12 Digestive System
WTCS Learning Objectives
- Apply the rules of medical language to build, analyze, spell, pronounce, abbreviate, and define terms as they relate to the digestive system
- Identify meanings of key word components of the digestive system
- Categorize diagnostic, therapeutic, procedural or anatomic terms related to the digestive system
- Use terms related to the digestive system
- Use terms related to the diseases and disorders of the digestive system
Digestive System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Digestive System.
Introduction to the Digestive System
The digestive system is continually at work, yet people seldom appreciate the complex tasks it performs in a choreographed biologic symphony. Consider what happens when you eat an apple. Of course, you enjoy the apple’s taste as you chew it, but in the hours that follow, unless something goes amiss and you get a stomachache, you don’t notice that your digestive system is working. You may be taking a walk or studying or sleeping, having forgotten all about the apple, but your stomach and intestines are busy digesting it and absorbing its vitamins and other nutrients. By the time any waste material is excreted, the body has appropriated all it can use from the apple. In short, whether you pay attention or not, the organs of the digestive system perform their specific functions, allowing you to use the food you eat to keep you going.
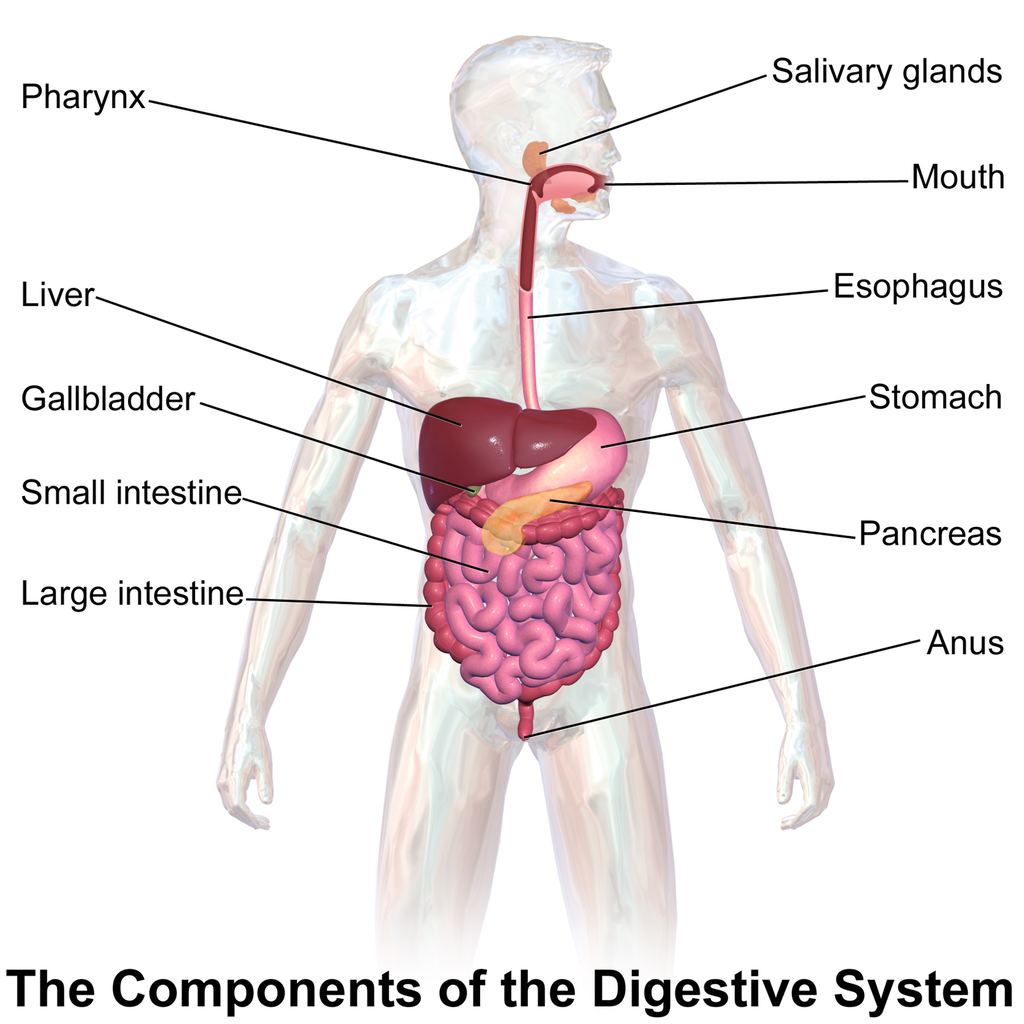
This chapter examines the structure and functions of these organs, and explores the mechanics and chemistry of the digestive processes. The function of the digestive system is to break down the foods you eat, release their nutrients, and absorb those nutrients into the body. Although the small intestine is the workhorse of the system, where the majority of digestion occurs, and where most of the released nutrients are absorbed into the blood or lymph, each of the digestive system organs makes a vital contribution to this process (see Figure 12.1).
Watch this video:
Media 12.1 How your digestive system works – Emma Bryce. Copyright 2017 by Ted-Ed.
Digestive System Medical Terms
Now that you have memorized the word parts see if you can break down the following Digestive terms and define them.
Practice with this activity:
Anatomy (Structures) of the Digestive System
The Mouth
also called the oral cavity (or buccal cavity). The structures of the mouth are illustrated in Figure 12.2.
The pocket-like part of the mouth that is framed on the inside by the gums and teeth, and on the outside by the cheeks and lips is called the oral vestibule. The main open area of the mouth, or oral cavity proper, runs from the gums and teeth to the fauces.
