13 Skeletal System
WTCS Learning Objectives
- Apply the rules of medical language to build, analyze, spell, pronounce, abbreviate, and define terms as they relate to the musculoskeletal system
- Identify meanings of key word components of the musculoskeletal system
- Categorize diagnostic, therapeutic, procedural or anatomic terms related to the musculoskeletal system
- Use terms related to the musculoskeletal system
- Use terms related to the diseases and disorders of the musculoskeletal system
Skeletal System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Musculoskeletal System.
Introduction to the Skeletal System
The skeletal system forms the framework of the body. It is the body system composed of bones, cartilage and ligaments. Each bone serves a particular function and varies in size, shape and strength. Bones are weight-bearing structures in your body and can therefore change in thickness as you gain or lose weight. The skeletal system performs the following critical functions for the human body:
- supports the body
- facilitates movement
- protects internal organs
- produces blood cells
- stores and releases minerals and fat
Watch this video:
Media 13.1. The Skeletal System: Crash Course A&P #19 [Online video]. Copyright 2015 by CrashCourse.
Skeletal System Medical Terms
Anatomy (Structures) of the Skeletal System
The skeletal system includes all of the bones, cartilages, and ligaments of the body that support and give shape to the body and body structures. The skeleton consists of the bones of the body. For adults, there are 206 bones in the skeleton. Younger individuals have higher numbers of bones because some bones fuse together during childhood and adolescence to form an adult bone. The primary functions of the skeleton are to provide a rigid, internal structure that can support the weight of the body against the force of gravity, and to provide a structure upon which muscles can act to produce movements of the body.
In addition to providing for support and movements of the body, the skeleton has protective and storage functions. It protects the internal organs, including the brain, spinal cord, heart, lungs, and pelvic organs. The bones of the skeleton serve as the primary storage site for important minerals such as calcium and phosphate. The bone marrow found within bones stores fat and houses the blood-cell producing tissue of the body.
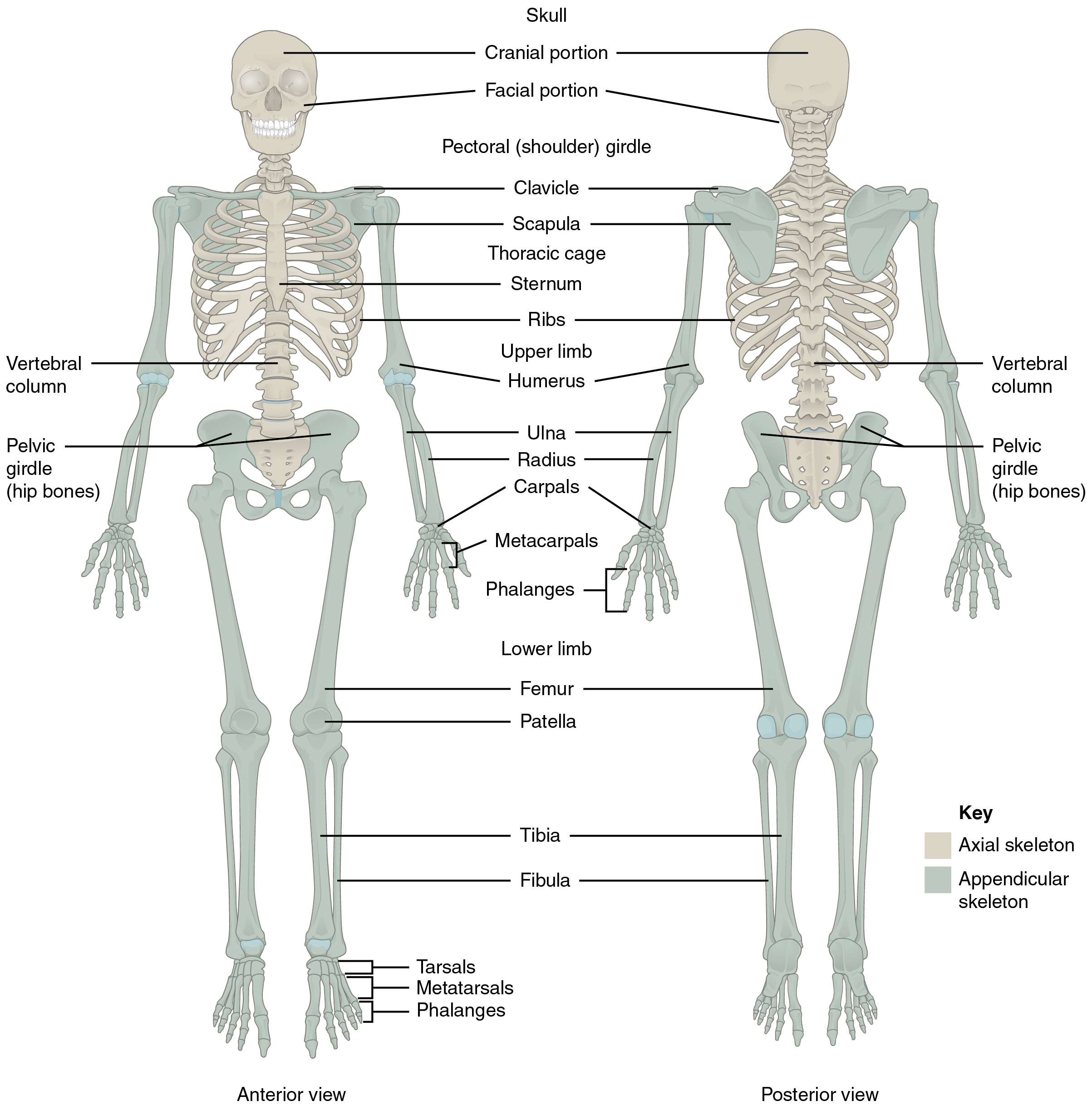
The skeleton is subdivided into two major divisions: the axial and appendicular.
The Axial Skeleton
The axial skeleton forms the vertical, central axis of the body and includes all bones of the head, neck, chest, and back (see Figure 13.1). It serves to protect the brain, spinal cord, heart, and lungs. It also serves as the attachment site for muscles that move the head, neck, and back, and for muscles that act across the shoulder and hip joints to move their corresponding limbs.
The axial skeleton of the adult consists of 80 bones including the skull, the vertebral column, and the thoracic cage. The skull is formed by 22 bones. Also associated with the head are an additional seven bones, including the hyoid bone and the ear ossicles (three small bones found in each middle ear). The vertebral column consists of 24 bones, each called a vertebra, plus the sacrum and coccyx. The thoracic cage includes the 12 pairs of ribs, and the sternum, the flattened bone of the anterior chest.
The cranium or skull supports the face and protects the brain. It is subdivided into the bones of the skull and the bones of the face.
