Sensory Impairments
7.2 Sensory Impairments Basic Concepts
Interpreting Sensations
Before learning about sensory function, it is important to understand how the nervous system works. An intact nervous system is necessary for information to be delivered from the environment to the brain to trigger responses from the body. For neurons to transmit these messages, they are in the form of an action potential. Sensory receptors perceive a stimulus and then change the sensation to an electrical signal so that it can be transmitted to the brain and then out to the body. For example, a pain receptor perceives pain as your hand touches a hot tray. The signal is transmitted to the brain where it is interpreted, and then signals are quickly sent to the hand to pull away from the hot stimuli.[1]
Our bodies interpret sensations through a process using reception, perception, and reaction. Reception is the first part of the sensory process when a nerve cell or sensory receptor is stimulated by a sensation. Sensory receptors are activated by mechanical, chemical, or temperature stimuli. In addition to our five senses, we also have somatosensation. Somatosensation refers to sensory receptors that respond to stimuli such as pain, pressure, temperature, and vibration. It also includes vestibular sensation, a sense of spatial orientation and balance, and proprioception, the sense of the position of our bones, joints, and muscles. Although these sensory systems are all very different, they share a common purpose. They change a stimulus into an electrical signal that is transmitted in the nervous system.[2]
The sensory receptors for each of our senses work differently from one another. Light receptors, sound receptors, and touch receptors are each activated by different stimuli with specialized receptor specificity. For example, touch receptors are sensitive to pressure but do not have sensitivity to sound or light. Nerve impulses from sensory receptors travel along pathways to the spinal cord or directly to the brain. Some stimuli are also combined in the brain, such as our sense of smell that can affect our sense of taste.[3]
As an individual becomes aware of a stimulus and it is transmitted to the brain, perception occurs. Perception is the interpretation of a sensation. All sensory signals, except olfactory system input, are transmitted to the thalamus and to the appropriate region of the cortex of the brain. The thalamus, which is in the forebrain, acts as a relay station for sensory and motor signals. When a sensory signal leaves the thalamus, it is sent to the specific area of the cortex that processes that sense.[4] However, conditions that affect a person’s consciousness also affect the ability to perceive and interpret stimuli.
Reaction is the response that individuals have to a perception of a received stimulus. The brain determines what sensations are significant because it is impossible to react to all stimuli that are constantly received from our environment. A healthy brain maintains a balance between sensory stimuli received and those reaching awareness. However, sensory overload can occur if the amount of stimuli the brain is receiving is overwhelming to an individual. Sensory deprivation can also occur if there are insufficient sensations from the environment.[5]
Sensory Impairment
Alterations in sensory function include sensory impairment, sensory overload, and sensory deprivation. Sensory impairment includes any type of difficulty that an individual has with one of their five senses. When an individual experiences loss of a sensory function, such as vision, the way they interact with the environment is affected. For example, when an individual gradually loses their vision, their reliance on other senses to receive information from the environment is often enhanced.
Safety is always a nursing consideration for a patient with a sensory impairment. Intact senses are required to make decisions about functioning safely within the environment. For example, an individual who has impaired hearing may not be able to hear a smoke alarm and requires visual indicators when the alarm is triggered.
Sensory impairments are very common in older adults. Most older adults develop impaired near vision called presbyopia. See Figure 7.2[6] for an image of simulated presbyopia.
Deficits in taste and smell are also prevalent in this age group. Additionally, kinesthetic impairment (an altered sense of touch) can occur in adults as young as 55. Kinesthetic impairment can cause difficulty in daily functioning, such as buttoning one’s shirt or performing other fine motor tasks. These sensory losses can greatly impact how older adults live and function.[7]
Vision Impairments
Several types of visual impairments commonly occur in older adults, including macular degeneration, cataracts, glaucoma, diabetic retinopathy, and presbyopia. See Table 7.2 for more information about each of these visual conditions.
Table 7.2 Common Visual Conditions
| Macular Degeneration | Macular degeneration is the leading cause of legal blindness in individuals over 60 years of age. Risk factors include advancing age, a positive family history, hypertension, and smoking. In macular degeneration, there is loss of central vision with classic symptoms such as blurred central vision, distorted vision that causes difficulty driving and reading, and the requirement for brighter lights and magnification for close-up visual activities.[8] |
|---|---|
| Cataracts | Cataracts are the opacity of the lens of the eye that causes clouded, blurred, or dimmed vision. About half of individuals ages 65 to 75 will develop cataracts, with further incidence occurring after age 75. Cataracts can be removed with surgery that replaces the lens with an artificial lens.[9] |
| Glaucoma | Glaucoma is caused by elevated intraocular pressure that leads to progressive damage to the optic nerve, resulting in gradual loss of peripheral vision. It affects about 4% of individuals over age 70.[10] |
| Diabetic Retinopathy | Diabetic retinopathy is the leading cause of blindness in adults diagnosed with type 1 and type 2 diabetes mellitus. Diabetic retinopathy is a complication of diabetes mellitus due to damaged blood vessels in the retina causing vision loss.[11] Patients with diabetes are encouraged to receive annual eye exams so that retinopathy can be discovered and treated early. Treatments, such as laser treatment that can help shrink blood vessels, injections that can reduce swelling, or surgery, can prevent permanent vision loss.[12] |
| Presbyopia | As a person ages, the lens of the eye gradually becomes thicker and loses flexibility. It stops focusing light on the retina correctly, causing impaired near vision and accommodation at all distances. Presbyopia starts in the early to mid-forties and worsens with aging. It can lead to significant visual impairment but does not usually cause blindness.[13] |
Hearing Loss and Ear Problems
Approximately one third of individuals aged 70 and older have hearing loss. Good hearing depends on a series of events that change sound waves in the air into electrical signals. The auditory nerve conducts these electrical signals from the ear to the brain through a series of steps. The structures of the ear, such as the tympanic membrane and cochlea, must be intact and functioning appropriately for conduction of sound to occur. Age-related hearing loss (presbycusis) gradually occurs in most individuals as they age.[14] Typically, low-pitched sounds are easiest to hear, but it often becomes increasingly difficult to hear normal conversation, especially over loud background noise. Hearing aids are commonly used to enhance hearing. See Figure 7.3[15] for an image of common hearing aids used to treat hearing loss.

Hearing loss can be caused by other factors in addition to aging. A build-up of ear wax in the ear canal can cause temporary hearing loss. Sounds that are too loud or long-term exposure to loud noises can cause noise-induced hearing loss. For example, a loud explosion or employment using loud machinery without ear protection can damage the sensory hair cells in the ear. After these hair cells are damaged, the ability to hear is permanently diminished. Tinnitus, a medical term for ringing in the ears, can also occur. Some medications, such as high doses of aspirin or loop diuretics, can cause toxic effects to the sensory cells in the ear and lead to hearing loss or tinnitus.[16],[17] In addition to hearing loss, ear problems can also cause problems with balance, dizziness, and vertigo due to vestibular dysfunction.
Kinesthetic Impairments
Kinesthetic impairments, such as peripheral neuropathy, affect the ability to feel sensations. Symptoms of peripheral neuropathy include sensations of pain, burning, tingling, and numbness in the extremities that decrease a person’s ability to feel touch, pressure, and vibration. Position sense can also be affected and makes it difficult to coordinate complex movements, such as walking, fastening buttons, or maintaining balance when one’s eyes are closed. Peripheral neuropathy is caused by nerve damage that commonly occurs in patients with diabetes mellitus or peripheral vascular disease. It can also be caused by physical injuries, infections, autoimmune diseases, vitamin deficiencies, kidney diseases, liver diseases, and some medications.[18]
Life Span Considerations
Impaired sensory functioning increases the risk for social isolation in older adults. For example, when individuals are not able to hear well, they may pretend to hear in an attempt to avoid embarrassment when asking for the information to be repeated. They may begin to avoid noisy environments or stop participating socially in conversations around them.
Infants and children are also at risk for vision and hearing impairments related to genetic or prenatal conditions. Early determination of sensory impairments is crucial so that problems can be addressed with accommodations to minimize the impact on a child’s development. For example, a screening hearing test is completed on all newborns before discharge to evaluate for hearing impairments that can affect their speech development.
Sensory Overload and Sensory Deprivation
Stimuli are continually received from a variety of sources in our environment and from within our bodies. When an individual receives too many stimuli or cannot selectively filter out meaningful stimuli, sensory overload can occur. Symptoms of sensory overload include irritability, restlessness, covering ears or eyes to shield them from sensory input, and increased sensitivity to tactile input (i.e., scratchy fabric or sensations of medical equipment).[19] Sensory overload affects an individual’s ability to interpret stimuli from their environment and can lead to confusion and agitation. See Figure 7.4[20] of an image of a patient reacting to sensory overload.
The health care environment with its frequent noisy alarms, treatments, staff interruptions, and noisy hallway conversations can cause sensory overload for patients. Individuals have different tolerances for the amount of stimuli that will affect them adversely. Tolerance to stimuli is impacted by factors such as pain, stress levels, sleep patterns, physical health, and emotional health. When sensory overload occurs in a hospitalized patient, it can lead to delirium and acute confusion. It is important for the nurse to limit unnecessary awakenings and interactions with the health care team members when a patient is experiencing sensory overload.