When you are chewing, you do not find it difficult to breathe simultaneously. The next time you have food in your mouth, notice how the arched shape of the roof of your mouth allows you to handle both digestion and respiration at the same time. This arch is called the palate. The anterior region of the palate serves as a wall (or septum) between the oral and nasal cavities as well as a rigid shelf against which the tongue can push food. It is created by the maxillary and palatine bones of the skull and, given its bony structure, is known as the hard palate. If you run your tongue along the roof of your mouth, you’ll notice that the hard palate ends in the posterior oral cavity, and the tissue becomes fleshier. This part of the palate, known as the soft palate, is composed mainly of skeletal muscle. You can therefore manipulate, subconsciously, the soft palate—for instance, to yawn, swallow, or sing (see Figure 12.2).
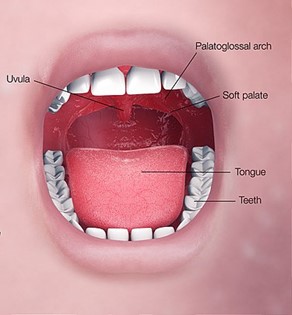
A fleshy bead of tissue called the uvula drops down from the center of the posterior edge of the soft palate. Although some have suggested that the uvula is a vestigial organ, it serves an important purpose. When you swallow, the soft palate and uvula move upward, helping to keep foods and liquid from entering the nasal cavity. Unfortunately, it can also contribute to the sound produced by snoring. Two muscular folds extend downward from the soft palate, on either side of the uvula. Between these two folds are the palatine tonsils, clusters of lymphoid tissue that protect the pharynx. The lingual tonsils are located at the base of the tongue.
Tongue
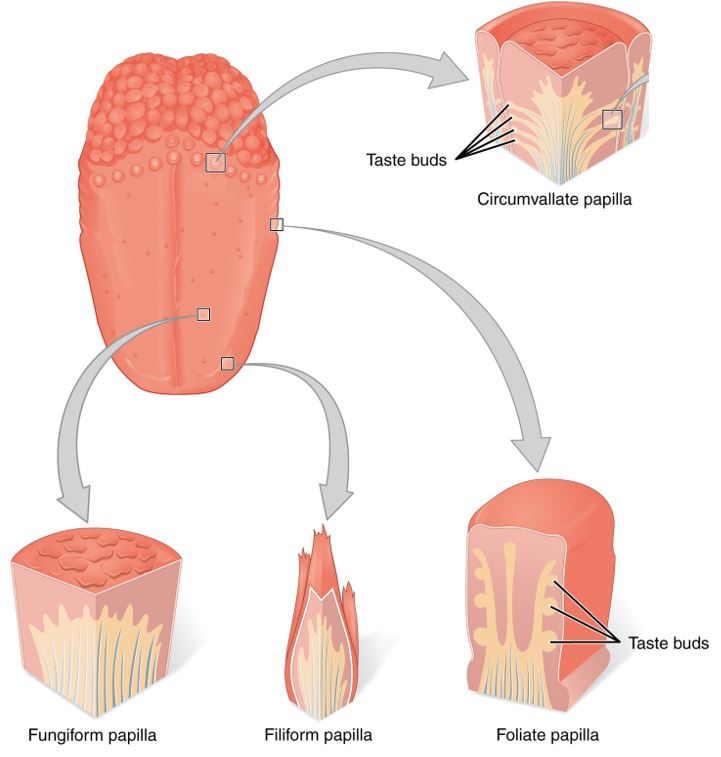
Perhaps you have heard it said that the tongue is the strongest muscle in the body. Those who stake this claim cite its strength proportionate to its size. Although it is difficult to quantify the relative strength of different muscles, it remains indisputable that the tongue is a workhorse, facilitating ingestion, mechanical digestion, chemical digestion (lingual lipase), sensation (of taste, texture, and temperature of food), swallowing, and vocalization.
The top and sides of the tongue are studded with papillae (see Figure 12.3).
Salivary Glands
Many small salivary glands are housed within the mucous membranes of the mouth and tongue. These minor exocrine glands are constantly secreting saliva, either directly into the oral cavity or indirectly through ducts, even while you sleep. In fact, an average of 1 to 1.5 liters of saliva is secreted each day. Usually just enough saliva is present to moisten the mouth and teeth. Secretion increases when you eat, because saliva is essential to moisten food and initiate the chemical breakdown of carbohydrates. Small amounts of saliva are also secreted by the labial glands in the lips. In addition, the buccal glands in the cheeks, palatal glands in the palate, and lingual glands in the tongue help ensure that all areas of the mouth are supplied with adequate saliva.
Concept Check
- Describe how the anatomy of the mouth permits breathing and chewing at the same time
- Explain the role saliva performs in the digestive system
Pharynx
The pharynx (throat) is involved in both digestion and respiration. It receives food and air from the mouth, and air from the nasal cavities. When food enters the pharynx, involuntary muscle contractions close off the air passageways. A short tube of skeletal muscle lined with a mucous membrane, the pharynx runs from the posterior oral and nasal cavities to the opening of the esophagus and larynx. It has three subdivisions. The most superior, the nasopharynx, is involved only in breathing and speech. The other two subdivisions, the oropharynx and the laryngopharynx, are used for both breathing and digestion. The oropharynx begins inferior to the nasopharynx and is continuous below with the laryngopharynx. The inferior border of the laryngopharynx connects to the esophagus, whereas the anterior portion connects to the larynx, allowing air to flow into the bronchial tree.