Bones of the Skull
- Frontal – forms the forehead
- Parietal – the upper lateral sides of the cranium
- Occipital – the posterior skull and base of the cranial cavity
- Temporal – the lower lateral sides of the cranium
- Sphenoid -the ‘keystone’ bone that forms part of the base of skull and eye sockets
- Ethmoid – forms part of the nose and orbit and base of cranium
- Auditory ossicles – the small bones of the middle ear
- External auditory meatus – the external opening of ear and temporal bone
Bones of the Face
- Zygomatic – the cheekbone
- Maxillary – the upper jaw and hard palate
- Palatine – the lateral walls of the nose
- Lacrimal – the walls of the orbit
- Inferior conchae – the lower lateral wall of the nasal cavity
- Vomer – the separates the left and right nasal cavity
- Mandible – the lower jaw bone (The only movable bone of the skull)
- Hyoid – the bone located between the mandible and larynx, not connected to other bones
Bones of the Vertebral Column
The vertebral column is also known as the spinal column or spine (see Figure 13.2). It consists of a sequence of vertebrae (singular = vertebra), each of which is separated and united by an intervertebral disc. Together, the vertebrae and intervertebral discs form the vertebral column. It is a flexible column that supports the head, neck, and body and allows for their movements. It also protects the spinal cord, which passes down the back through openings in the vertebrae.
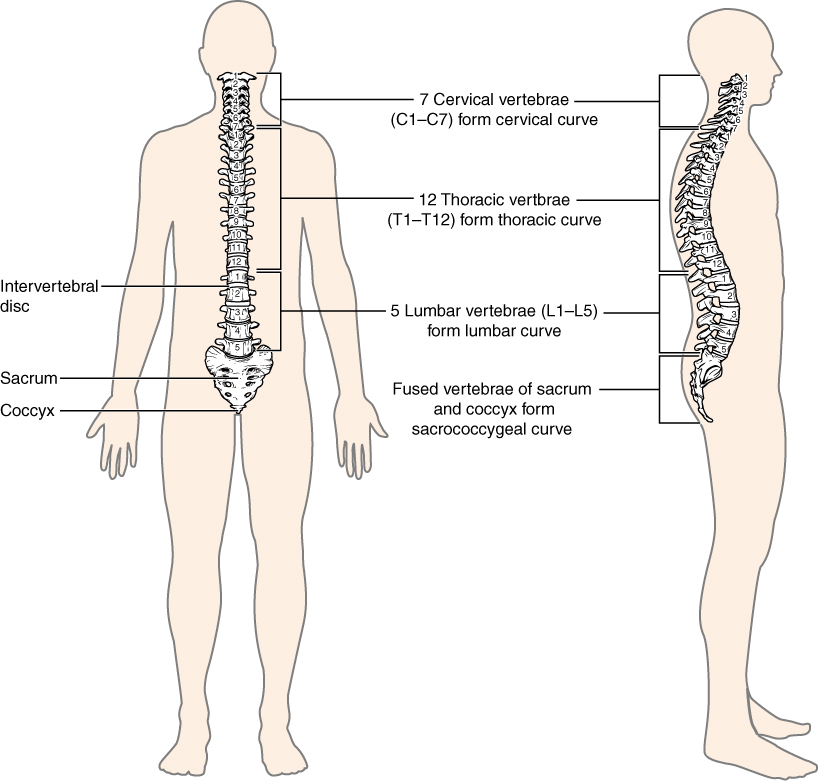
Types of Vertebrae
- Cervical – C1 to C7 – the first 7 vertebrae in the neck region
- Thoracic – T1 to T12 – the next 12 vertebrae that forms the outward curvature of the spine
- Lumbar – L1 to L5 – the next 5 vertebrae that forms the inner curvature of spine
- Sacrum – the triangular-shaped bone at the base of the spine
- Coccyx – the tailbone
Bones of the Thoracic Cavity
The thoracic cage (rib cage) forms the thorax (chest) portion of the body. It consists of the 12 pairs of ribs with their costal cartilages and the sternum (see Figure 13.3). The ribs are anchored posteriorly to the 12 thoracic vertebrae (T1–T12). The thoracic cage protects the heart and lungs.
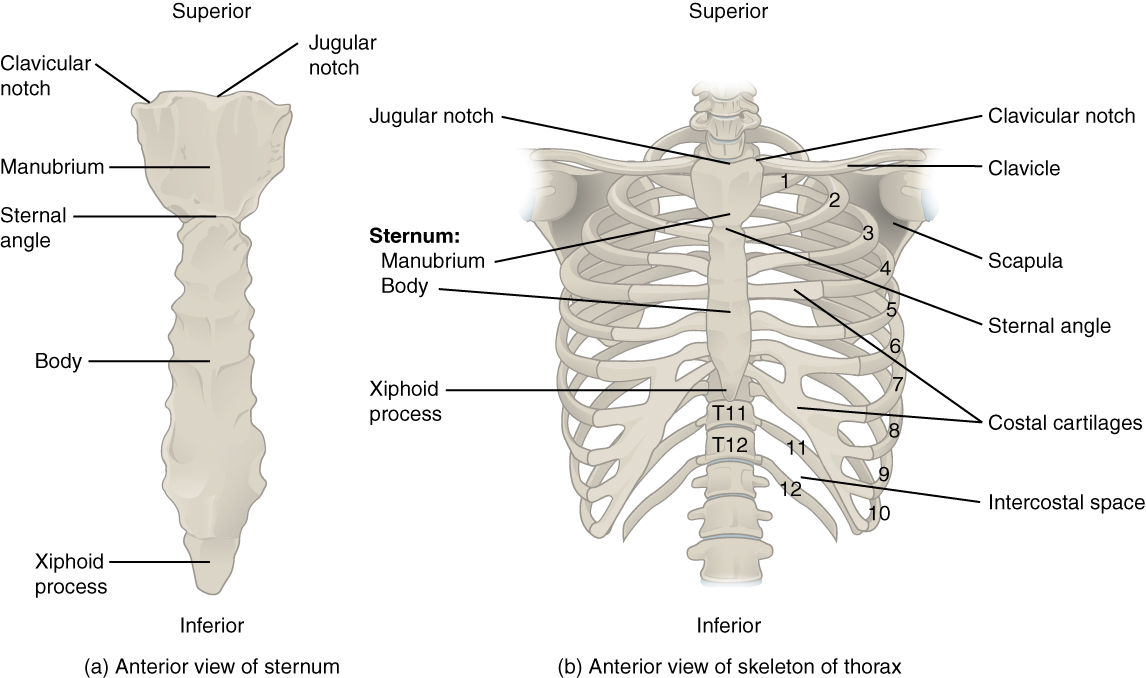
Ribs
There are 12 sets of ribs and can be divided as such:
- 7 true ribs as they are attached to the front of the sternum
- 3 false ribs as they are attached to the cartilage that joins the sternum
- 2 floating ribs as they are not attached to the front of the sternum
Sternum
The sternum, also known as the breast bone, is divided into 3 parts:
- manubrium – the upper portion of the breast bone
- body – the middle portion of the breast bone
- xiphoid process – the lower portion of the breast bone and is made up of cartilage
Concept Check
Answer the following questions:
- What is the medical term for the upper jaw bone and for the lower jaw bone?