Conversely, symptoms of sensory deprivation may occur when there are a lack of stimuli. People experiencing sensory deprivation often report perceptual disturbances such as hallucinations. Symptoms of sensory deprivation can mimic delirium, so it is important for a nurse to further investigate new perceptual disturbances.[21]
- This work is a derivative of StatPearls by Gadhvi & Waseem and is licensed under CC BY 4.0 ↵
- This work is a derivative of Sensory Processes by Lumen Learning and is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Sensory Processes by Lumen Learning and is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Sensory Processes by Lumen Learning and is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Sensory Processes by Lumen Learning and is licensed under CC BY-SA 4.0 ↵
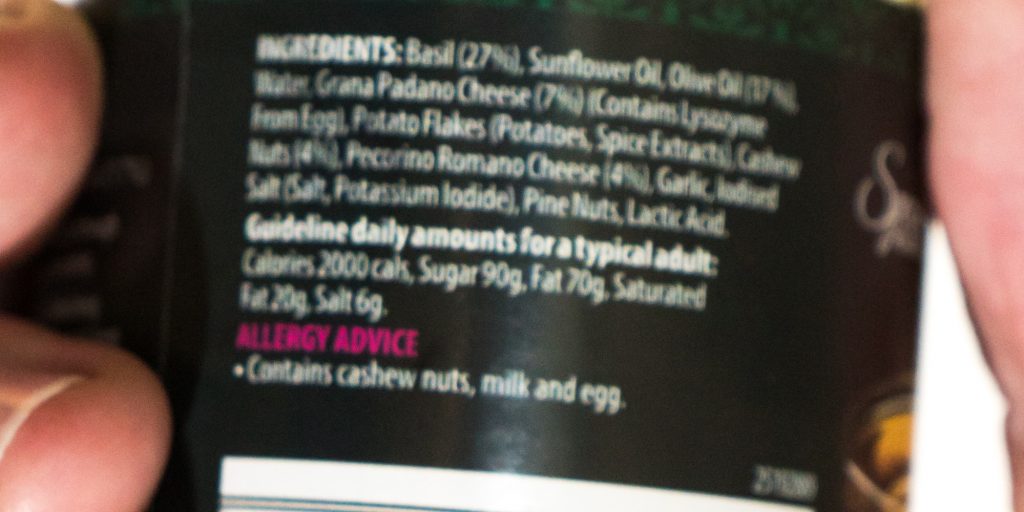
- “Pesto ingredients - blurred.jpg” by Colin is licensed under CC BY-SA 4.0 ↵
- Correia, C., Lopez, K. J., Wroblewski, K. E., Huisingh-Scheetz, M., Kern, D. W., Chen, R. C., Schumm, L. P., Dale, W., McClintock, M. K., & Pinto, J. M. (2016). Global sensory impairment in older adults in the United States. Journal of the American Geriatrics Society, 64(2), 306–313. https://doi.org/10.1111/jgs.13955 ↵
- Loh, K. Y., & Ogle, J. (2004). Age related visual impairment in the elderly. The Medical Journal of Malaysia, 59(4), 562–569. https://pubmed.ncbi.nlm.nih.gov/15779599/ ↵
- Loh, K. Y., & Ogle, J. (2004). Age related visual impairment in the elderly. The Medical Journal of Malaysia, 59(4), 562–569. https://pubmed.ncbi.nlm.nih.gov/15779599/ ↵
- Loh, K. Y., & Ogle, J. (2004). Age related visual impairment in the elderly. The Medical Journal of Malaysia, 59(4), 562–569. https://pubmed.ncbi.nlm.nih.gov/15779599/ ↵
- Loh, K. Y., & Ogle, J. (2004). Age related visual impairment in the elderly. The Medical Journal of Malaysia, 59(4), 562–569. https://pubmed.ncbi.nlm.nih.gov/15779599/ ↵
- Centers for Disease Control and Prevention. (2018, November 5). Watch out for diabetic retinopathy. https://www.cdc.gov/features/diabetic-retinopathy/index.html ↵
- Loh, K. Y., & Ogle, J. (2004). Age related visual impairment in the elderly. The Medical Journal of Malaysia, 59(4), 562–569. https://pubmed.ncbi.nlm.nih.gov/15779599/ ↵
- National Institute on Deafness and Other Communication Disorders. (2018, July 17). Age-related hearing loss. https://www.nidcd.nih.gov/health/age-related-hearing-loss ↵
- "Traditional_hearing_aids.jpg” by ikesters is licensed under CC BY-SA 2.0 ↵
- National Institute on Deafness and Other Communication Disorders. (2018, July 17). Age-related hearing loss. https://www.nidcd.nih.gov/health/age-related-hearing-loss ↵
- American Speech-Language-Hearing Association. (n.d.). Causes of hearing loss in adults. https://www.asha.org/public/hearing/causes-of-hearing-loss-in-adults/ ↵
- National Institute of Neurological Disorders and Stroke. (2020, March 16). Peripheral neuropathy fact sheet. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Peripheral-Neuropathy-Fact-Sheet ↵
- Watson, K. (2018, September 27). What is sensory overload? https://www.healthline.com/health/sensory-overload#causes ↵
- “Sensory_Overload.jpg” by Stewart Black is licensed under CC BY 2.0 ↵
- Mason, O., & Brady, F. (2009). The psychotomimetic effects of short-term sensory deprivation. The Journal of Nervous and Mental Disease, 197(10), 783-785. https://doi.org/10.1097/nmd.0b013e3181b9760b ↵
Grieving a loss is a normal process that has implications for both patient and family well-being. NANDA formally recognizes the dimensions of grief with the nursing diagnoses of Grieving and Complicated Grieving. Recall that grief can be experienced due to many types of loss, in addition to death. For example, when patients receive a diagnosis of breast cancer, they may demonstrate signs of various stages of grief, such as denial, anger, bargaining, depression, and acceptance. When undergoing mastectomy and chemotherapy, the patient may grieve over the loss of prior body image.
Communities can also experience grief. For example, when a town experiences a significant tragedy, such as a devastating flood or a tornado, there can be widespread community grief as families grieve the loss of life, property, or a previous way of life. In these situations, nurses are cognizant of the multiple factors that may impact an individual’s health and grieving process. Identifying these factors can help ensure that appropriate resources are mobilized to facilitate coping and progression through the grief process.
Assessment
Grief assessment includes the patient, family members, and significant others. It begins when a patient is diagnosed with an acute, chronic, or terminal illness and/or when the patient is admitted to a hospital, nursing facility, or assisted living facility. It continues throughout the course of a terminal illness for the patient, family members, and significant others and then continues through the bereavement period for the survivors. During the bereavement period, the nurse monitors for symptoms of complicated grief.[1]
Grief can be manifested by physical, emotional, and cognitive symptoms. Physical symptoms can occur, such as feeling ill, headaches, tremors, muscle aches, exhaustion, insomnia, loss of appetite, or weight loss or gain. Cognitive symptoms may occur, such as lack of concentration, confusion, and hallucinations. Emotional symptoms, such as anxiety, guilt, anger, fear, sadness, helplessness, or feelings of relief may occur. These symptoms of grief and loss can be manifested in many different ways and can vary from day to day. Manifestations of grief are unique to the individual and may be influenced by one’s age, culture, resources, and previous experiences with loss. Additionally, as patients cope with grief and loss, it is important for the nurse to recognize that support is often needed by their family members.[2]
Any behavior that may endanger the patient or family should be reported to the health care provider, such as symptoms of depression, suicidal ideation, or symptoms lasting greater than six months.
Diagnoses
Consult a nursing care planning resource when selecting nursing diagnoses for patients and their family members experiencing grief. See Table 17.3 for definitions and selected defining characteristics of the NANDA-I diagnoses Grieving and Complicated Grieving while also keeping in mind the previous discussion in this chapter regarding stages and tasks of normal grief.
Table 17.3 NANDA-I Nursing Diagnoses Related to Grieving[3]
| NANDA-I Diagnosis | Definition | Selected Defining Characteristics |
|---|---|---|
| Grieving | A normal, complex process that includes emotional, physical, spiritual, social, and intellectual responses and behaviors by which individuals, families, and communities incorporate an actual, anticipated, or perceived loss into their daily lives. |
|
| Complicated Grieving | A disorder that occurs after the death of a significant other, in which the experience of distress accompanying bereavement fails to follow normative expectations and manifests in functional impairment. |
|
Examples
See the following for examples of PES statements related to Grieving and Complicated Grieving:
- A patient diagnosed with metastatic cancer is advised they have less than six months to live. They begin to move through the stages of grief as they assimilate this information. A sample NANDA-I diagnosis in current PES format is: “Grieving related to anticipatory loss as evidenced by detachment, disorganization, and alteration in activity level.” The nurse would plan and implement interventions to enhance coping for this patient.
- A patient’s husband died two years ago, and she continues to be preoccupied with thoughts about her husband. Her grown children live several hours away, and she becomes isolated and unable to complete daily activities, such as cleaning the house and grocery shopping. A sample PES statement is: “Complicated Grieving related to insufficient social support as evidenced by avoidance of decreased functioning and preoccupation with thoughts about her deceased husband.” The nurse would plan interventions to facilitate grief work while also arranging for assistance with ADLs and IADLs in the patient’s home.
Outcome Identification
Goal setting and outcome identification for patients and family members experiencing grief are customized to the specific situation and focus on grief resolution. Grief resolution is evidenced by the following indicators:
- Resolves feelings about the loss
- Verbalizes reality and acceptance of loss
- Maintains living environment
- Seeks social support[4]
For the nursing diagnosis of Grieving and Complicated Grieving, a sample goal is, “The patient will experience grief resolution.”
A sample SMART outcome is, “The patient will discuss the meaning of the loss to their life in the next 2 weeks.”[5]
Planning and Implementing Interventions
Nurses are in the ideal position to assist patients with identifying and expressing their feelings related to loss. The most important intervention that nurses can provide is active listening and offering a supportive presence. Actively listening to the bereaved helps them express their feelings and relate the emotions and feelings related to the loss. Interventions to facilitate grief resolution focus on coping enhancement, anticipatory grieving interventions, and grief work facilitation.
Coping Enhancement
Interventions to enhance coping can be implemented for patients and families experiencing any type of actual, anticipated, or perceived loss. Sample interventions include the following:[6]
- Assist the patient in identifying short- and long-term goals.
- Assist the patient in examining available resources to meet the goals.
- Assist the patient in breaking down complex steps into small, manageable steps.
- Encourage relationships with others who have common interests and goals.
- Assist the patient to solve problems in a constructive manner.
- Appraise the effect of a patient’s life situation on roles and relationships.
- Appraise and discuss alternative responses to the situation.
- Use a calm, reassuring approach.
- Provide an atmosphere of acceptance.
- Help the patient identify information they are most interested in obtaining.
- Provide factual information regarding medical diagnosis, treatment, and prognosis.
- Provide the patient with realistic choices about certain aspects of care.
- Encourage an attitude of realistic hope as a way of dealing with hopelessness.
- Seek to understand the patient’s perspective of a stressful situation.
- Discourage decision-making when the patient is under severe stress.
- Acknowledge the patient’s cultural and spiritual background and encourage use of spiritual resources, if desired.
- Encourage verbalization of feelings, perceptions, and fears.
- Encourage family involvement, as appropriate.
- Assist the patient to identify positive strategies to deal with limitations and manage needed lifestyle or role changes.
- Instruct the patient on the use of relaxation techniques.
See Figure 17.18[7] for an image of a nurse enhancing a patient’s ability to cope with their illness through active listening and touch.