Esophagus
The esophagus is a muscular tube that connects the pharynx to the stomach. It is approximately 25.4 cm (10 in) in length, located posterior to the trachea, and remains in a collapsed form when not engaged in swallowing. As you can see in Figure 12.4, the esophagus runs a mainly straight route through the mediastinum of the thorax. To enter the abdomen, the esophagus penetrates the diaphragm through an opening called the esophageal hiatus.
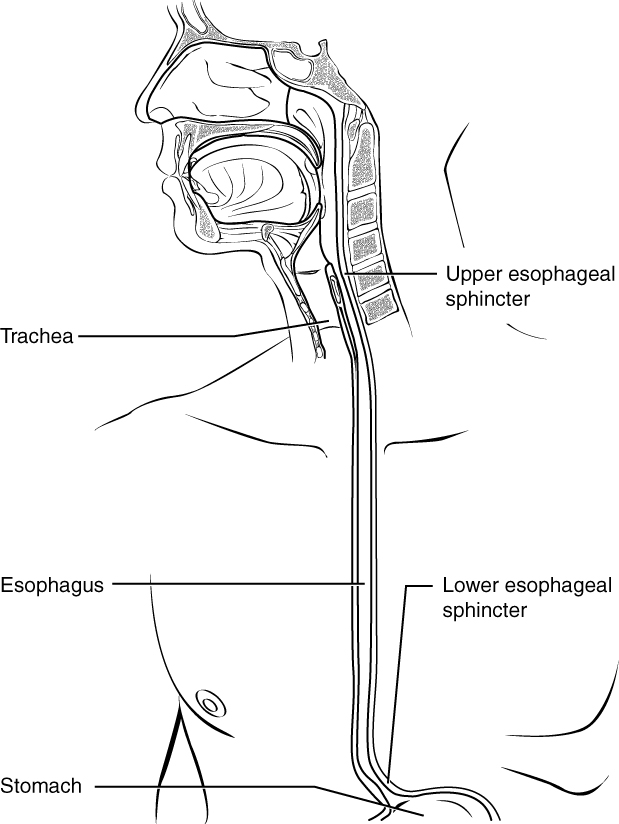
Passage of Food Through the Esophagus
The upper esophageal sphincter, controls the movement of food from the pharynx into the esophagus. The upper two-thirds of the esophagus consists of both smooth and skeletal muscle fibers. A series of contractions called peristalsis push food through the esophagus and into the stomach. Just before the opening to the stomach is an important ring-shaped muscle called the lower esophageal sphincter (LES). Recall that sphincters are muscles that surround tubes and serve as valves, closing the tube when the sphincters contract and opening it when they relax. This sphincter opens to let food pass into the stomach and closes to keep it there.
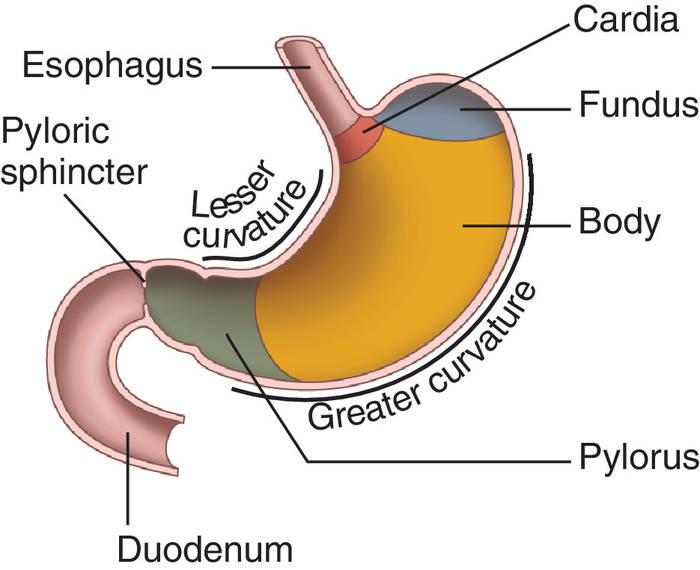
Stomach
There are four main regions in the stomach: the cardia, fundus, body, and pylorus (see Figure 12.5). The cardia (or cardiac region) is the point where the esophagus connects to the stomach and through which food passes into the stomach. Located inferior to the diaphragm, above and to the left of the cardia, is the dome-shaped fundus. Below the fundus is the body, the main part of the stomach. The funnel-shaped pylorus connects the stomach to the duodenum.
