11 Lymphatic and Immune Systems
Topic: Lymphatic and Immune Systems
Text Reference: Chapter 11. Lymphatic and Immune Systems
Objectives: Students should be able to…
Identify meanings of key word components of the lymphatic and immune systems
Prefixes
a- (absence of, without)
an- (absence of, without)
ana- (up, upward or back, backward)
brady- (slow)
inter- (between)
pan- (all)
Combining Forms
immun/o (immune, immunity)
lymph/o (lymph, lymph tissue)
lymphaden/o (lymph gland, lymph node)
myel/o (bone marrow, spinal cord)
splen/o (spleen)
thym/o (thymus gland)
tox/o (poison)
Suffixes
-ac (one affected with)
-apheresis (withdrawal or removal)
-cyte (cell)
-ectomy (excision, cut out)
-itis (inflammation)
-logist (specialist, physician who studies and treats)
-logy (study of)
-megaly (enlarged, enlargement)
-oid (resembling)
-oma (tumor, swelling)
-osis (abnormal condition)
-pathy (disease)
-penia (decrease, deficiency)
-poiesis (formation, production)
-rrhaphy (suturing)
Apply the rules of medical language to pronounce, break into word parts, and define the following terms.
Label each word part by using the following abbreviations:
P = Prefix
WR = Word Root
CV = Combining Vowel
S = Suffix
CF = Combining Form
Example: osteoarthropathy (ä-stē-ō-är-THROP-ă-thē) – disease of bone and joint
WR CV WR CV S
oste / o / arthr / o /pathy
CF CF
Practice pronouncing and defining these medical terms that are not easily broken into word parts.
acute inflammation (ă-KŪT in-flă-MĀ-shŏn)
afferent lymphatic vessels (AF-ĕ-rĕnt lim-FAT-ik VES-ĕls)
allergen (AL-ĕr-jĕn)
allergist (AL-ĕr-jist)
allergy (AL-ĕr-jē)
antibody (ANT-i-bod-ē)
antigen (ANT-i-jĕn)
apoptosis (ap-ŏp-TŌ-sĭs)
autoimmune disease (OT-ō-im-yūn diz-ĒZ)
bone marrow (bōn MAR-ō)
chronic inflammation (KRON-ĭk in-flă-MĀ-shŏn)
chyle (kīl)
efferent lymphatic vessels (EF-ĕ-rĕnt lim-FAT-ik VES-ĕls)
erythroblastosis fetalis (ĕ-rĭth-rō-blăs-TŌ-sĭs fĕ-TAL-ĭs)
graft-versus-host disease (GVHD)
histamine (HIS-tă-mēn)
immunity (im-Ū-nĭt-ē)
immunodeficiency (im-yŭ-nō-dĕ-FISH-ĕn-sē)
immunological memory (im-yŭ-NOL-ŏ-jē- kăl MEM-ŏ-rē)
inflammation (in-flă-MĀ-shŏn)
innate immune response (ĭn-NĀT i-MŪN ri-SPONS)
intersititial (in-tĕr-STISH-ăl)
intersititial space (in-tĕr-STISH-ăl spās)
lymph (limf)
lymph node (limf nōd)
passive immunity (PĂS-ĭv im-Ū-nĭt-ē)
severe combined immunodeficiency disease (SCID) (im-yŭ-nō-dĕ-FISH-ĕn-sē)
spleen (splēn)
thymus (THĪ-mŭs)
tonsils (TON-sĭls)
vaccine (vak-SĒN)
Practice pronouncing and defining these commonly abbreviated lymphatic and immune terms.
AIDS (acquired immunodeficiency syndrome)
CBC and DIff (complete blood count and differential)
CD4+ Cell (helper T cell)
CD8+ Cell (cytotoxic T cell)
CMV (cytomegalovirus- causes opportunistic AIDS-related infection)
Crypto (Cryptococcus- causes opportunistic AIDS-related infection)
ELISA (enzyme-linked immunosorbent assay – test to detect anti-HIV antibodies)
G-CSF (granulocyte colony-stimulating factor – cytokine that promotes neutrophil production)
GM-CSF (granulocyte macrophage colony-stimulating factor – cytokine secreted by macrophages to promote growth of myeloid progenitor cells and their differentiation to granulocytes)
GVHD (Graft-versus-host Disease)
HAART (highly active antiretroviral therapy – use of combinations of drugs that are effective against AIDS)
Hct (hematocrit)
HDN (hemolytic disease of the newborn)
Hgb (hemoglobin)
Histo (histoplasmosis-fungal infection seen in AIDS patients)
HIV (human immunodeficiency virus)
HSV (herpes simplex virus)
Iga, IgD, IgE, IgG, IgM (immunoglobulins)
IL1 to IL38 (interleukins)
IV (Intravenous)
KS (Kaposi sarcoma)
MAI (Mycobacterium avium-intracellulare (MAI) complex – group of pathogens that cause lung and systemic disease in immunocompromised patients)
MoAb (monoclonal antibody)
NHL (non-Hodgkin lymphoma)
PCP (Pneumocystis pneumonia-opportunistic AIDS-related infection)
PI (protease inhibitor)
SCID (severe combined immunodeficiency)
SPECT (single-photon emission computed tomography)
Treg (regulatory T cell (suppressor T cell)
Toxo (toxoplasmosis- parasitic infection associated with AIDS)
WBC (White Blood Cell)
Sort the terms from the word lists above into the following categories.