Anticipatory Grieving Interventions
Anticipatory grieving refers to a grief reaction that occurs in anticipation of an impending loss. Recall that anticipatory grieving can be related to impending death of oneself or a loved one, but it can also occur in anticipation of other losses, such as the loss of a body part due to scheduled surgery or the loss of one’s home due to a move to a long-term care facility. Interventions to facilitate resolution of anticipatory grieving include the following:[8]
- Develop a trusting relationship with the patient and family members by using presence and other therapeutic communication techniques.
- Keep the patient and family members apprised of the patient’s ongoing condition as much as possible.
- Keep the family informed of the patient’s needs for physical care and support in symptom control, and inform them about health care options at the end of life, including palliative care, hospice care, and home care.
- Actively listen as the patient grieves for their own death or loss. Normalize the patient’s expressions of grief.
- Discuss the patient’s preferred place of death and document their wishes.
- Ask family members about having adequate resources to care for themselves and the critically ill family member.
- Recognize caregiver role strain in family members providing long-term care at home.
- Listen to the family member’s story.
- Encourage family members to show their caring feelings and talk with the family members.
- Recognize and respect different feelings and wishes from the patient and their family members.
- Refer the patient and family members to counselors or chaplains for spiritual care as appropriate.
Grief Work Facilitation
Grief work facilitation assists patients and family members in resolution of a significant loss. Sample interventions include the following:[9]
- Identify the loss.
- Assist the patient to identify the initial reaction to the loss.
- Listen to expressions of grief.
- Encourage discussion of previous loss experiences.
- Encourage the verbalization of memories of the loss.
- Make empathetic statements about grief.
- Encourage identification of greatest fears concerning the loss.
- Educate about stages and tasks of the grieving process, as appropriate.
- Support progression through personal grieving stages.
- Assist in identifying personal coping strategies.
- Encourage implementation of cultural, religious, and social customs associated with the loss.
- Answer children’s questions about the loss and encourage discussion of feelings.
- Identify sources of community support.
- Reinforce progress made in the grieving process.
- Assist in identifying modifications needed in lifestyle.
Community Resources
Bereavement follow-up with families is a component of hospice programs and includes formal activities and events to promote closure and acceptance. Many hospices have nondenominational memorial services to honor patients. Family members and staff are invited to participate, which can be effective at helping individuals find closure. Other formal types of support can include organized support groups to facilitate discussion and coping. Individual, group counseling, or psychotherapy are other methods that can assist the bereaved in coping with their loss. See additional resources for family members in the following box.
Additional Resources for Grief and Loss
Evaluation
It is always important to evaluate the effectiveness of interventions implemented. Nurses assess the effectiveness of interventions in helping individuals cope and work through the grief process based on the customized outcome criteria established for their situation.
Now that we have discussed basic concepts and the nursing process related to the grieving process, let’s discuss more details regarding providing palliative care. Nurses provide palliative care whenever caring for patients with chronic disease. As the disease progresses and becomes end-stage, the palliative care they provide becomes even more important. As previously discussed, palliative care is “patient and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care occurs throughout the continuum of care and involves the interdisciplinary team collaboratively addressing physical, intellectual, emotional, social, and spiritual needs and facilitating patient autonomy, access to information, and choice.”[10]
Providing care at the end of life is similar for patients with a broad variety of medical diagnoses. It addresses multiple dimensions of care, including physical, psychological, social, and spiritual aspects:
- Physical: Functional ability, strength/fatigue, sleep/rest, nausea, appetite, constipation, and pain
- Psychological: Anxiety, depression, enjoyment/leisure, pain, distress, happiness, fear, and cognition/attention
- Social: Financial burden, caregiver burden, roles/relationships, affection, and appearance
- Spiritual: Hope, suffering, the meaning of pain, religiosity, and transcendence[11]
The interdisciplinary team manages pain and other symptoms, assists with difficult medical decisions, and provides additional support to patients, family members, and caregivers. Nurses have the opportunity to maintain hope for patients and family members by providing excellent physical, psychosocial, and spiritual palliative care. Nursing interventions begin immediately after the initial medical diagnosis and continue throughout the continuum of care until the end of life. As a patient approaches end-of-life care, nursing interventions include the following:
- Eliciting the patient’s goals for care
- Listening to the patient and their family members
- Communicating with members of the interdisciplinary team and advocating for the patient’s wishes
- Managing end-of-life symptoms
- Encouraging reminiscing
- Facilitating participating in religious rituals and spiritual practices
- Making referrals to chaplains, clergy, and other spiritual support[12]
While providing palliative care, it is important to remain aware that some things cannot be “fixed”:
- We cannot change the inevitability of death.
- We cannot change the anguish felt when a loved one dies.
- We must all face the fact that we, too, will die.
- The perfect words or interventions rarely exist, so providing presence is vital.[13]
The Palliative Care Network of Wisconsin contain excellent resources for nurses providing care for seriously ill patients.
View the "Fast Facts" page for extensive information about palliative care and end of life topics.
Management of Common Symptoms
Many patients with serious, life-limiting illnesses have common symptoms that the nurse can assess, prevent, and manage to optimize their quality of life. These symptoms include pain, dyspnea, cough, anorexia and cachexia, constipation, diarrhea, nausea and vomiting, depression, anxiety, cognitive changes, fatigue, pressure injuries, seizures, and sleep disturbances. Good symptom management improves quality of life and functioning at all states of chronic illness. Nurses play a critical role in recognizing these symptoms and communicating them to the interdisciplinary team for optimal management. The plan of care should always be based on the patient’s goals and their definition of quality of life.[14] These common symptoms are discussed in the following subsections.
Pain
Pain is frequently defined as “whatever the experiencing person says it is, existing whenever he says it does.”[15] When a patient is unable to verbally report their pain, it is important to assess nonverbal and behavioral indicators of pain. The goal is to balance the patient’s desire for pain relief, along with their desire to manage side effects and oversedation. There are many options available for analgesics. Reassure a patient that reaching their goal of satisfactory pain relief is achievable. Read more about pain management in the “Comfort” chapter. See Figure 17.19[16] for an image illustrating a patient experiencing pain.

Dyspnea
Dyspnea is a subjective experience of breathing discomfort and is the most reported symptom by patients with life-limiting illness. Dyspnea can be extremely frightening. Assessing dyspnea can be challenging because the patient’s respiratory rate and oxygenation status do not always correlate with the symptom of breathlessness.[17] See Figure 17.20[18] for an image of a patient experiencing dyspnea.

When assessing dyspnea, include the following components:
- Ask the patient to rate the severity of their breathlessness on a scale of 0-10
- Assess their ability to speak in sentences, phrases, or words
- Assess the patient’s anxiety
- Observe respiratory rate and effort
- Measure oxygenation status (i.e., pulse oximetry or ABG)
- Auscultate lung sounds
- Assess for the presence of chest pain or other pain
- Assess factors that improve or worsen breathlessness
- Evaluate the impact of dyspnea on functional status and quality of life[19]
If you suspect that new dyspnea is caused by an acute condition, report assessment findings immediately to a health care provider. However, in end-stage disease, dyspnea can be a chronic condition that is treated with pharmacological and nonpharmacological management. Relatively small doses of opioids can be used to improve dyspnea while having little impact on their respiratory status or a patient’s life expectancy. The dosage should be titrated to the patient’s desired goals for relief of dyspnea without over sedation.
Nonpharmacological interventions for dyspnea include pursed-lip breathing, energy conservation techniques, fans and open windows to circulate air, elevation of the patient bed, placing the patient in a tripod position, and relaxation techniques such as music and a calm, cool environment. Patient education can also reduce anxiety.[20] Read more about nonpharmacological interventions for dyspnea in the “Oxygenation” chapter.
Cough
A cough can be frustrating and debilitating for a patient, causing pain, fatigue, vomiting, and insomnia. See Figure 17.21[21] for an image of a patient with a chronic cough. Coughing is frequently present in advanced diseases such as chronic obstructive pulmonary disease (COPD), heart failure (HF), cancer, and AIDS. There are several potential causes of a cough. Medications that can be used to control a cough are opioids, dextromethorphan, and benzonatate. Guaifenesin can be used to thin thick secretions, and anticholinergics (such as scopolamine) can be used for high-volume secretions.

Anorexia and Cachexia
Anorexia (loss of appetite or loss of desire to eat) and cachexia (wasting of muscle and adipose tissue due to lack of nutrition) are commonly found in advanced disease. See Figure 17.22[22] for an image of a patient with cachexia. Weight loss is present in both conditions and is associated with decreased survival. Unfortunately, aggressive nutritional treatment does not improve survival or quality of life and can actually create more discomfort for the patient.[23]

Assessment of anorexia and cachexia focuses on understanding the patient’s experience and concerns, as well as determining potentially reversible causes. Referral to a dietician may be needed. Read more about nutritional assessment in the “Nutrition” chapter.
Interventions for anorexia and cachexia should be individualized for each patient with the goal being eating for pleasure for those at the end of life. Patients should be encouraged to eat their favorite foods, as well as select foods that are high in calories and easy to chew. Small, frequent meals with pleasing food presentation are important. Family members should be aware that odors associated with cooking can inhibit eating. The patient may need to be moved away from the kitchen or cooking times separated from eating times.[24]
Medication may be prescribed to increase intake, such as mirtazapine or olanzapine. Prokinetics such as metoclopramide may be helpful in increasing gastric emptying. Medical marijuana or dronabinol may also be useful. In some cases, enteral nutrition is helpful for patients who continue to have an appetite but cannot swallow.[25]
Patient and family member education about anorexia at the end of life is important. Nurses should be aware that many family members perceive eating as a way to “get better” and are distressed to see their loved one not eat. After listening respectfully to their concerns, explain that the patient may feel more discomfort when forcing themselves to eat.
Constipation
Constipation is a frequent symptom in many patients at the end of life for many factors, such as low intake of food and fluids, use of opioids, chemotherapy, and impaired mobility. Constipation is defined as having less than three bowel movements per week. The patient may experience associated symptoms such as rectal pressure, abdominal cramps, bloating, distension, and straining. See Figure 17.23[26] for an image of a patient experiencing constipation.