Small Intestines
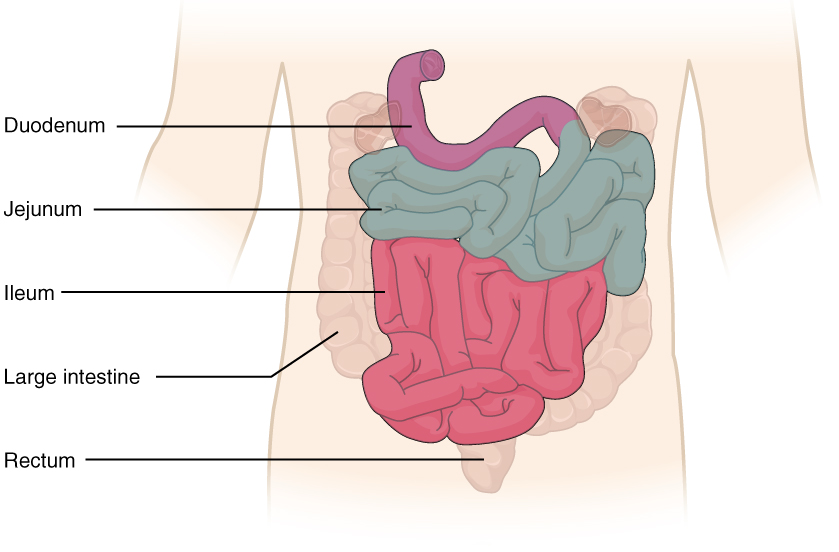
Chyme released from the stomach enters the small intestine, which is the primary digestive organ in the body. Not only is this where most digestion occurs, it is also where practically all absorption occurs. The longest part of the alimentary canal, the small intestine is about 3.05 meters (10 feet) long in a living person (but about twice as long in a cadaver due to the loss of muscle tone). Since this makes it about five times longer than the large intestine, you might wonder why it is called “small.” In fact, its name derives from its relatively smaller diameter of only about 2.54 cm (1 in), compared with 7.62 cm (3 in) for the large intestine. As we’ll see shortly, in addition to its length, the folds and projections of the lining of the small intestine work to give it an enormous surface area, more than 100 times the surface area of your skin. This large surface area is necessary for complex processes of digestion and absorption that occur within it.
The coiled tube of the small intestine is subdivided into three regions. From proximal (at the stomach) to distal, these are the duodenum, jejunum, and ileum (see Figure 12.6).
Large Intestines
The large intestine is the terminal part of the alimentary canal. The primary function of this organ is to finish absorption of nutrients and water, synthesize certain vitamins, form feces, and eliminate feces from the body.
The large intestine runs from the appendix to the anus. It frames the small intestine on three sides. Despite its being about one-half as long as the small intestine, it is called large because it is more than twice the diameter of the small intestine, about 3 inches.
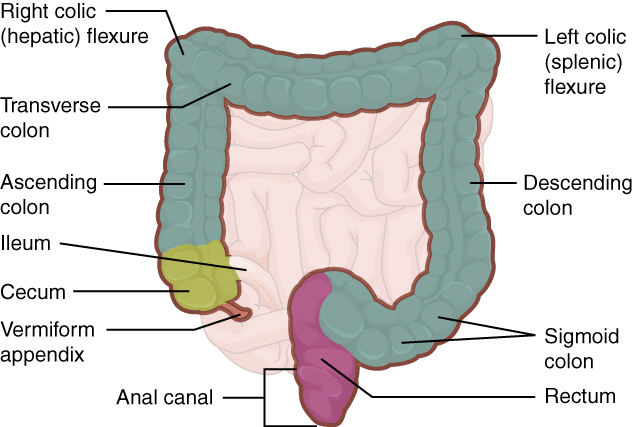
Cecum
The first part of the large intestine is the cecum, a sac-like structure that is suspended inferior to the ileocecal valve. It is about 6 cm (2.4 in) long, receives the contents of the ileum, and continues the absorption of water and salts. The appendix (or vermiform appendix) is a winding tube that attaches to the cecum. Although the 7.6-cm (3-in) long appendix contains lymphoid tissue, suggesting an immunologic function, this organ is generally considered vestigial. However, at least one recent report assumes a survival advantage conferred by the appendix: In diarrheal illness, the appendix may serve as a bacterial reservoir to repopulate the enteric bacteria for those surviving the initial phases of the illness. Moreover, its twisted anatomy provides a haven for the accumulation and multiplication of enteric bacteria.
Colon
The cecum blends seamlessly with the colon. Upon entering the colon, the food residue first travels up the ascending colon on the right side of the abdomen. At the inferior surface of the liver, the colon bends to become the transverse colon. The region defined as hindgut begins with the last third of the transverse colon and continues on. Food residue passing through the transverse colon travels across to the left side of the abdomen. From there, food residue passes through the descending colon, which runs down the left side of the posterior abdominal wall. After entering the pelvis inferiorly, it becomes the s-shaped sigmoid colon, which extends medially to the midline (see Figure 12.7). The ascending and descending colon, and the rectum (discussed next) are located in the retroperitoneum.
Accessory Organs of Digestion
Chemical digestion in the small intestine relies on the activities of three accessory digestive organs: the liver, pancreas, and gallbladder (see Figure 12.8). The digestive role of the liver is to produce bile and export it to the duodenum. The gallbladder primarily stores, concentrates, and releases bile. The pancreas produces pancreatic juice, which contains digestive enzymes and bicarbonate ions, and delivers it to the duodenum.