- How many bones make up the cervical region of the vertebral column?
The Appendicular Skeleton
Bones of the Pectoral Girdle
- Scapula – the shoulder blades
- Clavicle – the collar bones. It connects the sternum to the scapula
- Acromion – the extension that forms the bony point of the shoulder
Bones of the Upper Limbs
The bones of the upper limbs include the bones of the arms, wrists, and hands.
Bones of the Arm
- Humerus – the bone in upper arm
- Radius – the bone that runs thumb-side of the forearm
- Ulna – the bone that runs on the side of the little finger of the forearm
Watch this video:
Media 13.2. Radius and Ulna [Online video]. Copyright 2013 by UCDenver Anatomy Lab 3244.
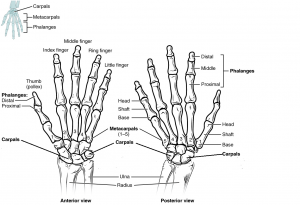
Bones of the Wrist and Hand
- Carpals – the wrist bones
- Metacarpals – the bones in the palm of hand
- Phalanges – the finger and toe bones
Each phalanx has three bones: the distal, medial, and proximal. The exception is the thumb and big toe which has two bones: distal and proximal. See Fig 13.4 below. There are 30 bones in each upper limb. Can you count them on your limb?
Bones of the Pelvic Region
The bones of the pelvic region protect the reproductive, urinary, and excretory organs.
- Pelvic girdle – the hip or coxal bone. It is formed by the fusion of three bones during adolescence
- Illium – the largest part of the hip bone
- Ischium – the lower portion of pelvic girdle
- Pubis – the anterior portion of pelvic girdle
- Pelvis – consists of four bones: the left and right hip bones as well as the sacrum and coccyx
- Acetabulum – the large socket in the pelvic bones that holds the head of the femur
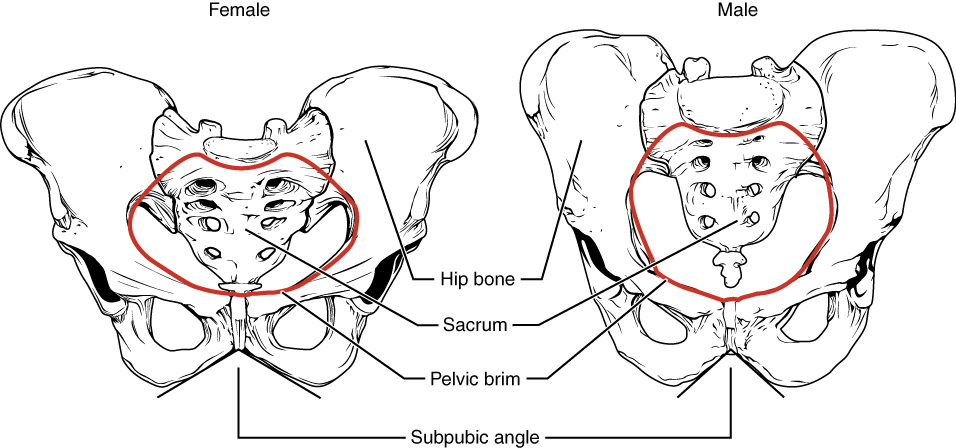
The shape of the pelvic girdle is different for males than females. In the male, it is a funnel shape. In the female it is shaped like a basin to accommodate for the fetus during pregnancy (see Figure 13.5).
Bones of the Lower Limbs
The bones of the lower limb include bones of the leg and the feet.
Bones of the Leg
- Femur – the thigh bone and is also referred to the upper leg bone. It is the longest and strongest bone in the human body
- Patella – the knee cap
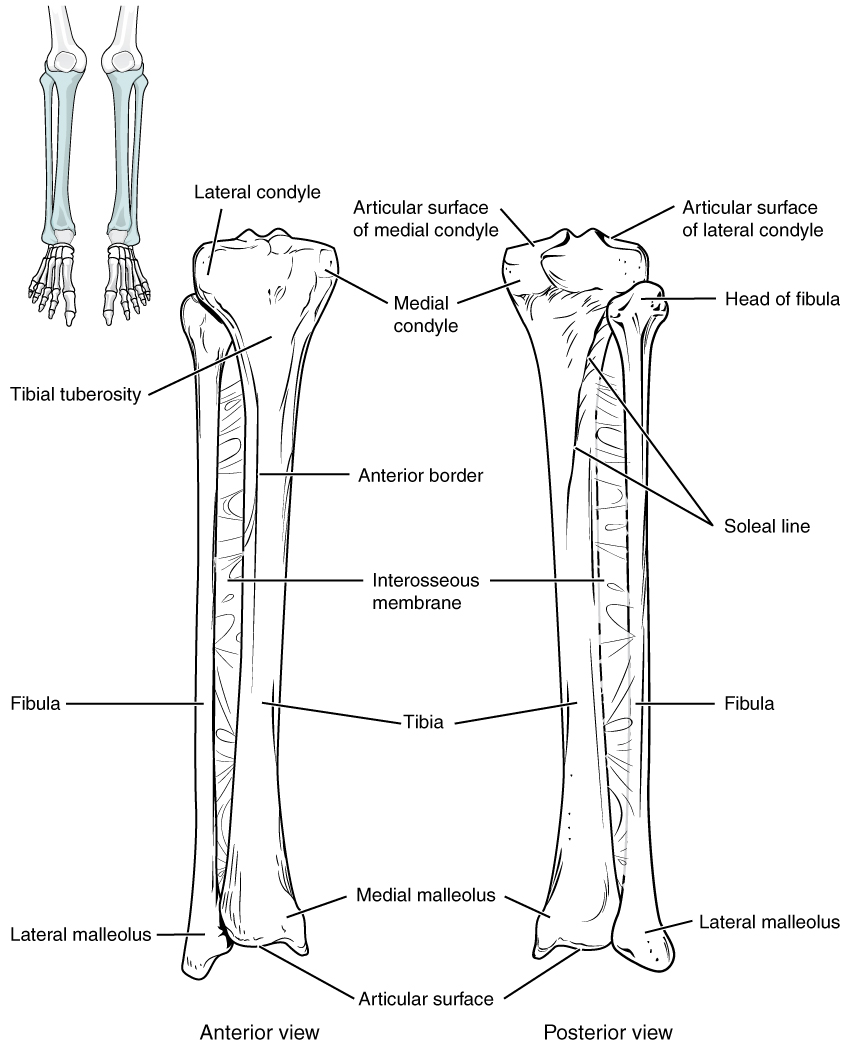
- Tibia – the shin bone. It is a medial bone and the main weight-bearing bone of the lower leg
- Fibula – the smaller of the lower leg bone (see Figure 13.6)
Bones of the Ankles and Feet
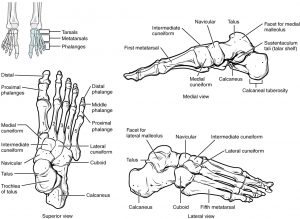
- Tarsals – the ankle bones (7 total)
- Malleous – the bony protrusions of the ankle bones
- Talus – the superior ankle bones
- Calcaneous – the heel bones
- Metatarsals – the foot bones
- Phalanges – the bones of the toes (see Figure 13.7)
Concept Check
Answer the following questions:
- Is the humerus the same as the funny bone?