The goal is to establish what is considered normal for each patient and to have a bowel movement at least every 72 hours regardless of intake. Treatment includes a bowel regimen such as oral stool softeners (i.e., docusate) and a stimulant (i.e., sennosides). Rectal suppositories (i.e., bisacodyl) or enemas should be considered when oral medications are not effective or the patient can no longer tolerate oral medications.[27]
Read more about managing constipation in the “Elimination” chapter.
Diarrhea
Diarrhea is defined as having more than three unformed stools in 24 hours. Diarrhea can be especially problematic for patients receiving chemotherapy, pelvic radiation, or treatment for AIDS. It can cause dehydration, skin breakdown, and electrolyte imbalances and dramatically affect a person’s quality of life. It can also be a huge burden for caregivers.[28]
Early treatment of diarrhea includes promoting hydration with water or fluids that improve electrolyte status (i.e., sports drinks). Intravenous fluids may be required based on the patient’s disease stage and goals for care. Medications such as loperamide, psyllium, and anticholinergic agents may also be prescribed.
Read more about managing diarrhea in the “Elimination” chapter.
Nausea and Vomiting
Nausea is common in advanced disease and is a dreaded side effect of many treatments for cancer. Assessment of nausea and vomiting should include the patient’s history, effectiveness of previous treatment, medication history, frequency and intensity of episodes of nausea and vomiting, and activities that precipitate or alleviate nausea and vomiting.[29]
Nonpharmacological interventions for nausea include eating meals and fluids at room temperature, avoiding strong odors, avoiding high-bulk meals, using relaxation techniques, and listening to music therapy.[30] Antiemetic medications, such as prochlorperazine and ondansetron, may be prescribed.
Read more information about managing nausea in the “Antiemetics” section of the Gastrointestinal chapter in Open RN Nursing Pharmacology.
Depression
Patients who have a serious life-threatening illness will normally experience sadness, grief, and loss, but there is usually some capacity for pleasure. Persistent feelings of helplessness, hopelessness, and suicidal ideation are not considered a normal part of the grief process and should be treated. Undertreated depression can cause a decreased immune response, decreased quality of life, and decreased survival time. Evaluation of depression requires interdisciplinary assessment and referrals to social work and psychiatry may be needed.[31]
Antidepressants such as serotonin selective reuptake inhibitors (i.e., fluoxetine, paroxetine, sertraline, or citalopram) are generally prescribed as first-line treatment of depression. Other medication may be prescribed if these medications are not effective.
Nonpharmacological interventions for depression may include the following:
- Promoting and facilitating as much autonomy and control as possible
- Encouraging patient and family participation in care, thus promoting a sense of control and reducing feelings of helplessness
- Reminiscing and life review to focus on life accomplishments and to promote closure and resolution of life events. See Figure 17.24[32] for an image of reminiscing with pictures.
- Grief counseling to assist patients and families in dealing with loss
- Maximizing symptom management
- Referring to counseling for those experiencing inability to cope
- Assisting the patient to draw on previous sources of strength, such as faith, religious rituals, and spirituality
- Referring for cognitive behavioral techniques to assist with reframing negative thoughts into positive thoughts
- Teaching relaxation techniques
- Providing ongoing emotional support and “being present”
- Reducing isolation
- Facilitating spiritual support[33]

A suicide assessment is critical for a patient with depression. It is important for nurses to ask questions, such as these:
- Do you have interest or pleasure in doing things?
- Have you had thoughts of harming yourself?
- If yes, do you have a plan for doing so?
To destigmatize the questions, it is helpful to phrase them in the following way, “It wouldn’t be unusual for someone in your circumstances to have thoughts of harming themselves. Have you had thoughts like that?" Patients with immediate, precise suicide plans and resources to carry out this plan should be immediately evaluated by psychiatric professionals.[34]
Anxiety
Anxiety is a subjective feeling of apprehension, tension, insecurity, and uneasiness, usually without a known specific cause. It may be anticipatory. It is assessed along a continuum as mild, moderate, or severe. Patients with life-limiting illness will experience various degrees of anxiety due to various issues such as their prognosis, mortality, financial concerns, uncontrolled pain and other symptoms, and feelings of loss of control.[35]
Physical symptoms of anxiety include sweating, tachycardia, restlessness, agitation, trembling, chest pain, hyperventilation, tension, and insomnia. Cognitive symptoms include recurrent and persistent thoughts and difficulty concentrating. See Figure 17.25[36] for an illustration of anxiety.

Benzodiazepines (i.e., lorazepam), may be prescribed to treat anxiety. However, the nurse should assess for adverse effects such as oversedation, falls, and delirium, especially in the frail elderly.
Nonpharmacological interventions are crucial and include the following:
- Maximizing symptom management to decrease stressors
- Promoting the use of relaxation and guided imagery techniques, such as breathing exercises, progressive muscle relaxation, and the use of audiotapes
- Referring for psychiatric counseling for those unable to cope with the experience of their illness
- Facilitating spiritual support by contacting chaplains and clergy
- Acknowledging patient fears and using open-ended questions and active listening with therapeutic communication
- Identifying effective coping strategies the patient has used in the past, as well as teaching new coping skills such as as relaxation and guided imagery techniques
- Providing concrete information to eliminate fear of the unknown
- Encouraging the use of a stress diary that helps the patient understand the relationship between situations, thoughts, and feelings[37]
Cognitive Changes
Delirium is a common cognitive disorder in hospitals and palliative care settings. Delirium is an acute change in cognition and requires urgent management in inpatient care. Up to 90% of patients at the end of life will develop delirium in their final days and hours of life. Early detection of delirium can cause resolution if the cause is reversible.[38]
Symptoms of delirium include agitation, confusion, hallucinations, or inappropriate behavior. It is important to obtain information from the caregiver to establish a mental status baseline. The most common cause of delirium at end of life is medication, followed by metabolic insufficiency due to organ failure.[39]
Medications such as neuroleptics (i.e., haloperidol and chlorpromazine) or benzodiazepines may be prescribed. It is also important to remember that delirium can be related to opioid toxicity. It may be helpful to request the presence of family to reorient the patient, as well as provide nonpharmacological interventions such as massage, distraction, and relaxation techniques.[40]
Read more about delirium in the “Cognitive Impairments” chapter.
Fatigue
Fatigue has been cited as the most disabling condition for patients receiving a variety of treatments in palliative care. Fatigue is defined as a distressing, persistent, subjective sense of physical, emotional, and/or cognitive tiredness or exhaustion that is not proportional to activity and interferes with usual functioning.[41] See Figure 17.26[42] for an image of an older patient experiencing fatigue.

The primary cause of fatigue is metabolic alteration related to chronic disease, but it can also be caused by anemia, infection, poor sleep quality, chronic pain, and medication side effects. Nonpharmacological interventions include energy conservation techniques.
Pressure Injuries
Patients at end of life are at risk for quickly developing pressure injuries, formerly referred to as pressure ulcers. Prevention is key and requires interventions such as promoting mobility, reducing moisture, and encouraging nutrition as appropriate.
The Kennedy Terminal Ulcer is a type of pressure injury that some patients develop shortly before death resulting from multiorgan failure. It usually starts on the sacrum and is shaped like a pear, butterfly, or horseshoe. It is red, yellow, black, or purple in color with irregular borders and progresses quickly. For example, the injury may be identified by a nurse at the end of a shift who says, “That injury was not present when I assessed the patient this morning.”[43]
Read more about assessing, preventing, and treating pressure injuries in the “Integumentary” chapter.
Seizures
Seizures are sudden, abnormal, excessive electrical impulses in the brain that alter neurological functions such as motor, autonomic, behavioral, and cognitive function. A seizure can be caused by infection, trauma, brain injury, brain tumors, side effects of medications, metabolic imbalances, drug toxicities, and withdrawal from medications.[44]
Seizures can have gradual or acute onset and include symptoms such as mental status changes, motor movement changes, and sensory changes. Treatment is focused on prevention and limiting trauma that occur during the seizure. Medications may be prescribed such as phenytoin, phenobarbital, benzodiazepines, or levetiracetam.[45]
Sleep Disturbances
Sleep disturbances affect quality of life and can cause much suffering. It can be caused by poor pain and symptom management, as well as environmental disturbances. Nurses can promote improved sleep for inpatients by creating a quiet, calm environment, promoting sleep routines, and advocating for periods of uninterrupted rest without disruptions by the health care team.
Read more about promoting good sleep in the “Sleep and Rest” chapter.
Spiritual Distress
When patients are initially diagnosed with an illness or experience a serious injury, they often grapple with the existential question, “Why is this happening to me?” This question is often a sign of spiritual distress. Spiritual distress is defined by NANDA-I as, “A state of suffering related to the inability to experience meaning in life through connections with self, others, the world, or a superior being.”[46] Nurses can help relieve this suffering by therapeutically responding to patients’ signs of spiritual distress and advocating for their spiritual needs throughout their health care experience.
Spirituality
Provision 1 of the ANA Code of Ethics states, “The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person” and “optimal nursing care enables the patient to live with as much physical, emotional, social, and religious or spiritual well-being as possible and reflects the patient’s own values.”[47]
Spiritual well-being is a pattern of experiencing and integrating meaning and purpose in life through connectedness with self, others, art, music, literature, nature, and/or a power greater than oneself.[48] Spirituality is defined by the Interprofessional Spiritual Care Education Curriculum (ISPEC) as, “A dynamic and intrinsic aspect of humanity through which persons seek ultimate meaning, purpose, and transcendence and experience relationship to self, family, others, community, society, nature, and the significant or sacred.”[49] Spiritual needs and spirituality are often mistakenly equated with religion, but spirituality is a broader concept. Elements of spirituality include faith, meaning, love, belonging, forgiveness, and connectedness.[50] Spirituality and spiritual values in the context of nursing are closely intertwined with the concept of caring.[51] See Figure 18.1[52] for an illustration of spirituality.

An integrative review of nursing research and resources was completed in 2014 to describe the impact of spirituality and spiritual support in nursing.[53] See the following box for discussion of findings from this integrative review.
Integrative Review of Spirituality in Nursing[54]
An integrative review of nursing literature selected 26 articles published between 1999 and 2013 to describe the experiences of spirituality and the positive impact of spiritual support in nursing literature.[55] Spirituality was described as the integration of body, mind, and spirit into a harmonious whole (often referred to as holistic care). Spirituality was associated with the development of inner strength, looking into one’s own soul, believing there is more to life than worldly affairs, and trying to understand who we are and why we are on this earth.
Transcendence was described as an understanding of being part of a greater picture or of something greater than oneself, such as the awe one can experience when walking in nature. It was also expressed as a search for the sacred through subjective feelings, thoughts, and behaviors. Spirituality was found to have a positive effect on patients’ health and promoted recovery by viewing life from different perspectives and looking beyond one’s own anxiety to develop an understanding of illness and change.
Relationships and connectedness were also found to be powerful spiritual interventions that contributed to an individual’s spirituality. This included embracing, crying together, gift giving, having coffee together, and visiting each other. Laughter, happy thoughts, and the smiles of others were considered comforting. Being with others was described as a primary spiritual need, and conversation was unnecessary. Spirituality brought about the realization that the relationship with family and friends is important and involves finding a healthy balance in relationships among friends, family, society, and a higher power. Presence was the most influential element in positively influencing recovery. The presence of family and friends was a calming experience that brought forth comfort, peace, happiness, joy, acceptance, and hope.
Nurses facilitate their patients’ search for meaning by enabling them to express personal beliefs, as well as by supporting them in taking part in their religious and cultural practices. Furthermore, nurses assess and meet their patients’ spiritual needs by using active listening when talking, asking questions, and picking up patient cues. Active listening requires nurses to be fully present, especially when patients appear depressed or upset.
Nurses were found to use their own spirituality when helping patients achieve spiritual well-being. A desire to help others in need is an important part of spirituality, which is also described as discovering meaning and purpose in life and offering the gift of self to others. Helping others also brings a sense of self-worth, personal fulfilment, and satisfaction.
Spiritual Assessment
The Joint Commission requires that health care organizations provide a spiritual assessment when patients are admitted to a hospital. Spiritual assessment can include questions such as the following:
- Who or what provides you with strength or hope?
- How do you express your spirituality?
- What spiritual needs can we advocate for you during this health care experience?
In addition to performing a routine spiritual assessment on admission, nurses often notice other cues related to a patient’s spiritual distress or desire to enhance their spiritual well-being. When these cues are identified, spiritual care should be provided to relieve suffering and promote spiritual health. There are several nursing interventions that can be implemented, in addition to contacting the health care agency’s chaplain or the patient’s clergy member. See the “Applying the Nursing Process” section for a discussion of spiritual assessment tools and nursing interventions related to spiritual care.
Many hospitals, nursing homes, assisted living facilities, and hospices employ professionally trained chaplains to assist with the spiritual, religious, and emotional needs of patients, family members, and staff. In these settings, chaplains support and encourage people of all religious faiths and cultures and customize their approach to each individual’s background, age, and medical condition. Chaplains can meet with any individual regardless of their belief, or lack of belief, in a higher power and can be very helpful in reducing anxiety and distress. A nurse can make a referral for a chaplain without a provider order. See Figure 18.2[56] for an image of a hospital chaplain offering support to a patient.