Concept Check
On the Figure 12.8 diagram locate the following anatomical organs and consider how these organs support the digestive process
- Liver
- Pancreas
- Gallbladder
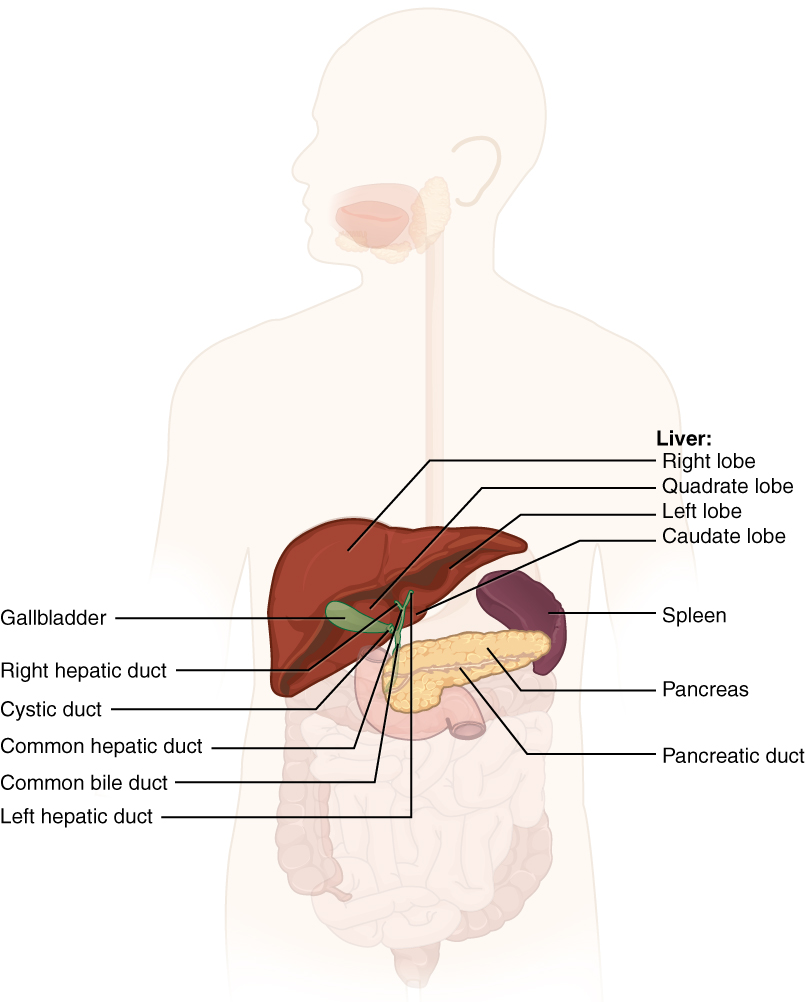
Liver
The liver is the largest gland in the body, weighing about three pounds in an adult. It is also one of the most important organs. In addition to being an accessory digestive organ, it plays a number of roles in metabolism and regulation. The liver lies inferior to the diaphragm in the right upper quadrant of the abdominal cavity and receives protection from the surrounding ribs. The liver is divided into two primary lobes: a large right lobe and a much smaller left lobe.
The hepatic portal vein delivers partially deoxygenated blood containing nutrients absorbed from the small intestine and actually supplies more oxygen to the liver than do the much smaller hepatic arteries. In addition to nutrients, drugs and toxins are also absorbed. After processing the bloodborne nutrients and toxins, the liver releases nutrients needed by other cells back into the blood, which drains into the central vein and then through the hepatic vein to the inferior vena cava. With this hepatic portal circulation, all blood from the alimentary canal passes through the liver. This largely explains why the liver is the most common site for the metastasis of cancers that originate in the alimentary canal.
Bile produced by the liver is a mixture secreted by the liver to accomplish the emulsification of lipids in the small intestine.
Bilirubin, the main bile pigment, is a waste product produced when the spleen removes old or damaged red blood cells from the circulation. These breakdown products, including proteins, iron, and toxic bilirubin, are transported to the liver via the splenic vein of the hepatic portal system. In the liver, proteins and iron are recycled, whereas bilirubin is excreted in the bile. It accounts for the green color of bile. Bilirubin is eventually transformed by intestinal bacteria into stercobilin, a brown pigment that gives your stool its characteristic color! In some disease states, bile does not enter the intestine, resulting in white (‘acholic’) stool with a high fat content, since virtually no fats are broken down or absorbed.
Between meals, bile is produced but conserved. The valve-like hepatopancreatic ampulla closes, allowing bile to divert to the gallbladder, where it is concentrated and stored until the next meal.
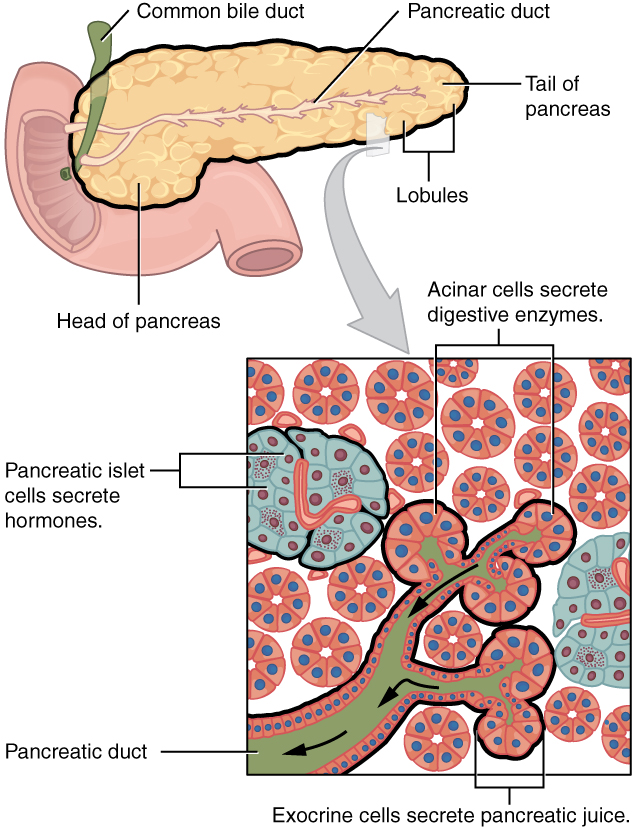
Pancreas
The soft, oblong, glandular pancreas lies transversely in the retroperitoneum behind the stomach. Its head is nestled into the “c-shaped” curvature of the duodenum with the body extending to the left about 15.2 cm (6 in) and ending as a tapering tail in the hilum of the spleen. It is a curious mix of exocrine (secreting digestive enzymes) and endocrine (releasing hormones into the blood) functions (Figure 12.9).