- What is the medical term for the kneecap?
Anatomy Labeling Activity
Physiology (Function) of the Skeletal System
The bones of the skeletal system is comprised of an inner spongy tissue referred to as bone marrow. There are two types of bone marrow, red and yellow. The red bone marrow produces the red blood cells and it does so by a process called hematopoiesis. The yellow bone marrow contains adipose tissues which can be a source of energy. The bones of the skeletal system also store minerals such as calcium and phosphate. These minerals are important for the physiological processes in the body and are released into the bloodstream when levels are low in the body.
Joints
Watch this video:
Media 13.3. Joints: Crash Course A&P #20 [Online video]. Copyright 2015 by CrashCourse.
Most bones connect to at least one other bone in the body. The area where bones meet bones or where bones meet cartilage are called articulations. Joints can be classified based on their ability to move. At movable joints, the articulating surfaces of the adjacent bones can move smoothly against each other. However, other joints may be connected to each other by connective tissue or cartilage. These joints are designed for stability and provide for little or no movement. Importantly, joint stability and movement are related to each other. This means that stable joints allow for little or no mobility between the adjacent bones. Conversely, joints that provide the most movement between bones are the least stable.
Based on the function of joints, there are 3 types of joints:
- Synarthrosis (sin-ahr-throh-seez) joints which allow no movement
- example: joints of the skull
- Amphiarthrosis (am-fee-ahr-throh-sis) joints which allow some movement
- example: joints of the pubic symphysis
- Diarthrosis (dahy-ahr-throh-seez) joints which allow for free movement
- example: joints of the knee
Structures associated with joints are:
- Cartilage – the elastic connective tissue that is found at the ends of bones, nose tip, etc.
- Synovial membrane – the lining or covering of synovial joints
- Synovial fluid – the lubricating fluid found between synovial joints
- Ligaments – the tough, elastic connective tissue that connects bone to bone
- Tendons – the fibrous connective tissue that attaches muscle to bone
- Bursa – the closed, fluid-filled sacs that works as a cushion
- Meniscus – C-shaped cartilage that act as shock absorbers between bones
Body Movements
Synovial joints are movable joints and provide most of the body movements. Body movement occurs when the bones, joints and muscles work together.
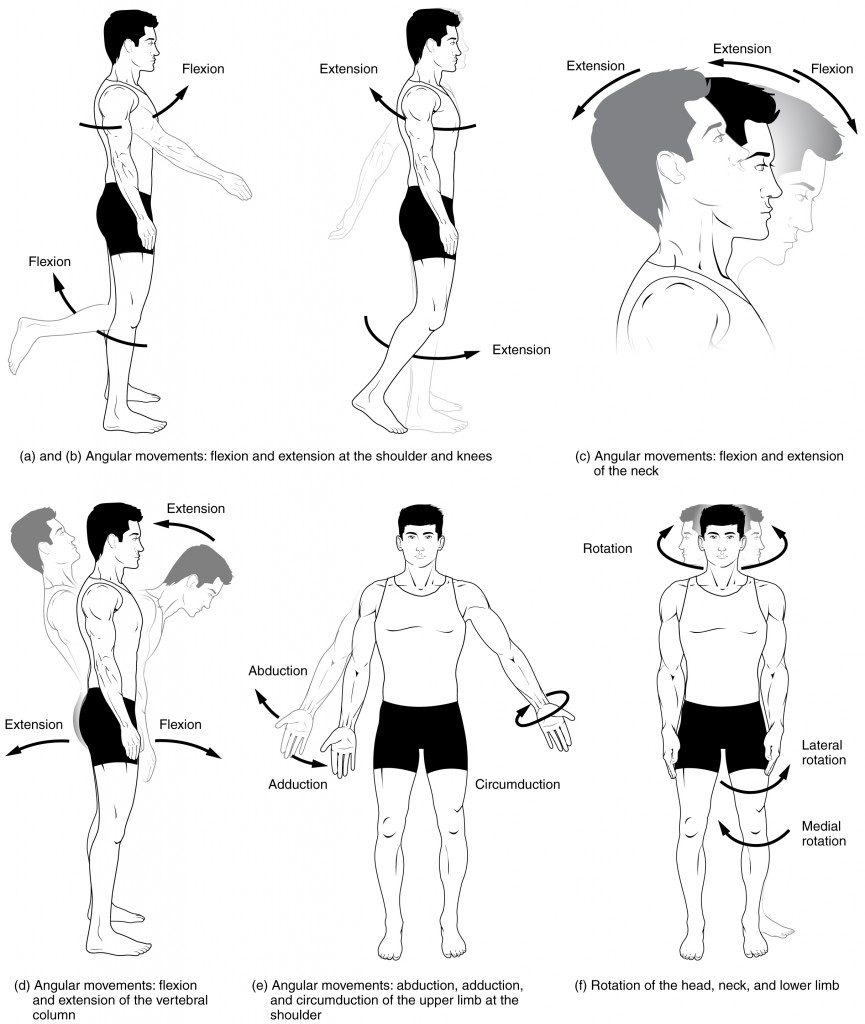
Flexion and Extension
Flexion and extension are movements that take place within the sagittal plane and involve anterior or posterior movements of the body or limbs. For the vertebral column, flexion (anterior flexion) is an anterior (forward) bending of the neck or body, while extension involves a posterior-directed motion, such as straightening from a flexed position or bending backward. Lateral flexion is the bending of the neck or body toward the right or left side. These movements of the vertebral column involve both the joints as well as the associated intervertebral disc.