A chaplain assists patients and their family members to develop a spiritual view of their serious illness, injury, or death, which promotes coping and healing. A spiritual view of life and death includes elements such as the following:
-
- Suffering occurs at physical, mental, emotional, and spiritual levels. Sociocultural factors, religious beliefs, family values and dynamics, and other environmental factors affect a person’s response to suffering.
- Hope is a desire or goal for a particular event or outcome. For example, some people may view dying as “hopeless” whereas a spiritual view can define hope as a “good death” when the patient dies peacefully according to the end-of-life preferences they previously expressed. Read more about the concept of a “good death” in the "Grief and Loss" chapter.
- Mystery is knowing there is truth beyond understanding and explanation.
- Peacemaking is the creation of a space for nurturing and healing.
- Forgiveness is an internal process releasing intense emotions attached to past incidents. Self-forgiveness is essential to spiritual growth and healing.
- Prayer is an expression of one's spirituality through a personalized interaction or organized form of petitioning and worship.
Learning Objectives
- Demonstrate principles of holistic care by incorporating cultural, religious, and spiritual influences on patient health
- Explain the interconnection between spirituality and religious concepts as they relate to health and spiritually sensitive nursing care
- Describe methods to assess the spiritual and religious preferences, strengths, concerns, or distress of clients and plan appropriate nursing care
Spirituality includes a sense of connection to something bigger than oneself and typically involves a search for meaning and purpose in life. People may describe a spiritual experience as sacred or transcendent or simply feel a deep sense of aliveness and interconnectedness. Some people’s spiritual life is linked to a religious association with a church, temple, mosque, or synagogue, whereas others pray and find comfort in a personal relationship with God or a higher power and still others find meaning through their connections to nature or art. A person’s definition of spirituality and sense of purpose often change throughout one’s lifetime as it evolves based on personal experiences and relationships.[61]
Over the past decade, research has demonstrated the importance of spirituality in health care. Spiritual distress is very common in patients and their family members experiencing serious illness, injury, or death, and nurses are on the front lines as they assist these individuals to cope. Addressing a patient’s spirituality and providing spiritual care have been shown to improve patients’ health and quality of life, including how they experience pain, cope with stress and suffering associated with serious illness, and approach end of life.[62],[63]
Consensus-driven recommendations define a spiritual care model where all clinicians address spiritual issues and work with trained chaplains who are spiritual care specialists.[64],[65] By therapeutically using presence, unconditional acceptance, and compassion, nurses often provide spiritual care and help patients find hope and meaning in their life experiences.[66] The Interprofessional Spiritual Care Education Curriculum (ISPEC), developed by George Washington University for health care professionals, is an education initiative to improve spiritual care for seriously ill patients in the United States and internationally. This chapter will introduce concepts included in the ISPEC curriculum, review religious beliefs and practices of various world religions, and discuss therapeutic interventions that nurses can use to promote patients’ and their own spiritual well-being.
Read more about professional development opportunities regarding spiritual health using the Interprofessional Spiritual Care Education Curriculum (ISPEC) offered by George Washington University Institute for Spirituality and Health.
Explore more information about spirituality using free online resources provided by the University of Minnesota’s Earl E. Bakken Center for Spirituality and Healing.
Spiritual Distress
When patients are initially diagnosed with an illness or experience a serious injury, they often grapple with the existential question, “Why is this happening to me?” This question is often a sign of spiritual distress. Spiritual distress is defined by NANDA-I as, “A state of suffering related to the inability to experience meaning in life through connections with self, others, the world, or a superior being.”[67] Nurses can help relieve this suffering by therapeutically responding to patients’ signs of spiritual distress and advocating for their spiritual needs throughout their health care experience.
Spirituality
Provision 1 of the ANA Code of Ethics states, “The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person” and “optimal nursing care enables the patient to live with as much physical, emotional, social, and religious or spiritual well-being as possible and reflects the patient’s own values.”[68]
Spiritual well-being is a pattern of experiencing and integrating meaning and purpose in life through connectedness with self, others, art, music, literature, nature, and/or a power greater than oneself.[69] Spirituality is defined by the Interprofessional Spiritual Care Education Curriculum (ISPEC) as, “A dynamic and intrinsic aspect of humanity through which persons seek ultimate meaning, purpose, and transcendence and experience relationship to self, family, others, community, society, nature, and the significant or sacred.”[70] Spiritual needs and spirituality are often mistakenly equated with religion, but spirituality is a broader concept. Elements of spirituality include faith, meaning, love, belonging, forgiveness, and connectedness.[71] Spirituality and spiritual values in the context of nursing are closely intertwined with the concept of caring.[72] See Figure 18.1[73] for an illustration of spirituality.

An integrative review of nursing research and resources was completed in 2014 to describe the impact of spirituality and spiritual support in nursing.[74] See the following box for discussion of findings from this integrative review.
Integrative Review of Spirituality in Nursing[75]
An integrative review of nursing literature selected 26 articles published between 1999 and 2013 to describe the experiences of spirituality and the positive impact of spiritual support in nursing literature.[76] Spirituality was described as the integration of body, mind, and spirit into a harmonious whole (often referred to as holistic care). Spirituality was associated with the development of inner strength, looking into one’s own soul, believing there is more to life than worldly affairs, and trying to understand who we are and why we are on this earth.
Transcendence was described as an understanding of being part of a greater picture or of something greater than oneself, such as the awe one can experience when walking in nature. It was also expressed as a search for the sacred through subjective feelings, thoughts, and behaviors. Spirituality was found to have a positive effect on patients’ health and promoted recovery by viewing life from different perspectives and looking beyond one’s own anxiety to develop an understanding of illness and change.
Relationships and connectedness were also found to be powerful spiritual interventions that contributed to an individual’s spirituality. This included embracing, crying together, gift giving, having coffee together, and visiting each other. Laughter, happy thoughts, and the smiles of others were considered comforting. Being with others was described as a primary spiritual need, and conversation was unnecessary. Spirituality brought about the realization that the relationship with family and friends is important and involves finding a healthy balance in relationships among friends, family, society, and a higher power. Presence was the most influential element in positively influencing recovery. The presence of family and friends was a calming experience that brought forth comfort, peace, happiness, joy, acceptance, and hope.
Nurses facilitate their patients’ search for meaning by enabling them to express personal beliefs, as well as by supporting them in taking part in their religious and cultural practices. Furthermore, nurses assess and meet their patients’ spiritual needs by using active listening when talking, asking questions, and picking up patient cues. Active listening requires nurses to be fully present, especially when patients appear depressed or upset.
Nurses were found to use their own spirituality when helping patients achieve spiritual well-being. A desire to help others in need is an important part of spirituality, which is also described as discovering meaning and purpose in life and offering the gift of self to others. Helping others also brings a sense of self-worth, personal fulfilment, and satisfaction.
Spiritual Assessment
The Joint Commission requires that health care organizations provide a spiritual assessment when patients are admitted to a hospital. Spiritual assessment can include questions such as the following:
- Who or what provides you with strength or hope?
- How do you express your spirituality?
- What spiritual needs can we advocate for you during this health care experience?
In addition to performing a routine spiritual assessment on admission, nurses often notice other cues related to a patient’s spiritual distress or desire to enhance their spiritual well-being. When these cues are identified, spiritual care should be provided to relieve suffering and promote spiritual health. There are several nursing interventions that can be implemented, in addition to contacting the health care agency’s chaplain or the patient’s clergy member. See the “Applying the Nursing Process” section for a discussion of spiritual assessment tools and nursing interventions related to spiritual care.
Many hospitals, nursing homes, assisted living facilities, and hospices employ professionally trained chaplains to assist with the spiritual, religious, and emotional needs of patients, family members, and staff. In these settings, chaplains support and encourage people of all religious faiths and cultures and customize their approach to each individual’s background, age, and medical condition. Chaplains can meet with any individual regardless of their belief, or lack of belief, in a higher power and can be very helpful in reducing anxiety and distress. A nurse can make a referral for a chaplain without a provider order. See Figure 18.2[77] for an image of a hospital chaplain offering support to a patient.