Gallbladder
The gallbladder is 8–10 cm (~3–4 in) long and is nested in a shallow area on the posterior aspect of the right lobe of the liver. This muscular sac stores, concentrates, and, when stimulated, propels the bile into the duodenum via the common bile duct. It is divided into three regions. The fundus is the widest portion and tapers medially into the body, which in turn narrows to become the neck.
Anatomy Labeling Activity
Physiology (Function) of the Digestive System
The main functions of the digestive system are:
- Ingesting food
- Digesting food
- Absorbing nutrients
- Elimination of waste products
Digestive Processes
The processes of digestion include six activities: ingestion, propulsion, mechanical or physical digestion, chemical digestion, absorption, and defecation.
The first of these processes, ingestion, refers to the entry of food into the alimentary canal through the mouth. There, the food is chewed and mixed with saliva, which contains enzymes that begin breaking down the carbohydrates in the food plus some lipid digestion via lingual lipase. Chewing increases the surface area of the food and allows an appropriately sized bolus to be produced.
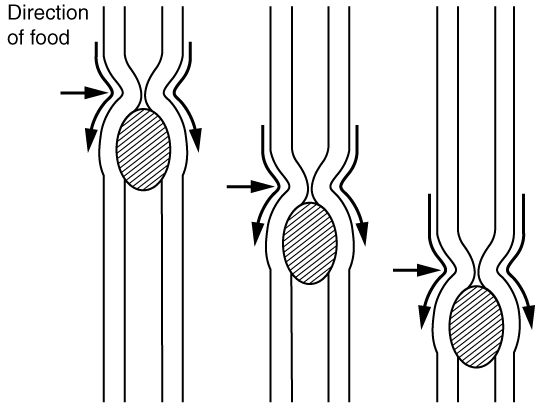
Food leaves the mouth when the tongue and pharyngeal muscles propel it into the esophagus. This act of swallowing, the last voluntary act until defecation, is an example of propulsion, which refers to the movement of food through the digestive tract. It includes both the voluntary process of swallowing and the involuntary process of peristalsis. Peristalsis consists of sequential, alternating waves of contraction and relaxation of alimentary wall smooth muscles, which act to propel food along (see Figure 12.10). These waves also play a role in mixing food with digestive juices. Peristalsis is so powerful that foods and liquids you swallow enter your stomach even if you are standing on your head.
Digestion includes both mechanical and chemical processes. Mechanical digestion is a purely physical process that does not change the chemical nature of the food. Instead, it makes the food smaller to increase both surface area and mobility. It includes mastication, or chewing, as well as tongue movements that help break food into smaller bits and mix food with saliva. Although there may be a tendency to think that mechanical digestion is limited to the first steps of the digestive process, it occurs after the food leaves the mouth, as well. The mechanical churning of food in the stomach serves to further break it apart and expose more of its surface area to digestive juices, creating an acidic “soup” called chyme.
In chemical digestion, starting in the mouth, digestive secretions break down complex food molecules into their chemical building blocks (for example, proteins into separate amino acids). These secretions vary in composition, but typically contain water, various enzymes, acids, and salts. The process is completed in the small intestine.
Food that has been broken down is of no value to the body unless it enters the bloodstream and its nutrients are put to work. This occurs through the process of absorption, which takes place primarily within the small intestine.
In defecation, the final step in digestion, undigested materials are removed from the body as feces.
Digestive System: From Appetite Suppression to Constipation
Age-related changes in the digestive system begin in the mouth and can affect virtually every aspect of the digestive system. Taste buds become less sensitive, so food isn’t as appetizing as it once was. A slice of pizza is a challenge, not a treat, when you have lost teeth, your gums are diseased, and your salivary glands aren’t producing enough saliva. Swallowing can be difficult, and ingested food moves slowly through the alimentary canal because of reduced strength and tone of muscular tissue.
Pathologies that affect the digestive organs—such as hiatal hernia, gastritis, and peptic ulcer disease—can occur at greater frequencies as you age. Problems in the small intestine may include duodenal ulcers, maldigestion, and malabsorption. Problems in the large intestine include hemorrhoids, diverticular disease, and constipation. Conditions that affect the function of accessory organs—and their abilities to deliver pancreatic enzymes and bile to the small intestine—include jaundice, acute pancreatitis, cirrhosis, and gallstones.
In some cases, a single organ is in charge of a digestive process. For example, ingestion occurs only in the mouth and defecation only in the anus. However, most digestive processes involve the interaction of several organs and occur gradually as food moves through the alimentary canal (see Figure 12.11).