- Disease and Disorder (terms describing any deviation from normal structure and function)
- Diagnostic (terms related to process of identifying a disease, condition, or injury from its signs and symptoms)
- Therapeutic (terms related to treatment or curing of diseases)
- Anatomic (terms related to body structure)
Use terms related to the lymphatic and immune systems.
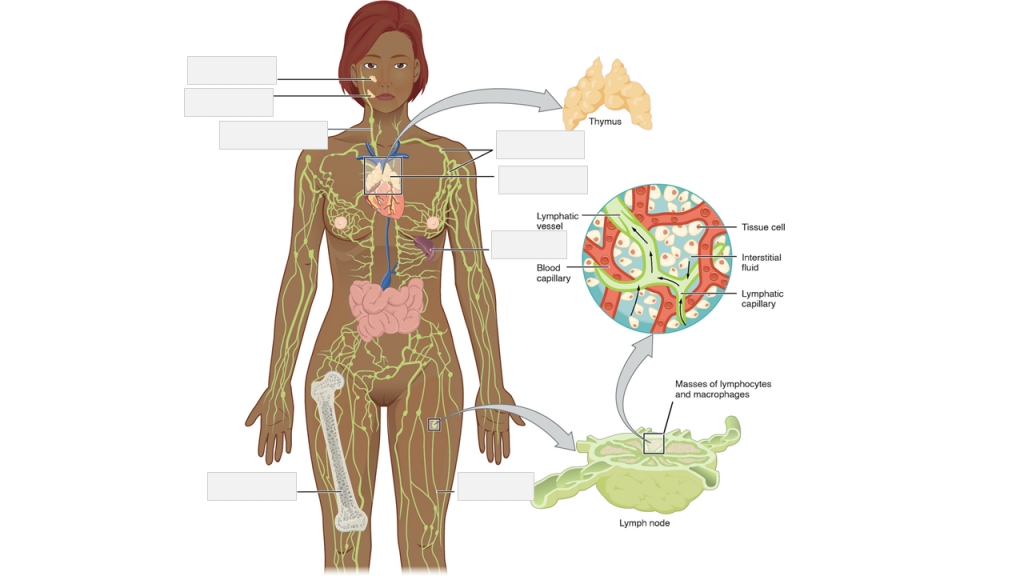
Label the following lymphatic system anatomy.
adenoid | bone marrow | lymph nodes | lymph vessel | right lymphatic duct, entering vein | spleen | thymus | tonsil
Place the following medical terms in context to complete the scenario below.
allergies | dander | distress | drainage | Dyspnea | heart | iron | itchy | medications | q.d. | rhinitis | runny
LYMPHATIC SYSTEM – MEDICAL REPORT
PATIENT NAME: Sally WESSON
AGE: 43
SEX: Female
DOB: September 26
DATE OF ASSESSMENT: March 20
ATTENDING PHYSICIAN: Trevor Sharpe, MD
CHIEF COMPLAINT: Allergies.
HISTORY: A 43-year-old Asian female states being very tired and irritable. She had presented watery and ________ eyes, itchy throat, sneezing, ________, and stuffy nose. She has family history of ________. She always struggled with many different allergies: dust, pollen, cat and dog ________. She had tried different types of over-the-counter allergy ________, but they didn’t help to alleviate the symptoms. She is currently taking Reactine 5 mg daily which does not relieve all of her symptoms.
PHYSICAL EXAMINATION: GENERAL: Patient is pale and in moderate ________. VITAL SIGNS: Weight 160 pounds, B/P 120/80, ________ rate 90 beats per minute, respiratory rate 18 per minute, temperature 98.6 F. HEENT: EYES: Red, watery, itching, burning and swelling. EARS: Normal. NOSE: Mouth breathing, sneezing, runny and itchy nose, post-nasal ________, nasal congestion. THROAT: Itchy and swollen. CHEST: ________ and wheezing.