In the limbs, flexion decreases the angle between the bones (bending of the joint), while extension increases the angle and straightens the joint (see Figure 13.8(a-d)). You will discover in the muscular system chapter that the associated muscles to these movements are flexor and extensor.
Abduction and Adduction
Abduction and adduction motions occur within the coronal plane and involve medial-lateral motions of the limbs, fingers, toes, or thumb. For example, abduction is raising the arm at the shoulder joint, moving it laterally away from the body, while adduction brings the arm down to the side of the body (see Figure 13.8(e)). In the muscular system chapter you will discover that the associated muscles to these movements are abductor and adductor.
Circumduction
Circumduction is the movement of a body region in a circular manner, in which one end of the body region being moved stays relatively stationary while the other end describes a circle. It involves the sequential combination of flexion, adduction, extension, and abduction at a joint (see Figure 13.8(e)).
Rotation
Rotation can occur within the vertebral column, at a pivot joint, or at a ball-and-socket joint. Rotation of the neck or body is the twisting movement produced by the summation of the small rotational movements available between adjacent vertebrae. At a pivot joint, one bone rotates in relation to another bone.
Rotation can also occur at the ball-and-socket joints of the shoulder and hip. Here, the humerus and femur rotate around their long axis, which moves the anterior surface of the arm or thigh either toward or away from the midline of the body (see see Figure 13.8(f)).
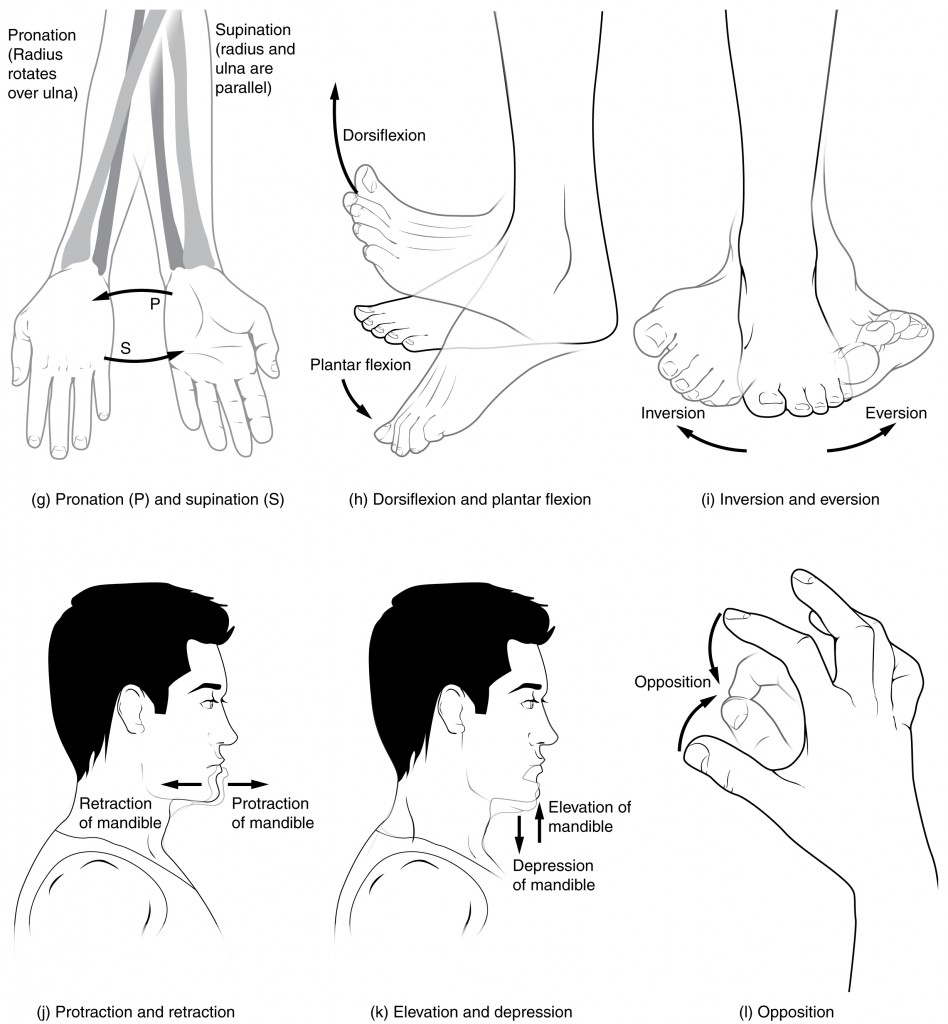
Supination and Pronation
Supination and pronation are movements of the forearm. In the anatomical position, the upper limb is held next to the body with the palm facing forward. This is the supinated position of the forearm. In this position, the radius and ulna are parallel to each other. When the palm of the hand faces backward, the forearm is in the pronated position, and the radius and ulna form an X-shape.
Pronation is the movement that allows the palm of the hand to face backward while in supination the palm of the hand faces forward. It helps to remember that supination is the motion you use when scooping up soup with a spoon (see Figure 13.9(g)).
Dorsiflexion and Plantar Flexion
Dorsiflexion and plantar flexion are movements at the ankle joint, which is a hinge joint. Lifting the front of the foot, so that the top of the foot moves (upward) toward the anterior leg is dorsiflexion, while lifting the heel of the foot from the ground or pointing the toes downward is plantar flexion. These are the only movements available at the ankle joint (see Figure 13.9(h)).
Inversion and Eversion
Inversion and eversion are complex movements that involve the multiple plane joints among the tarsal bones of the posterior foot (intertarsal joints) and thus are not motions that take place at the ankle joint. Inversion is the turning of the foot to angle the bottom of the foot toward the midline, while eversion turns the bottom of the foot away from the midline. The foot has a greater range of inversion than eversion motion. These are important motions that help to stabilize the foot when walking or running on an uneven surface and aid in the quick side-to-side changes in direction used during active sports such as basketball, racquetball, or soccer (see Figure 13.9(i)).
Protraction and Retraction
Protraction and retraction are anterior-posterior movements of the scapula or mandible. Protraction of the scapula occurs when the shoulder is moved forward, as when pushing against something or throwing a ball. Retraction is the opposite motion, with the scapula being pulled posteriorly and medially, toward the vertebral column. For the mandible, protraction occurs when the lower jaw is pushed forward, to stick out the chin, while retraction pulls the lower jaw backward (see Figure 13.9(j)).
Depression and Elevation
Depression and elevation are downward and upward movements of the scapula or mandible. The upward movement of the scapula and shoulder is elevation, while a downward movement is depression. These movements are used to shrug your shoulders. Similarly, elevation of the mandible is the upward movement of the lower jaw used to close the mouth or bite on something, and depression is the downward movement that produces opening of the mouth (see Figure 13.9(k)).
