ function tests (PFTs) in 2 weeks.
If required, will treat with Amphotericin B, Tosufloxacin, Macrolide or similar. If any of these treatments are indicated, weekly LFTs and ________ function testing will be required as these classes of drugs is notoriously ________ and nephrotoxic.
I will see the patient again in approximately 4 days to review the results and decide on a course of action – more testing or appropriate treatments as indicated above.
____________________________
Joyce Mathers, MD Pulmonology
Test your knowledge by answering the questions below.
A small bulbous, teardrop-shaped structure located at the apex of the soft palate…
- Posterior
- Lymphocytes
- Uvula
Located at the anterior region of the nasal cavity and is composed of bone…
- Fauces
- Glottis
- Hard palate
A ridge of cartilage that separates the two main bronchi…
- Carina
- Alveolar Duc
- Eupnea
Serves as an airway and is continuous with the nasal cavity
- Conducting zone
- Hilum
- Nasopharynx
Consists of the surface and skeletal structures that result in the outward appearance of the nose and contribute to its numerous functions…
- Pharynx
- Inferior
- External nose