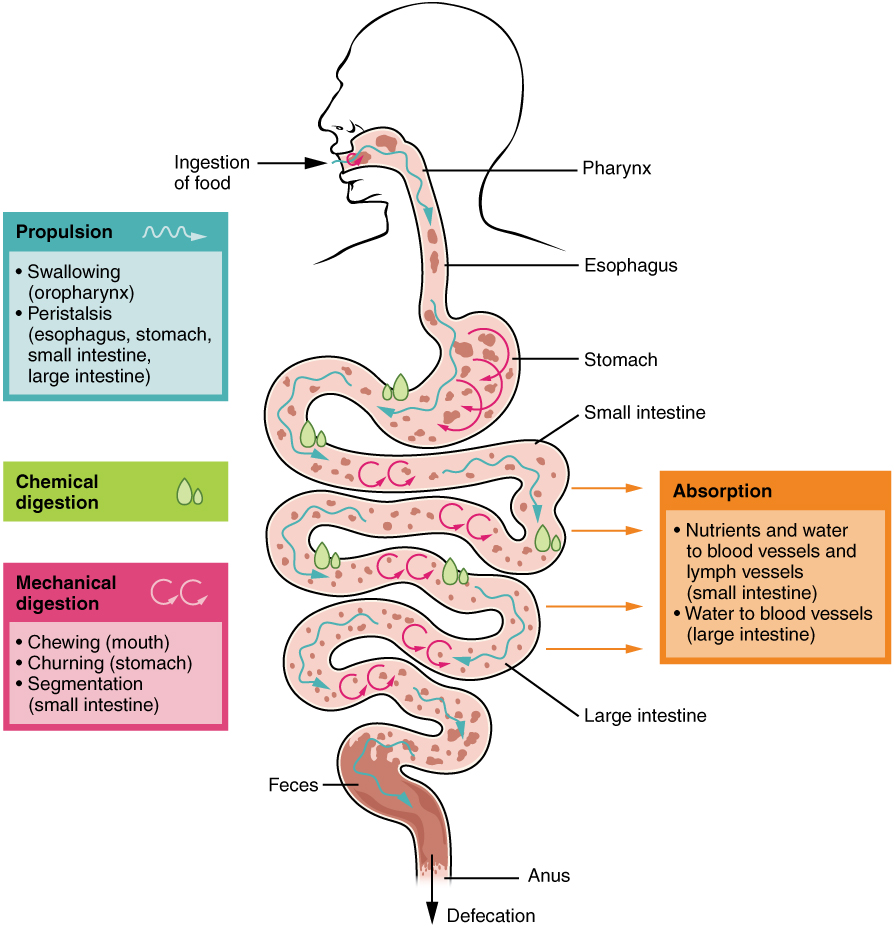
Some chemical digestion occurs in the mouth. Some absorption can occur in the mouth and stomach, for example, alcohol and aspirin.
Medical Terms not Easily Broken into Word Parts
Common Digestive Abbreviations
Diseases and Disorders of the Digestive System
Gastroesophageal Reflux Disease
This condition is largely caused by gastric acid flowing upwards from the stomach into the esophagus. Those suffering from the condition will often feel a burning sensation radiating near the top of the stomach. (Mayo Clinic Staff, 2020). To learn more about GERD visit the Mayo Clinic’s Gastroesophageal Reflux Disease (GERD) page.
Cholecystitis
This condition is known as inflammation of the gall bladder. Gall stone development can block the gall bladder’s release of bile leading to an inflammatory response. Surgical removal (cholecystectomy) or laser stone crushing known as lithotripsy are often the treatment options (“Cholecystitis”, 2019). To learn more about cholecystitis visit the Radiology Info’s cholecystitis web page.
Cirrhosis
Cirrhosis is condition whereby the liver scars. Advanced cirrhosis is life threatening. It generally can not be reversed. It is caused by different forms of liver disease and chronic alcoholism. (Mayo Clinic Staff, 2018).
Cirrhosis often has no signs or symptoms until liver damage is extensive and may include:
-
-
- Fatigue
- Easily bleeding or bruising
- Loss of appetite
- Nausea
- Edema
- Weight loss
- Itchy skin
- Jaundice
- Ascitis (Mayo Clinic Staff, 2018)
-
To learn more about Cirrhosis visit the Mayo Clinic’s Cirrohsis web page .
Esophageal Cancer
This is cancer of the esophagus. The cancer can occur anywhere along the esophageal tube, and can be caused by factors including tobacco use, alcohol, and chronic acid reflux (American Cancer Society medical and editorial team, 2020a). To learn more about esophageal cancer, visit the American Cancer Society’s Esophageal Cancer web page.
Hepatitis A, B and C
Inflammation of the liver is referred to as hepatitis. This condition can by caused by several factors such as viruses, alcohol consumption, toxins, and drug interactions. In some cases it can also be caused by an autoimmune response in the body. There are five types of viral hepatitis, A, B, C, D, and E (Booth, 2018). To learn more, visit Healthline’s article on Hepatitis.
Celiac Sprue (Celiac Disease)
Individuals who posses celiac disease have an immune sensitivity reaction occurring in the small intestines when they consume gluten. Typically people with this condition are genetically pre-disposed to the condition. Damage to the small intestine will occur if continued consumption of gluten occurs. Individuals once diagnosed eat a gluten free diet as a best approach for management of the condition. (Celiac Disease Foundation, n.d.). To learn more, visit the Celiac Disease Foundation’s What is Celiac Disease? article .
Crohn’s Disease and Ulcerative Colitis
Crohn’s disease and ulcerative colitis are chronic inflammatory bowel diseases (IBD) whereby a section or segments of the digestive tract experience inflammation. Crohn’s disease can occur anywhere along the digestive tract from the mouth to the anus, although it is most often found in the small intestines. This often leads to malabsorption of nutrients from food. Ulcerative colitis is localized inflammation and ulcers in the colon (UCLA Health, n.d.). To learn more, visit UCLA Health’s page about inflammatory bowel diseases.
Colon Cancer
Cancer formation in the colon portion of the digestive tract. It is typically found in older adults. Colon cancer is often diagnosed through a colonoscopy. (American Cancer Society medical and editorial team, 2020b). To learn more, visit the American Cancer Society’s page on colon cancer.