Concept Check
- Differentiate between pronation and supination.
Skeletal System Movement Terms
Medical Terms in Context
Common Skeletal System Abbreviations
Common Diseases and Disorders
Osteoporosis
Osteoporosis is a bone disease that causes bones to become weak and thin over time (National Osteoporosis Foundation, 2021). This weakness can lead to fractures from simple movements and occur often in the wrist, shoulder, spine, and hip. To learn more about osteoporosis please visit the National Osteoporosis Foundation website.
Arthritis
Arthritis often presents as edema , arthralgia, and ankylosis (Centers for Disease Control and Prevention, 2019). Common types of arthritis are osteoarthritis (OA), rheumatoid arthritis (RA), fibromyalgia, Gout and lupus. To learn more about arthritis visit the CDC’s Arthritis Basics web page.
Osteoarthritis
Osteoarthritis (OA) is the most common form of arthritis, and over 32.5 million US adults have been diagnosed with OA (Centers for Disease Control and Prevention, 2020b). The breakdown of cartilage and bone occurs over time when joints are exposed to heavy workloads either through occupation, obesity and/or prior injury to a joint. Common symptoms are pain, stiffness and aching that worsens over time. While there is no cure, symptoms can be managed through exercise, medications and in severe cases joint replacements (Centers for Disease Control and Prevention, 2020b).
Rheumatoid arthritis
The CDC describes rheumatoid arthritis (RA) as an autoimmune and inflammatory disease. Autoimmune diseases are disorders in which the immune system over reacts and begins to attack itself. In the case of RA inflammation to the joint tissues of the hands, wrists and knees is painful and debilitating. Treatments may include immunosuppressive drugs and anti-inflammatory drugs (Betts, et al., 2021). RA can also affect other tissues throughout the body and cause problems in organs such as the lungs, heart, and eyes. RA can affect children and in this case it is referred to as juvenile rheumatoid arthritis (Centers for Disease Control and Prevention, 2020c).
Gout
According to the Arthritis Society, gout is an inflammatory arthritis caused when the immune system attacks the crystals that form when uric acid builds up in a joint. Gout has periods of exacerbation and remission and is commonly treated through lifestyle changes and medication. While any joint can be effected it is common in the lower extremities and most often in the big toe (Choy & MacMullan, 2017). To learn more about the causes and treatments please visit the Arthritis Society’s web page about gout.
Myasthenia Gravis
The National Institute of Neurological Disorders and Strokes describes myasthenia gravis as a "chronic autoimmune neuromuscular disorder that causes weakness in the skeletal muscle” (Office of Communications and Public Liaison, 2020). To learn more, visit the National Institute of Neurological Disorders and Stroke’s Myasthenia Gravis fact sheet.
Fibromyalgia
Fibromyalgia is a challenging disease to diagnose since symptoms manifest differently and are similar to other diseases. Symptoms may include chronic fatigue, emotional and mental stress, headaches, and increased pain sensitivity. Currently, the cause of fibromyalgia has not been identified (Centers for Disease Control and Prevention, 2020a). To learn more about the diagnosis and treatment for fibromyalgia please visit the Centers for Disease Control and Prevention’s fibromyalgia web page.
Osteomyelitis
Osteomyelitis is a bone infection caused when staphylococcus bacteria travels through the blood stream from an infection in one part of the body to the bone. Staphylococcus bacteria is found on the skin and it can transfer to the bone through a wound and/or surgical contamination. The risk increases as people age or if their immune system is compromised (Mayo Clinic Staff, 2021). To learn more about the causes, symptoms and treatments for osteomyelitis please visit the Mayo Clinic’s osteomyelitis web page.
Disorders of the Curvature of the Spine
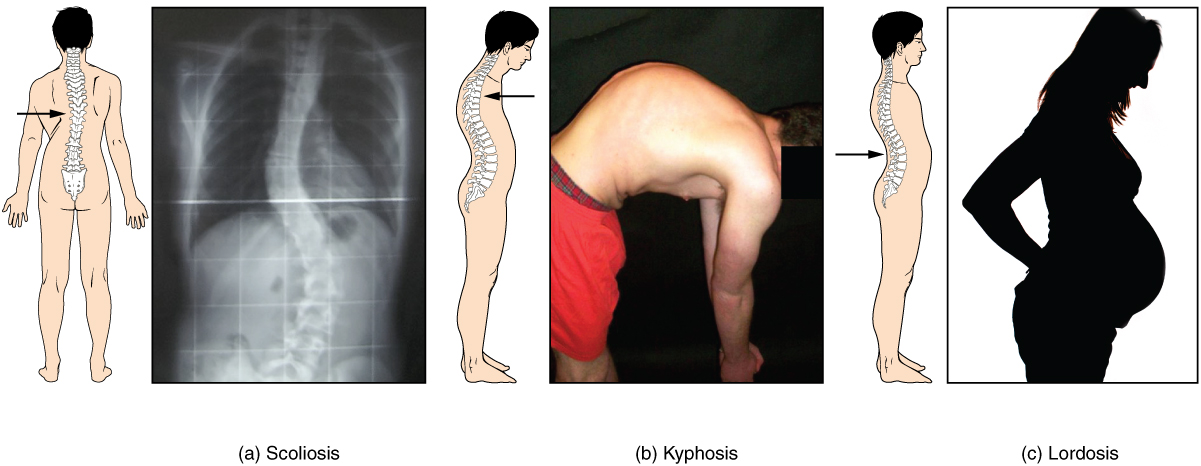
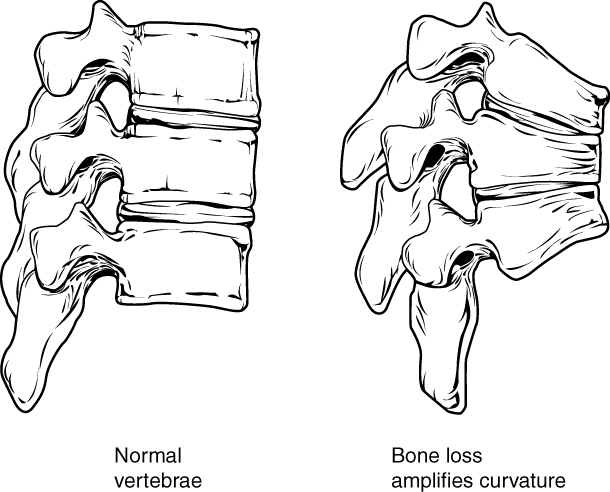
Developmental anomalies, pathological changes, or obesity can enhance the normal vertebral column curves, resulting in the development of abnormal or excessive curvatures (see Figure 13.10). Disorders associated with the curvature of the spine include:
- Kyphosis: Also referred to as humpback, is an excessive posterior curvature of the thoracic region. This can develop when osteoporosis causes weakening and erosion of the anterior portions of the upper thoracic vertebrae, resulting in their gradual collapse (see Figure 13.11).