A chaplain assists patients and their family members to develop a spiritual view of their serious illness, injury, or death, which promotes coping and healing. A spiritual view of life and death includes elements such as the following:
-
- Suffering occurs at physical, mental, emotional, and spiritual levels. Sociocultural factors, religious beliefs, family values and dynamics, and other environmental factors affect a person’s response to suffering.
- Hope is a desire or goal for a particular event or outcome. For example, some people may view dying as “hopeless” whereas a spiritual view can define hope as a “good death” when the patient dies peacefully according to the end-of-life preferences they previously expressed. Read more about the concept of a “good death” in the "Grief and Loss" chapter.
- Mystery is knowing there is truth beyond understanding and explanation.
- Peacemaking is the creation of a space for nurturing and healing.
- Forgiveness is an internal process releasing intense emotions attached to past incidents. Self-forgiveness is essential to spiritual growth and healing.
- Prayer is an expression of one's spirituality through a personalized interaction or organized form of petitioning and worship.
Now that we have discussed basic concepts and the nursing process related to the grieving process, let’s discuss more details regarding providing palliative care. Nurses provide palliative care whenever caring for patients with chronic disease. As the disease progresses and becomes end-stage, the palliative care they provide becomes even more important. As previously discussed, palliative care is “patient and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care occurs throughout the continuum of care and involves the interdisciplinary team collaboratively addressing physical, intellectual, emotional, social, and spiritual needs and facilitating patient autonomy, access to information, and choice.”[82]
Providing care at the end of life is similar for patients with a broad variety of medical diagnoses. It addresses multiple dimensions of care, including physical, psychological, social, and spiritual aspects:
- Physical: Functional ability, strength/fatigue, sleep/rest, nausea, appetite, constipation, and pain
- Psychological: Anxiety, depression, enjoyment/leisure, pain, distress, happiness, fear, and cognition/attention
- Social: Financial burden, caregiver burden, roles/relationships, affection, and appearance
- Spiritual: Hope, suffering, the meaning of pain, religiosity, and transcendence[83]
The interdisciplinary team manages pain and other symptoms, assists with difficult medical decisions, and provides additional support to patients, family members, and caregivers. Nurses have the opportunity to maintain hope for patients and family members by providing excellent physical, psychosocial, and spiritual palliative care. Nursing interventions begin immediately after the initial medical diagnosis and continue throughout the continuum of care until the end of life. As a patient approaches end-of-life care, nursing interventions include the following:
- Eliciting the patient’s goals for care
- Listening to the patient and their family members
- Communicating with members of the interdisciplinary team and advocating for the patient’s wishes
- Managing end-of-life symptoms
- Encouraging reminiscing
- Facilitating participating in religious rituals and spiritual practices
- Making referrals to chaplains, clergy, and other spiritual support[84]
While providing palliative care, it is important to remain aware that some things cannot be “fixed”:
- We cannot change the inevitability of death.
- We cannot change the anguish felt when a loved one dies.
- We must all face the fact that we, too, will die.
- The perfect words or interventions rarely exist, so providing presence is vital.[85]
The Palliative Care Network of Wisconsin contain excellent resources for nurses providing care for seriously ill patients.
View the "Fast Facts" page for extensive information about palliative care and end of life topics.
Management of Common Symptoms
Many patients with serious, life-limiting illnesses have common symptoms that the nurse can assess, prevent, and manage to optimize their quality of life. These symptoms include pain, dyspnea, cough, anorexia and cachexia, constipation, diarrhea, nausea and vomiting, depression, anxiety, cognitive changes, fatigue, pressure injuries, seizures, and sleep disturbances. Good symptom management improves quality of life and functioning at all states of chronic illness. Nurses play a critical role in recognizing these symptoms and communicating them to the interdisciplinary team for optimal management. The plan of care should always be based on the patient’s goals and their definition of quality of life.[86] These common symptoms are discussed in the following subsections.
Pain
Pain is frequently defined as “whatever the experiencing person says it is, existing whenever he says it does.”[87] When a patient is unable to verbally report their pain, it is important to assess nonverbal and behavioral indicators of pain. The goal is to balance the patient’s desire for pain relief, along with their desire to manage side effects and oversedation. There are many options available for analgesics. Reassure a patient that reaching their goal of satisfactory pain relief is achievable. Read more about pain management in the “Comfort” chapter. See Figure 17.19[88] for an image illustrating a patient experiencing pain.

Dyspnea
Dyspnea is a subjective experience of breathing discomfort and is the most reported symptom by patients with life-limiting illness. Dyspnea can be extremely frightening. Assessing dyspnea can be challenging because the patient’s respiratory rate and oxygenation status do not always correlate with the symptom of breathlessness.[89] See Figure 17.20[90] for an image of a patient experiencing dyspnea.

When assessing dyspnea, include the following components:
- Ask the patient to rate the severity of their breathlessness on a scale of 0-10
- Assess their ability to speak in sentences, phrases, or words
- Assess the patient’s anxiety
- Observe respiratory rate and effort
- Measure oxygenation status (i.e., pulse oximetry or ABG)
- Auscultate lung sounds
- Assess for the presence of chest pain or other pain
- Assess factors that improve or worsen breathlessness
- Evaluate the impact of dyspnea on functional status and quality of life[91]
If you suspect that new dyspnea is caused by an acute condition, report assessment findings immediately to a health care provider. However, in end-stage disease, dyspnea can be a chronic condition that is treated with pharmacological and nonpharmacological management. Relatively small doses of opioids can be used to improve dyspnea while having little impact on their respiratory status or a patient’s life expectancy. The dosage should be titrated to the patient’s desired goals for relief of dyspnea without over sedation.
Nonpharmacological interventions for dyspnea include pursed-lip breathing, energy conservation techniques, fans and open windows to circulate air, elevation of the patient bed, placing the patient in a tripod position, and relaxation techniques such as music and a calm, cool environment. Patient education can also reduce anxiety.[92] Read more about nonpharmacological interventions for dyspnea in the “Oxygenation” chapter.
Cough
A cough can be frustrating and debilitating for a patient, causing pain, fatigue, vomiting, and insomnia. See Figure 17.21[93] for an image of a patient with a chronic cough. Coughing is frequently present in advanced diseases such as chronic obstructive pulmonary disease (COPD), heart failure (HF), cancer, and AIDS. There are several potential causes of a cough. Medications that can be used to control a cough are opioids, dextromethorphan, and benzonatate. Guaifenesin can be used to thin thick secretions, and anticholinergics (such as scopolamine) can be used for high-volume secretions.

Anorexia and Cachexia
Anorexia (loss of appetite or loss of desire to eat) and cachexia (wasting of muscle and adipose tissue due to lack of nutrition) are commonly found in advanced disease. See Figure 17.22[94] for an image of a patient with cachexia. Weight loss is present in both conditions and is associated with decreased survival. Unfortunately, aggressive nutritional treatment does not improve survival or quality of life and can actually create more discomfort for the patient.[95]

Assessment of anorexia and cachexia focuses on understanding the patient’s experience and concerns, as well as determining potentially reversible causes. Referral to a dietician may be needed. Read more about nutritional assessment in the “Nutrition” chapter.
Interventions for anorexia and cachexia should be individualized for each patient with the goal being eating for pleasure for those at the end of life. Patients should be encouraged to eat their favorite foods, as well as select foods that are high in calories and easy to chew. Small, frequent meals with pleasing food presentation are important. Family members should be aware that odors associated with cooking can inhibit eating. The patient may need to be moved away from the kitchen or cooking times separated from eating times.[96]
Medication may be prescribed to increase intake, such as mirtazapine or olanzapine. Prokinetics such as metoclopramide may be helpful in increasing gastric emptying. Medical marijuana or dronabinol may also be useful. In some cases, enteral nutrition is helpful for patients who continue to have an appetite but cannot swallow.[97]
Patient and family member education about anorexia at the end of life is important. Nurses should be aware that many family members perceive eating as a way to “get better” and are distressed to see their loved one not eat. After listening respectfully to their concerns, explain that the patient may feel more discomfort when forcing themselves to eat.
Constipation
Constipation is a frequent symptom in many patients at the end of life for many factors, such as low intake of food and fluids, use of opioids, chemotherapy, and impaired mobility. Constipation is defined as having less than three bowel movements per week. The patient may experience associated symptoms such as rectal pressure, abdominal cramps, bloating, distension, and straining. See Figure 17.23[98] for an image of a patient experiencing constipation.

The goal is to establish what is considered normal for each patient and to have a bowel movement at least every 72 hours regardless of intake. Treatment includes a bowel regimen such as oral stool softeners (i.e., docusate) and a stimulant (i.e., sennosides). Rectal suppositories (i.e., bisacodyl) or enemas should be considered when oral medications are not effective or the patient can no longer tolerate oral medications.[99]
Read more about managing constipation in the “Elimination” chapter.
Diarrhea
Diarrhea is defined as having more than three unformed stools in 24 hours. Diarrhea can be especially problematic for patients receiving chemotherapy, pelvic radiation, or treatment for AIDS. It can cause dehydration, skin breakdown, and electrolyte imbalances and dramatically affect a person’s quality of life. It can also be a huge burden for caregivers.[100]
Early treatment of diarrhea includes promoting hydration with water or fluids that improve electrolyte status (i.e., sports drinks). Intravenous fluids may be required based on the patient’s disease stage and goals for care. Medications such as loperamide, psyllium, and anticholinergic agents may also be prescribed.
Read more about managing diarrhea in the “Elimination” chapter.
Nausea and Vomiting
Nausea is common in advanced disease and is a dreaded side effect of many treatments for cancer. Assessment of nausea and vomiting should include the patient’s history, effectiveness of previous treatment, medication history, frequency and intensity of episodes of nausea and vomiting, and activities that precipitate or alleviate nausea and vomiting.[101]
Nonpharmacological interventions for nausea include eating meals and fluids at room temperature, avoiding strong odors, avoiding high-bulk meals, using relaxation techniques, and listening to music therapy.[102] Antiemetic medications, such as prochlorperazine and ondansetron, may be prescribed.
Read more information about managing nausea in the “Antiemetics” section of the Gastrointestinal chapter in Open RN Nursing Pharmacology.
Depression
Patients who have a serious life-threatening illness will normally experience sadness, grief, and loss, but there is usually some capacity for pleasure. Persistent feelings of helplessness, hopelessness, and suicidal ideation are not considered a normal part of the grief process and should be treated. Undertreated depression can cause a decreased immune response, decreased quality of life, and decreased survival time. Evaluation of depression requires interdisciplinary assessment and referrals to social work and psychiatry may be needed.[103]
Antidepressants such as serotonin selective reuptake inhibitors (i.e., fluoxetine, paroxetine, sertraline, or citalopram) are generally prescribed as first-line treatment of depression. Other medication may be prescribed if these medications are not effective.
Nonpharmacological interventions for depression may include the following:
- Promoting and facilitating as much autonomy and control as possible
- Encouraging patient and family participation in care, thus promoting a sense of control and reducing feelings of helplessness
- Reminiscing and life review to focus on life accomplishments and to promote closure and resolution of life events. See Figure 17.24[104] for an image of reminiscing with pictures.
- Grief counseling to assist patients and families in dealing with loss
- Maximizing symptom management
- Referring to counseling for those experiencing inability to cope
- Assisting the patient to draw on previous sources of strength, such as faith, religious rituals, and spirituality
- Referring for cognitive behavioral techniques to assist with reframing negative thoughts into positive thoughts
- Teaching relaxation techniques
- Providing ongoing emotional support and “being present”
- Reducing isolation
- Facilitating spiritual support[105]

A suicide assessment is critical for a patient with depression. It is important for nurses to ask questions, such as these:
- Do you have interest or pleasure in doing things?
- Have you had thoughts of harming yourself?
- If yes, do you have a plan for doing so?
To destigmatize the questions, it is helpful to phrase them in the following way, “It wouldn’t be unusual for someone in your circumstances to have thoughts of harming themselves. Have you had thoughts like that?" Patients with immediate, precise suicide plans and resources to carry out this plan should be immediately evaluated by psychiatric professionals.[106]
Anxiety
Anxiety is a subjective feeling of apprehension, tension, insecurity, and uneasiness, usually without a known specific cause. It may be anticipatory. It is assessed along a continuum as mild, moderate, or severe. Patients with life-limiting illness will experience various degrees of anxiety due to various issues such as their prognosis, mortality, financial concerns, uncontrolled pain and other symptoms, and feelings of loss of control.[107]
Physical symptoms of anxiety include sweating, tachycardia, restlessness, agitation, trembling, chest pain, hyperventilation, tension, and insomnia. Cognitive symptoms include recurrent and persistent thoughts and difficulty concentrating. See Figure 17.25[108] for an illustration of anxiety.