MEDICATIONS
- Reactine 5 mg ________.
- Escitalopram 20 mg q.d.
- Lorazepam 0.5 mg p.r.n. nightly at bedtime.
- Fenofibrate 145 mg q.h.s.
ASSESSMENT
- Patient has severe seasonal allergic ________.
- Possible anemia.
PLAN
- Recommended Reactive 10 mg q.d.
- Referred to an allergist to provide patient more options for allergy treatments.
- Ordered a blood work to check her ________ and cholesterol levels.
- Follow up in 4 days to review her blood work results.
_________________________________
Trevor Sharpe, MD
Place the following medical terms in context to complete the scenario below.
cervical | crypts | dysphagia | erythema | fatigued | fever | gargles | pseudomembranes | stones | temperature | tonsillectomy | tonsillitis | tonsillolith
LYMPHATIC SYSTEM – MEDICAL REPORT
PATIENT NAME: Celine CAMERON
AGE: 16
SEX: Female
DOB: March 25
DATE OF ASSESSMENT: August 4
ATTENDING PHYSICIAN: Grant Talbot, MD, Pediatrics
HISTORY: This is a 16-year-old female today with complaints of throat pain. She has been struggling with inflamed tonsils for the last 2 weeks. The patient claims that tonsil ________ are forming and that a white film has appeared over their tonsils. She has been feeling very ________, has developed a mild ________ and occasionally feel nauseous.
The client has a family history of ________ resulting in tonsillectomy. She mentioned that her grandmother experienced recurrent tonsillitis around the same age. The condition of tonsillitis has occurred on 2 other occasions in the past 5 months.
PHYSICAL AND EXAMINATION: Ms. Cameron is in no acute distress. She appears fatigued. VITAL SIGNS: Blood Pressure 132/83, ________ is slightly elevated at 99.6, pulse 67. She is in generally in good condition. Throat palpation was performed. There is significant enlargement of the ________ lymph nodes. She appears to be experiencing ________. Throat was examined and revealed swelling, ________ and tonsillar ________ visible. A ________ was seen to be forming within one of the crypts. Celine’s claims of ________ were also confirmed. She denies any symptoms such as a nasal discharge, cough, or abdominal pain. Throat was swabbed.
ASSESSMENT: Ms. Cameron appears to be experiencing recurrent tonsillitis correlated to exaggerated tonsillar crypts. Possible ________ may be required.
PLAN
- Patient was given a referral to an ENT specialist and may require tonsillectomy.
- The patient was instructed to follow a diet of soft, smooth foods and soothing liquids.
- It was suggested that the patient use saltwater ________ in the mornings and before bed.
- A prescription of Amoxicillin 400 mg p.o. p.c.
___________________________________
Grant Talbot, MD, Pediatrics
Place the following medical terms in context to complete the scenario below.
dysphagia | enlarged | erythromycin | ibuprofen | lymph | prescribed | surgery | tonsillectomy
LYMPHATIC SYSTEM – MEDICAL REPORT
PATIENT NAME: Jason MACDONALD
AGE: 7
SEX: Male
DOB: August 19
DATE OF ASSESSMENT: November 15
ATTENDING PHYSICIAN: Grant Talbot, MD, Pediatrics
DIAGNOSIS: Tonsillitis
HISTORY: This 7-year-old white male has been seen by me on several occasions over the last two years. He has complained of pharyngitis, ________ , and fever. I have ________ erythromycin in the past.
PHYSICAL EXAMINATION: When I examined Jason today, he once again had the same complaints as in the past. I also noticed that the ________ nodes in his neck were ________ and tender. He had a temperature of 39 degrees.
TREATMENT: I gave Jason ________ for his fever and prescribed ________ again.
PLAN: It is my recommendation that Jason undergo a ________ . Jason’s parents are in agreement. I will make the arrangements for Jason’s ________.
_________________________
Grant Talbot, MD, Pediatrics
Test your knowledge by answering the questions below.
Vasoactive mediator in granules of mast cells and is the primary cause of allergies and anaphylactic shock…
- Mast cell
- Cisterna chyli
- Histamine
Large duct that drains lymph from the lower limbs, left thorax, left upper limb, and the left side of the head…
- Plasma cell
- Thoracic duct
- Lymph
Primary lymphoid organ; where t lymphocytes proliferate and mature…
- Lymphatic capillaries
- Thymus
- Antigen
Tissue found inside bones; the site of all blood cell differentiation and maturation of b lymphocytes…
- Bone marrow
- Interferons
- Neutrophil
Ability of the adaptive immune response to mount a stronger and faster immune response upon re-exposure to a pathogen…
- Immunological memory
- Chemokine
- Barrier defenses