- Lordosis: Also referred to as swayback, is an excessive anterior curvature of the lumbar region and is most commonly associated with obesity or late pregnancy. The accumulation of body weight in the abdominal region results an anterior shift in the line of gravity that carries the weight of the body. This causes in an anterior tilt of the pelvis and a pronounced enhancement of the lumbar curve.
- Scoliosis: An abnormal, lateral curvature, accompanied by twisting of the vertebral column. Scoliosis is the most common vertebral abnormality among girls. The cause is usually unknown, but it may result from weakness of the back muscles, defects such as differential growth rates in the right and left sides of the vertebral column, or differences in the length of the lower limbs. When present, scoliosis tends to get worse during adolescent growth spurts. Although most individuals do not require treatment, a back brace may be recommended for growing children. In extreme cases, surgery may be required (Betts, et al., 2021).
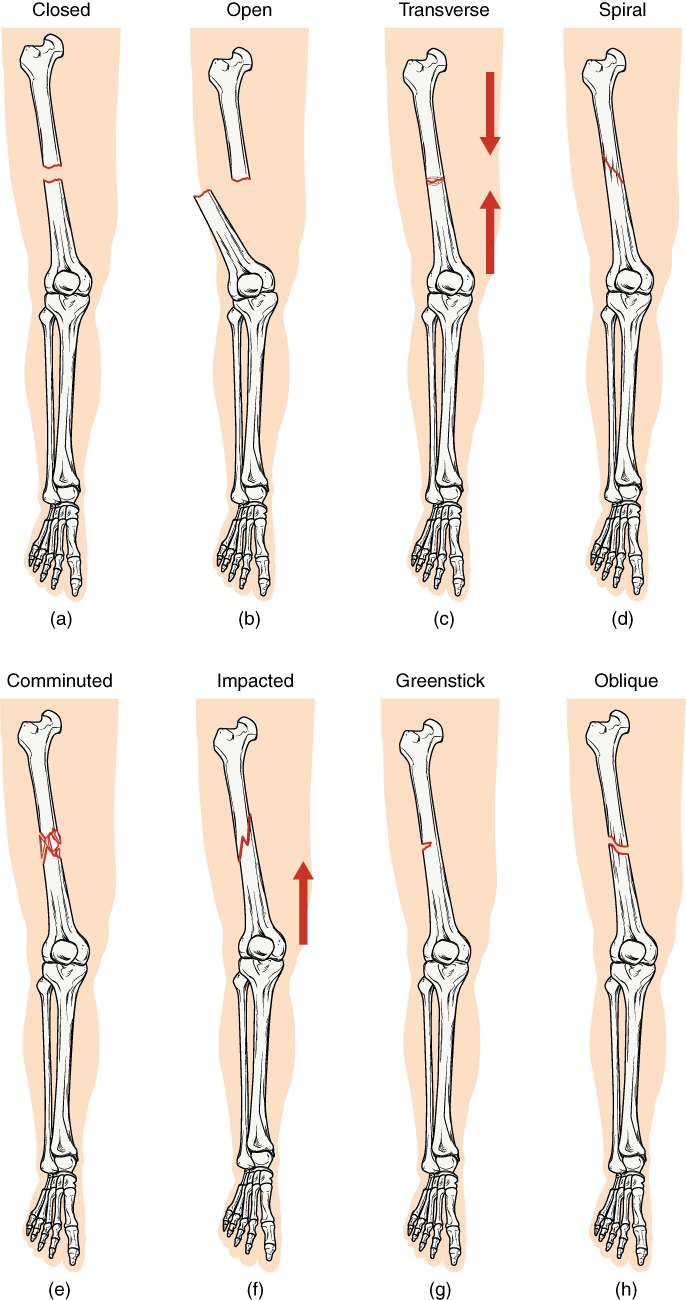
Fractures
A fracture is a broken bone. It will heal whether or not a physician resets it in its anatomical position. If the bone is not reset correctly, the healing process will keep the bone in its deformed position. Crepitation or crepitus is the creaking or popping sound that is heard when fractured bones move against each other Fractures are classified by their complexity, location, and other features (see Figure 13.12). Some fractures may be described using more than one term because it may have the features of more than one type (e.g., an open transverse fracture) (Betts, et al., 2021).
Types of fractures include:
- Closed or simple – bones are broken but does not protrude the skin
- Open or compound – bones are broken and pierce through the skin
- Transverse – bone is broken straight across
- Spiral – bone has twisted apart
- Comminuted – bones are broken and crushed into pieces
- Impacted – One fragment is driven into the other, usually as a result of compression
- Greenstick – bones are partially broken; occurs mainly in children
- Oblique – bones are broken at an angle
- Colles – bones are broken and occurs at the wrist or distal radius
- Stress – small crack in bone
Bone Cancer
There are three types of primary bone cancers: osteosarcoma, Ewing Sarcomas and chondrosarcoma. These are considered primary cancers because they originate in the bones. Osteosarcoma and Ewing Sarcomas are cancers found in children, teenagers, and young adults. Ewing Sarcomas is considered to be the more aggressive of the two cancers since it tends to metastasize quickly. Osteosarcoma is the most common type of bone cancer and it begins in the tissues of growing bones. Chondrosarcoma develops in cells that produce cartilage and affects adults (Mayo Clinic, 2021). To learn more, visit the Mayo Clinic web page on bone cancer.
Diagnostic Procedures
Common diagnostic procedures related specifically to the skeletal system include x-rays, bone mineral density testing, and arthroscopy.
- X-rays are common diagnostic tests used to confirm or rule out fractures and broken bones. The radiation dose is low so it is considered a safe diagnostic test (U.S. Food and Drug Administration, 2020).
- Dual x-ray absorptiometry (BMD), also called a bone mineral density test, is a test to determine osteoporosis by measuring the amount of bone mineral in a particular amount of bone (National Cancer Institute, 2021).
- Arthroscopy is a common procedure performed by orthopedic surgeons to view the inside of a joint to diagnose and/or to repair joint problems. The patient is given a local anesthetic and the surgeon inserts an arthroscope through an incision in the skin. Depending on what the surgeons finds, a repair of the joint may take place during the procedure (Mayo Clinic Staff, 2018a).
Medical Specialties Related to the Skeletal System
Orthopedic Surgeon
Orthopedic Surgeons are medical doctors who complete specialized training in the prevention, diagnosis, treatment and surgery of disorders and diseases related to the musculoskeletal systems (American Academy of Orthopedic Surgeons, 2021). For more details please visit the American Academy of Orthopaedic Surgeons’s page on Orthopaedic Surgeons.