Hernia
A hernia occurs when an organ or fatty tissue squeezes through a weak spot in a surrounding muscle or connective tissue. A hiatal hernia is found in the upper stomach region.
Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is a common disorder affecting the large intestines. IBS often involves abdominal pain as sensitive nerve tissue within the colon react to movement of food and waste through the digestive tract. Along with the abdominal pain individuals often experience gas and bloating. Diet and lifestyle modifications often help in the management of the condition. (American College of Gastroenterology, 2021a). To learn more about irritable bowel syndrome, visit the American College of Gastroenterology’s web page on IBS.
Polyps
A polyp is a small growth of tissue protruding outward from the intestinal wall. Some cancers in the intestines start off as a polyp. Typically, they are found in people over the age of 50. Polyps start as a small collection of cells found within the colon. Most are harmless but can transition over time into a cancerous growth (Mayo Clinic Staff, 2019). To learn more about polyps review the Mayo Clinic’s patient information page on polyps.
Medical Terms in Context
Medical Specialties and Procedures Related to the Digestive System
Gastroenterology
This specialty is focused on the diagnosis and treatment of conditions afflicting the digestive system. Gastroenterology is a branch of internal medicine. A physician who specializes in this area is known as a gastroenterologist. (American College of Gastroenterology, 2021b). To learn more about gastroenterology visit the American College of Gastroenterology’s profile page.
Procedures
Upper and Lower Gastrointestinal Series
This is a diagnostic a procedure involving the introduction of a contrast medium known as barium. Barium can be introduced by ingesting or by enema. After induction of the barium, x-rays can be taken of the upper and lower gastrointestinal system structures (Johns Hopkins Medicine, 2020). To learn more, visit Johns Hopkins Medicine’s web page on barium x-rays.
Fecal Occult Blood Test
This is a test for hidden blood in a fecal sample. A patient is provided with a card to place a small segment of fecal output on. The sample is viewed under a microscope to look for blood. Blood detection can be an indicator of an abnormal growth occurring in the intestines (Johns Hopkins Medicine, 2020a).
Stool Culture
This procedure involves the collection of a small sample of feces which is analyzed for abnormal bacterial growth through a culture check (Johns Hopkins Medicine, 2020a).
Esophagogastroduodenoscopy
An EGD (upper endoscopy) is a procedure by which a physician examines the upper gastrointestinal tract (esophagus, stomach, duodenum) using a special instrument called an endoscope. The physician examines the tissues and is able to take a biopsy, if needed. (Johns Hopkins Medicine, 2020a.)
Test Yourself
References
American Cancer Society medial and editorial content team. (2020a). What is Cancer of the Esophagus? American Cancer Society, Inc. https://www.cancer.org/cancer/esophagus-cancer/about/what-is-cancer-of-the-esophagus.html
American Cancer Society medial and editorial content team. (2020b). What is Colorectal Cancer? American Cancer Society, Inc. https://www.cancer.org/cancer/colon-rectal-cancer/about/what-is-colorectal-cancer.html
American College of Gastroenterology. (2021a). Irritable bowel syndrome. https://gi.org/topics/irritable-bowel-syndrome/#tabs1
American College of Gastroenterology. (2021b). What is Gastroenterology? https://gi.org/patients/gi-health-and-disease/what-is-a-gastroenterologist/
Booth, S. (2018, August 13). Everything you need to know about hepatitis A, B, C, D, E. Healthline. https://www.healthline.com/health-news/everything-you-need-to-know-about-hepatitis#1
Celiac Disease Foundation. (n.d.) What is celiac disease?. Available from: https://celiac.org
“Cholecystitis”. (2019, January 15). Radiologyinfo.org. https://www.radiologyinfo.org/en/info.cfm?pg=cholecystitis
Johns Hopkins Medicine. (2020). Barium x-rays (upper and lower GI). https://www.hopkinsmedicine.org/health/conditions-and-diseases/barium-xrays-upper-and-lower-gi
Johns Hopkins Medicine. (2020a). Digestive diagnostic procedures. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/digestive-diagnostic-procedures
Mayo Clinic Staff. (2020, May 22). Gastroesophageal reflux disease. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/gerd/symptoms-causes/syc-20361940
Mayo Clinic Staff. (2018, December 7). Cirrhosis. Mayo Clinic. Available from: https://www.mayoclinic.org/diseases-conditions/cirrhosis/symptoms-causes/syc-20351487
Mayo Clinic Staff. (2019, October 19). Colon polyps. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/colon-polyps/symptoms-causes/syc-20352875
UCLA Health. (n.d.) What is IBD? https://www.uclahealth.org/gastro/ibd/about-ibd
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.
The inside of your nose.
a pair of soft tissue masses located at the rear of the throat (pharynx)
collection of lymphatic tissue located in the lamina propria of the root of the tongue
to secrete externally, directly or through a duct
The sugars, starches and fibers found in fruits, grains, vegetables and milk products.
situated nearer to the center of the body or the point of attachment
Away from the center of the body or from the point of attachment
Resembling lymph or lymphatic tissues
A by-product of the body's metabolism
The process of breaking down the fat into smaller blood cells which makes it easy for enzymes to function and digest food.
A concave region where blood vessels, lymphatic vessels, and nerves also enter the lungs
A part of a hollow organ
Location where the diaphragm has a small opening (hiatus) through which the esophagus passes before connecting.
Poor breakdown of food
A disorder that occurs when people are unable to absorb nutrients from their diets