Benzodiazepines (i.e., lorazepam), may be prescribed to treat anxiety. However, the nurse should assess for adverse effects such as oversedation, falls, and delirium, especially in the frail elderly.
Nonpharmacological interventions are crucial and include the following:
- Maximizing symptom management to decrease stressors
- Promoting the use of relaxation and guided imagery techniques, such as breathing exercises, progressive muscle relaxation, and the use of audiotapes
- Referring for psychiatric counseling for those unable to cope with the experience of their illness
- Facilitating spiritual support by contacting chaplains and clergy
- Acknowledging patient fears and using open-ended questions and active listening with therapeutic communication
- Identifying effective coping strategies the patient has used in the past, as well as teaching new coping skills such as as relaxation and guided imagery techniques
- Providing concrete information to eliminate fear of the unknown
- Encouraging the use of a stress diary that helps the patient understand the relationship between situations, thoughts, and feelings[109]
Cognitive Changes
Delirium is a common cognitive disorder in hospitals and palliative care settings. Delirium is an acute change in cognition and requires urgent management in inpatient care. Up to 90% of patients at the end of life will develop delirium in their final days and hours of life. Early detection of delirium can cause resolution if the cause is reversible.[110]
Symptoms of delirium include agitation, confusion, hallucinations, or inappropriate behavior. It is important to obtain information from the caregiver to establish a mental status baseline. The most common cause of delirium at end of life is medication, followed by metabolic insufficiency due to organ failure.[111]
Medications such as neuroleptics (i.e., haloperidol and chlorpromazine) or benzodiazepines may be prescribed. It is also important to remember that delirium can be related to opioid toxicity. It may be helpful to request the presence of family to reorient the patient, as well as provide nonpharmacological interventions such as massage, distraction, and relaxation techniques.[112]
Read more about delirium in the “Cognitive Impairments” chapter.
Fatigue
Fatigue has been cited as the most disabling condition for patients receiving a variety of treatments in palliative care. Fatigue is defined as a distressing, persistent, subjective sense of physical, emotional, and/or cognitive tiredness or exhaustion that is not proportional to activity and interferes with usual functioning.[113] See Figure 17.26[114] for an image of an older patient experiencing fatigue.

The primary cause of fatigue is metabolic alteration related to chronic disease, but it can also be caused by anemia, infection, poor sleep quality, chronic pain, and medication side effects. Nonpharmacological interventions include energy conservation techniques.
Pressure Injuries
Patients at end of life are at risk for quickly developing pressure injuries, formerly referred to as pressure ulcers. Prevention is key and requires interventions such as promoting mobility, reducing moisture, and encouraging nutrition as appropriate.
The Kennedy Terminal Ulcer is a type of pressure injury that some patients develop shortly before death resulting from multiorgan failure. It usually starts on the sacrum and is shaped like a pear, butterfly, or horseshoe. It is red, yellow, black, or purple in color with irregular borders and progresses quickly. For example, the injury may be identified by a nurse at the end of a shift who says, “That injury was not present when I assessed the patient this morning.”[115]
Read more about assessing, preventing, and treating pressure injuries in the “Integumentary” chapter.
Seizures
Seizures are sudden, abnormal, excessive electrical impulses in the brain that alter neurological functions such as motor, autonomic, behavioral, and cognitive function. A seizure can be caused by infection, trauma, brain injury, brain tumors, side effects of medications, metabolic imbalances, drug toxicities, and withdrawal from medications.[116]
Seizures can have gradual or acute onset and include symptoms such as mental status changes, motor movement changes, and sensory changes. Treatment is focused on prevention and limiting trauma that occur during the seizure. Medications may be prescribed such as phenytoin, phenobarbital, benzodiazepines, or levetiracetam.[117]
Sleep Disturbances
Sleep disturbances affect quality of life and can cause much suffering. It can be caused by poor pain and symptom management, as well as environmental disturbances. Nurses can promote improved sleep for inpatients by creating a quiet, calm environment, promoting sleep routines, and advocating for periods of uninterrupted rest without disruptions by the health care team.
Read more about promoting good sleep in the “Sleep and Rest” chapter.
Recognizing approaching death allows the patient, family members, and interdisciplinary team to prepare for the actively dying phase. The nurse has two primary responsibilities at this time: providing symptom management and preparing the family for what to expect as death is approaching. Nurses also have additional responsibilities regarding organ donation, postmortem care, and facilitating arrangements.
It is essential for nurses to ensure that patients and their family members have access to the interdisciplinary team in the final days before death. Developmentally appropriate education should be provided to the patient, family, and/or other caregivers about what to expect during the final hours of life, as well as immediately following the patient’s death. Early access to hospice support should be facilitated whenever possible to optimize care outcomes for the patient and the family.[118]
Nurses have a responsibility to carry out and respect the patient's wishes to the extent they can. Each individual patient is different, and what works best for one patient might not work well for another. Dying is a multifaceted process that is unique to every patient. Providing a “good death” for patients means respecting their preferences and offering support for them and their family.
The nurse assumes multiple roles of advocate, professional caregiver, educator, and supporter and is frequently the one to facilitate a dignified death no matter the setting where death occurs. Nurses must be comfortable in “providing presence” and “bearing witness” with dying patients and their families. Rhythms of care (i.e., vital signs and routine assessments) often change during these final hours; be aware if these actions provide comfort or are burdens causing discomfort.[119]
Avoid overwhelming the family with too much medical jargon. Provide simple answers in accordance with the patient’s and family’s understanding and readiness for responses. Family members may be tired, emotional, and have difficulty concentrating. Because they may be in crisis and unable to retain much information, you may need to answer the same questions or provide the same information repeatedly.[120] It is helpful to provide family members written resources about what to expect. A commonly used resource in hospice care that can be very comforting for family members is Gone From My Sight: The Dying Experience. It is an inexpensive resource available to order online if it is not available at your facility.
There is no typical death. Each person dies in their own way, at their own time, with their own beliefs and values, and with unique relationships with family, friends, and significant others. Many people experience similar psychological and emotional responses during this time, such as fear of the dying process, fear of abandonment, fear of the unknown, nearing death awareness, and withdrawal. The nurse is essential in addressing patient’s fears and managing their symptoms according to their preferences.
Managing Common Symptoms During the Dying Process
Most patients experience the dying process as a natural slowing down of physical and mental processes. Two roads to death have often been described. One road involves sedation and lethargy leading to a comatose state and death. Another road involves confusion, restlessness, muscle jerks, seizures, and death.[121]
Pain and Dyspnea
During the final hours of life, changes in level of consciousness can make assessment and management of pain challenging. Consider behavioral cues such as grimacing and posturing, as well as previous pain issues. Some patients also demonstrate signs of increased dyspnea, commonly referred to as “air hunger,” with labored and increased work of breathing.
Pain pumps may be used to relieve severe pain, especially cancer-related pain. Medication can also be administered orally, even up to the last hours of life, for pain and dyspnea.[122] For example, Roxanol is a highly concentrated solution of morphine sulfate that can be administered sublingually for pain and/or air hunger. The typical dosage is 20 mg/mL. Morphine not only relieves pain, but also is used to relax respiratory muscles and improve air exchange to relieve air hunger. However, the nurse should always balance providing analgesia with the patient’s goal for maintaining alertness.
Principle of Double Effect
Nurses and family members may be hesitant to administer morphine in the last few hours of life, fearing that it may hasten death, yet also not wanting to see the patient suffer. The American Nurses Association and the Palliative Care Nurses Association support the nurse in this dilemma that is often referred to as the Rule of Double Effect. If the intent is good (i.e., relief of pain and suffering), then the act is morally justifiable even if it causes an unintended result of hastening death. Thus, the nurse should provide pain relief, without fear of sedation or respiratory depression that typically limits the administration of opioids, in the final days and hours of a patient’s life.[123]
Terminal Secretions
Terminal secretions, commonly known as the “death rattle,” can be a distressing and frightening symptom for family members and those involved in the patient’s care. Terminal secretions are usually observed 3-23 hours before death. Anticholinergic medications, such as atropine or scopolamine, can be used to dry the secretions. It is also helpful to reposition the patient on their side, if feasible. Suctioning is not recommended because it is not typically effective for these types of secretions and can cause increased agitation and distress in the patient. Family members caring for patients at home under hospice care should be warned about this phenomenon and instructed about potential treatment.[124]
View a supplementary video (11 minutes) on Lessons from a hospice nurse: Alia Indrawan at TEDxUbud.[125]
Phases of Dying
There are typically four phases that a person progresses through when dying. These phases include actively dying, transitioning, imminent death, and death.
Actively Dying
A patient in this phase will experience symptoms such as pain, dyspnea, fatigue, cough, incontinence, nausea and vomiting, depression, anxiety, and seizures. Treatments during this phase are focused on symptom management and emotional support to both the patient and the family. Read more about symptom management in the “Palliative Care Management” section of this chapter.
Educating the family and patient on what to expect is essential. Include written materials and progressive education as the patient’s condition changes. It is often helpful to provide guidance to the family in anticipation of upcoming phases of dying.
Transitioning
This is the phase between actively dying and imminent death where the patient withdraws physically. The patient begins to demonstrate decreased interest in activities of life with less frequent interactions with others and often has hallucinations. Other signs of this phase include hypoxia and acidosis. It is important for the nurse to keep the patient's environment as comfortable as possible, such as keeping lights low and minimizing alarms and other noises.
Imminent
Death will occur at any point during the imminent phase due to multisystem organ failure. This phase usually occurs within 24 hours before death with common, recognizable signs. See Table 17.5 for typical signs that occur during this stage and indicate that death is imminent.
Table 17.5 Typical Signs as Death Becomes Imminent
| System | Signs |
|---|---|
| Cardiovascular | Cool, clammy skin; mottled extremities; rapid or irregular pulse |
| Musculoskeletal | Inability to ambulate, move, or turn in bed |
| Neurological | Confusion, restlessness, increased lethargy, hallucinations |
| Respiratory | Increased respiratory rate, inability to clear secretions, Cheyenne-Stokes respirations, noisy breathing (i.e., terminal secretions) |
| Urinary | Decreased or dark urine output |
During this stage, the family often requires additional support from the nurse as death becomes more of a reality. Vital signs are usually no longer assessed because they do not provide a benefit for the patient. The nurse should offer support by encouraging reminiscence, calming music, touch, light massage, presence, and prayer (according to family preferences) as the patient begins their transition.
The dying process is variable for each individual. Families often ask for a definitive time frame when death will occur. Although these signs that indicate progression within 24 hours, a specific time line cannot be predicted. Some patients seem to instinctively know when death will occur.
Be aware of religious practices and beliefs that are sacred to the patient and/or their family members at this time. Provide spiritual comfort through presence and prayer (based on patient preferences and the nurse's comfort level). Call the agency chaplain and/or the patient's clergy as indicted. (Read more about chaplains in the "Spirituality" chapter.) Encourage family members to bring in favorite hymns, scriptures, or symbols (i.e., a rosary) so the patient can experience these spiritual comforts through different senses (hearing, seeing, touching).[126]
Consider coaching family members about the five tasks that may serve as parting words with their loved one:
- To ask forgiveness
- To forgive
- To say “Thank you”
- To say “I love you”
- To say “Goodbye”
Read more about parting tasks in the book by Ira Byock, M.D. titled The Four Things That Matter Most.[127]
Death Vigil by Family Members
Family members have historically desired to be at the patient’s bedside during the days to hours before death. See Figure 17.27[128] for artwork depicting the death vigil by family members when George Washington died.
Family members have common fears, such as the following:
- The patient being alone when they die
- Not knowing how to react or what to do
- Watching the patient suffer
- Not knowing if the patient has died
- Giving the “last dose” of medication at home and inadvertently causing death
It is important for the nurse to address family members’ fears proactively and provide education and support.
Death and Postmortem Care
Clinical death occurs when blood circulation ceases, the heart stops beating, and respirations stop. Within 4-6 minutes of clinical death, CPR can be performed to attempt resuscitation. However, because most patients receiving palliative or hospice care have Do Not Resuscitate (DNR) orders in place, CPR is not performed. After this time window, brain cells die from lack of oxygen, followed by death of cells in other organs. This is called biological death. Rigor mortis, stiffening of muscles, will begin to set in several hours following death and be at its peak 12-18 hours following death. Rigor mortis disappears 48 hours following death. The nurse should listen to the apical heartbeat for one full minute to ensure and document that death has occurred.
When a resident or patient passes away, the nurse should perform and document a final nursing assessment that includes the following:
- Date and time of the assessment
- Patient name
- Time of physician contact
- Individuals present at time of death (i.e., family members, friends)
- Lack of response to stimuli
- Absence of apical pulse
- Arrangement for transport to the morgue or funeral home
Care following a patient’s death requires sensitivity for the dignity of the deceased, as well as time for the care of family members. Following the death pronouncement, family members may feel numb and confused about what to do next. In a quiet and private place, explain the process for care of the body immediately following death.[129]
Following death, medical supplies and equipment tubes should be removed unless a coroner must approve of such measures. The goal is to provide a more personal closure experience for the family, leaving them memories of the deceased as a loved one rather than as a patient. Bathing, dressing, and positioning the body show respect and provide dignity for the patient and family. Position the body in proper alignment and place dentures in the mouth. Place dressings on leaking wounds and apply incontinence products as needed. Remember to honor cultural practices regarding care of the body after death and who should provide that care.[130]
The nurse should continue to provide support for the family and offer assistance as needed, such as contacting other family members to inform them of the death. Some family members may want to take pictures, comb their loved one’s hair, wash their face, hold their hand, kiss them, or crawl into bed and hold them. Support families in their various ways of saying goodbye.
Ask if the family completed preplanning for burial or cremation, but do not rush their final visit. In some cases, families will not have had time for making prearrangements. If they have made prearrangements, contact the funeral home. Be aware of county and agency policies that require notification of the local coroner prior to calling the funeral home.[131] When burial is chosen, the body will be embalmed, which is removing blood from the body and replacing it with an embalming solution that contains formaldehyde and other chemicals. The embalming process temporarily preserves the body to be shown at a funeral or memorial service. Cremation is the process of using heat to reduce the body to ashes that can be placed in a container called an urn. In some cultures, cremation is an ancient tradition. Depending on the family’s cultural beliefs and preferences, the ashes may be buried, placed in a mausoleum, or kept at home in an urn. See Figure 17.28[132] for an image of a burial in a memorial garden.