Rheumatologist
Rheumatologists are medical doctors who have additional training as internists with a sub-specialty in rheumatology. Many rheumatology disorders have an underlying autoimmune disorders. Subsequently, rheumatologists are interested in autoimmune disorders and their impact on multiple body systems including the musculoskeletal systems (American College of Rheumatology 2018). For more details please follow the link to the American College of Rheumatology’s web page called ‘What is a Rheumatologist?’
Doctor of Chiropractic (DC)/Chiropractor
A Doctor of Chiropractic (DC) completes a four-year doctoral graduate school program with at least 4,200 hours of clinical experience, and laboratory and course work. Chiropractors are trained in the prevention, assessment and treatment of the spine, muscular system and nervous system. Chiropractors focus on spinal adjustments, nutrition, and preventing injury without the use of pharmaceuticals or surgical procedures (American Chiropractic Association, 2021). To learn more visit the American Chiropractic Association website.
Physiotherapist
A physiotherapist has a Doctoral of Physical Therapy degree and has successfully completed the National Physical Therapy Examination. Physiotherapists use an evidenced-based approach when assessing and designing treatment plans for their clients. Treatments may include exercises, massage, joint manipulation, and occupational retraining (U.S. Bureau of Labor Statistics, 2021). To learn more please visit the U.S. Bureau of Labor Statistics web page on physical therapists.
Occupational Therapist
Occupational therapist helps people across the lifespan to do the things they want and need to do through the therapeutic use of daily activities (occupations). Occupational therapy practitioners enable people of all ages to live life to its fullest by helping them promote health, and prevent—or live better with—injury, illness, or disability. To learn more please visit the American Occupational Therapy Association webpage.
Certified Occupational Therapy Assistant
Certified occupational therapy assistants and aides help patients develop, recover, improve, as well as maintain the skills needed for daily living and working. To learn more please visit the Occupational Outlook Handbook: Occupational Therapy Assistants and Aides.
Physical Therapist
Physical therapists help people to maximize their quality of life. They work with people of all ages and abilities, and in a variety of settings. They help people rehabilitate from devastating injuries, manage chronic conditions, avoid surgery and prescription drugs, and create healthy habits. To learn more please visit: American Physical Therapy Association
Physical Therapist Assistants
Assist physical therapists in providing physical therapy treatments and procedures. May, in accordance with state laws, assist in the development of treatment plans, carry out routine functions, document the progress of treatment, and modify specific treatments in accordance with patient status and within the scope of treatment plans established by a physical therapist. Generally requires formal training. To learn more please visit: Physical Therapist Assistants
Test Yourself
References
American Academy of Orthopaedic Surgeons. (2021). Orthopaedic Surgeons: Restoring mobility and keeping our nation in motion. https://www.aaos.org/about/what-is-an-orthopaedic-surgeon/
American Chiropractic Association. (2021). Key Facts and Figures About the Chiropractic Profession. https://www.acatoday.org/News-Publications/Newsroom/Key-Facts
American College of Rheumatology. (2018). What is a Rheumatologist? https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Health-Care-Team/What-is-a-Rheumatologist
American Occupational Therapy Association. (2021).What is Occupational Therapy. https://www.aota.org/conference-events/otmonth/what-is-ot.aspx
American Physical Therapy Association. (2021). Careers in Physical Therapy. https://www.apta.org/your-career/careers-in-physical-therapy
Centers for Disease Control and Prevention. (2019). Arthritis basics. CDC Arthritis Program. https://www.cdc.gov/arthritis/basics/index.html
Centers for Disease Control and Prevention. (2020a). Fibromyalgia. CDC Arthritis Program. https://www.cdc.gov/arthritis/basics/fibromyalgia.htm
Centers for Disease Control and Prevention. (2020b). Osteoarthritis (OA). CDC Arthritis Program. https://www.cdc.gov/arthritis/basics/osteoarthritis.htm
Centers for Disease Control and Prevention. (2020c). Rheumatoid arthritis. CDC Arthritis Program. https://www.cdc.gov/arthritis/basics/rheumatoid-arthritis.html
Choy, G., & MacMullan, P. (2017). Gout. Arthritis Society. https://arthritis.ca/about-arthritis/arthritis-types-(a-z)/types/gout
Mayo Clinic Staff. (2018). Osteomyelitis. Mayo Clinic Patient Care and Health Information. https://www.mayoclinic.org/diseases-conditions/osteomyelitis/symptoms-causes/syc-20375913
Mayo Clinic Staff. (2018a). Arthroscopy. Mayo Clinic Patient Care and Health Information. https://www.mayoclinic.org/tests-procedures/arthroscopy/about/pac-20392974
Mayo Clinic Staff. (2021). Bone Cancer. Mayo Clinic Patient Care and Health Information. https://www.mayoclinic.org/diseases-conditions/bone-cancer/symptoms-causes/syc-20350217
National Osteoporosis Foundation. (2021). What is osteoporosis and what causes it? https://www.nof.org/patients/what-is-osteoporosis/
Occupational Therapy Assistants and Aides. (Sept 2021). Occupational Outlook Handbook. https://www.bls.gov/ooh/healthcare/occupational-therapy-assistants-and-aides.htm
Office of Communications and Public Liaison. (2020). Myasthenia gravis fact sheet. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Myasthenia-Gravis-Fact-Sheet
National Cancer Institute. Dual x-ray absorptiometry. National Institutes of Health. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/dual-x-ray-absorptiometry
U.S. Bureau of Labor Statistics. (2021). Occupational Therapists. https://www.bls.gov/ooh/healthcare/physical-therapists.htm#tab-1
U.S. Bureau of Labor Statistics. (2021). Physical Therapist Assistants. https://www.bls.gov/oes/current/oes312021.htm#nat
U.S. Food and Drug Administration. (2020). Medical X-ray Imaging. https://www.fda.gov/radiation-emitting-products/medical-imaging/medical-x-ray-imaging
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.
The process in which the body produces blood.
Also known as joints, where bones meet bones or where bones meet cartilage
away from the midline of the body
Movement toward the midline of the body
abnormal condition of bones that are porous.
Inflammation of the joints
swelling
painful joint(s)
abnormal condition of stiffness
Inflammation of bones and joints
pain in the fibrous tissues of muscles
increase in severity of a problem
grave or serious muscle weakness
a condition that lasts a long time with periods of remission and exacerbation
Production of cells that can mobilize and establish tumors in other organs of the body
Instrument that contains a small camera on a tube with a light. This is a tool used to view the inside of a joint.