In hospital settings, there may be a sense of urgency to get the room cleared as soon as possible so that another patient can be admitted. However, the nurse should advocate for the patient and make arrangements so the family does not feel rushed.[133] After the family has said their goodbyes and left the room, it is the nurses responsibility to ensure identification tags are applied to the body and the patient is moved to the morgue.
Organ Donation
If the patient is an organ or tissue donor, follow procedures as planned and in accordance with state and care setting guidelines, policies, and procedures. The patient's drivers license may have information about their organ donation wishes. Federal law and Medicare regulations mandate that hospitals give surviving family members the chance to authorize donation of their loved one’s organs and tissues. Many family members feel consolation in helping others through organ donation despite their own loss. There is no cost for organ or tissue donation.
This section will summarize the steps of the nursing process when caring for a patient who is actively dying and their family members.
Assessment
Assessments are generally limited for those patients at the end of life with the overall treatment goal of providing comfort. The goal in any performed assessment is to help ease the patient’s discomfort as the body begins to fail and facilitate a peaceful transition. If end-of-life care is occurring within the hospital setting, the nurse may need to remind members of the care team that “normal” care routines are not required. This may include collection of vital signs, intake and outputs, laboratory blood draws, and full physical assessment. It can feel challenging to switch modes of care in the inpatient setting where so many of our actions are focused on intervention and restoring a patient to health. However it is important to remember that our interventions take a different, but no less important, form. Providing comfort care at the end of life is one of the most important interventions a nurse can do to help ease patient and family suffering.
Subjective Assessment
Many individuals at the end of life may be nonverbal. Some may experience times of reminiscence as they progress toward death. It is important for the nurse to inform the family that communication can be quite variable as the patient progresses toward death, but the sense of hearing may still be intact. Family members and friends should be encouraged to share their thoughts and feelings with the patient, taking time to relate stories of comfort and feelings to the patient. This can be a therapeutic exchange for both the patient and the family.
Objective Assessment
Physical assessments should be limited and focused on providing patient comfort and creating a supportive environment for a therapeutic transition. Signs of pain such as grimacing, moaning, furrowing brow, and physical guarding should be noted and addressed. Many patients may experience increased respirations, labored breathing, and increased secretions that produce an audible respiratory “rattle.” The patient typically has a significant decline in circulation as they progress towards death, evidenced by cool and clammy skin, mottled extremities, and diminished pulses. The nurse should continue to monitor for signs of skin breakdown and urinary retention.
Notify the provider of unexpected findings on assessment, such as severe pain not relieved by pain management protocol, acute labored breathing, terminal secretions, or urinary retention resulting in bladder distention.
Diagnosis
As the patient progresses toward death, diagnosis statements are focused on provision of comfort for the patient. Identification of acute pain and ineffective breathing are areas that typically become priority as patients near their final transition. Additionally, attention to family coping and caregiver role strain remain areas of focus as the nurse assists family members in coping with the dying process.
When planning care, review a nursing care planning source for current NANDA-I approved nursing diagnoses and evidence-based nursing interventions. See Table 17.6 for the definition and defining characteristics regarding the NANDA-I diagnosis Death Anxiety.[134]
Table 17.6 NANDA-I Nursing Diagnoses Death Anxiety[135]
| NANDA-I Diagnosis | Definition | Defining Characteristics |
|---|---|---|
| Death Anxiety | Vague, uneasy feeling of discomfort or dread generated by perceptions of a real or imagined threat to one’s existence. |
|
Outcomes
An overall goal for a patient who is actively dying is, The patient will experience dignified life closure as evidenced by:
- Expression of readiness for death
- Resolution of important issues
- Sharing of feelings about dying
- Discussion regarding spiritual concerns[136]
An example of a SMART outcome for a patient actively dying is, “The patient will express their fears associated with dying by the end of the shift.”[137]
Nursing goals for care focus on the provision of comfort. For example, a common nursing goal is, “The patient will experience adequate pain management based on their expressed goals for pain relief and alertness.”
Planning and Implementing Interventions
Many patients require pain medications to assist with a therapeutic transition as they near death. These medications often include morphine and lorazepam to help ease pain, dyspnea, and anxiety. It is important for the nurse to be conscientious of the appropriateness of the medication’s route of administration, recognizing that patient condition can change rapidly. Concentrated oral solutions are absorbed through the buccal membranes, but if pain management needs are high, it may be necessary to contact the provider regarding a subcutaneous pump. Many patients in the imminent phase have terminal secretions so anticholinergic medications such as atropine or scopolamine may be administered. See the following box for a summary of other nursing interventions in the last days and hours of a patient’s life.
Interventions in the Last Days and Hours of Life[138]
- Honor the patient’s preferences for end-of-life care.
- Be respectful of the environment. Physical assessment and cares should be provided with the utmost respect and attention to comfort. Shielding the patient from harsh light or loud voices is encouraged to help provide a respectful environment.
- Reinforce the steps of the dying process so that family remains cognizant of what to expect. Although this can feel redundant, this conversation and anticipatory planning are very helpful due to the emotional nature of the situation and challenges that they may experience with information retention.
- Be present and attentive. Use active empathetic listening.
- Encourage the family to create a quiet and comfortable environment.
- Assess the patient for pain and provide pain relief measures based on their preferences.
- Assess the patient for fears related to death.
- Assist the patient with life review and reminiscence.
- Provide music of the patient’s choosing.
- Provide social support for families and guide them through end-of-life issues.
- Recognize the spiritual needs of the patient and their family members. Support religious beliefs, rituals, and prayer.
- Encourage family members to be physically close to their loved one and give them permission to touch them.
- When death occurs, allow appropriate time for closure. Provide information regarding the next steps of physical care and transporting the patient.
Evaluation
It is always important to evaluate the effectiveness of interventions based on the outcome criteria established for each patient. The nurse should closely monitor for escalating signs of patient discomfort that is not managed by the current treatment plan. It is helpful to educate the family regarding whom to contact if additional concerns arise.

