Diverse Patients
3.5 Health Disparities
Despite decades of promoting cultural competent care and the Patient’s Bill of Rights, disparities in health care continue. Vulnerable populations continue to experience increased prevalence and burden of diseases, as well as problems accessing quality health care. In 2003 the Institute of Medicine (IOM) published Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, sharing evidence that “bias, prejudice, and stereotyping on the part of health care providers may contribute to differences in care.”[1] The health care system in the United States was shaped by the values and beliefs of mainstream white culture and originally designed to primarily serve English-speaking patients with financial resources.[2] In addition, most health care professionals in the United States are members of the white culture and medical treatments tend to arise from that perspective.[3],[4]
The term health disparities describes the differences in health outcomes that result from social determinants of health. Social determinants of health are conditions in the environment where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes. Resources that enhance quality of life can have a significant influence on population health outcomes. Examples of resources include safe and affordable housing, access to education, public safety, availability of healthy foods, local emergency/health services, and environments free of life-threatening toxins.[5]
Vulnerable populations experience increased prevalence and burden of diseases, as well as problems accessing quality health care because of social determinants of health. Health disparities negatively impact groups of people based on their ethnicity, gender, age, mental health, disability, sexual orientation, gender identity, socioeconomic status, geographic location, or other characteristics historically linked to discrimination or exclusion.[6] A related term is health care disparity that refers to differences in access to health care and insurance coverage. Health disparities and health care disparities can lead to decreased quality of life, increased personal costs, and lower life expectancy. More broadly, these disparities also translate to greater societal costs, such as the financial burden of uncontrolled chronic illnesses.
The Agency for Healthcare Research and Quality (AHRQ) releases an annual National Healthcare Quality and Disparities Report that provides a comprehensive overview of the quality of health care received by the general U.S. population and disparities in care experienced by different racial and socioeconomic groups. Quality is described in terms of patient safety, person-centered care, care coordination, effective treatment, healthy living, and care affordability.[7] Although access to health care and quality have improved since 2000 in the wake of the Affordable Care Act (ACA), the 2019 report shows continued disparities, especially for poor and uninsured populations:
- For about 40% of quality measures, Blacks, African Americans, and Alaska Natives received worse care than Whites. For more than one third of quality measures, Hispanics received worse care than Whites.
- For nearly a quarter of quality measures, residents of large metropolitan areas received worse care than residents of suburban areas. For one third of quality measures, residents of rural areas received worse care than residents of suburban areas.[8]
There are several initiatives and agencies designed to combat the problem of health disparities in the United States. See Table 3.5 for a list of hyperlinks to available resources to combat health disparities.
Table 3.5 Resources to Combat Health Disparities
| AHRQ publishes the National Healthcare Quality and Disparities Report, a report on measures related to access to care, affordable care, care coordination, effective treatment, healthy living, patient safety, and person-centered care. | |
| A new Healthy People initiative is launched every ten years. The initiative guides national health promotion and disease prevention efforts to improve the health of the nation. | |
| The mission of the Office of Minority Health is to improve the health of minority populations and to act as a resource for health care providers. The Office of Minority Health has published National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care (CLAS). | |
|
Racial and Ethnic Approaches to Community Health Across the United States (REACH-US) |
This initiative, overseen by the Centers for Disease Control (CDC), seeks to remove barriers to health linked to race or ethnicity, education, income, location, or other social factors. |
|
National Partnership for Action to End Health Disparities (NPA) |
The mission of the NPA is to raise awareness and increase the effectiveness of programs targeting health disparities. |
| RWJF is a philanthropic organization with the goal of identifying the root causes of health disparities and removing barriers to improve health outcomes. | |
| The nonprofit Sullivan Alliance was formed to increase the numbers of ethnic and racial minorities within the health professions to raise awareness about health disparities and to develop partnerships between academia and the health professions. | |
|
Transcultural Nursing Society – Many Cultures One World (TCNS) |
The mission of TCNS is to improve the quality of culturally congruent and equitable care for people worldwide by ensuring cultural competence in nursing practice, scholarship, education, research, and administration. |
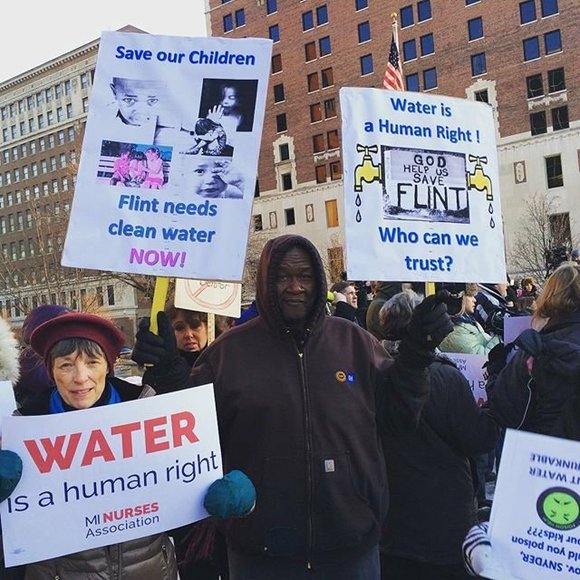
See the following box for an example of nurses addressing a community health care disparity during the water crisis in Flint, Michigan.
Nurses Addressing the Flint Michigan Water Crisis[9]
In 2014 the water system in Flint, Michigan, was discovered to be contaminated with lead. The city’s children were found to have perilously elevated lead levels. Children from poor households were most affected by the crisis. Lead is a dangerous neurotoxin. Elevated lead levels are linked to slowed physical development; low IQ; problems with cognition, attention, and memory; and learning disabilities.
In Flint approximately 150 local nurses and nursing students answered the call, organizing and arranging educational seminars, as well as setting up lead testing clinics to determine who had been affected by the water contamination. A nursing student involved in the effort told CBS Detroit that this situation has illustrated that “the need for health care, the need for nursing, goes way outside the hospital walls.” See Figure 3.5[10] for an image of the water crisis in Flint, Michigan.
Reflective Questions
- What factors led to the children from poor households being so adversely harmed by this crisis?
- What are ways that you as a future nurse can make a difference for vulnerable or marginalized people?
Providing culturally responsive care is a key strategy for reducing health disparities.[11] While there are multiple determinants contributing to a person’s health, nurses play an important role in reducing health disparities by providing a culturally sensitive environment, performing a cultural assessment, and providing culturally responsive care. These interventions will be further discussed in the following sections. On the other hand, a lack of culturally responsive care potentially contributes to miscommunication between the patient and the nurse. The patient may experience distress or loss of trust in the nurse or the health care system as a whole and may not adhere to prescribed treatments. Nurses are uniquely positioned to directly impact patient outcomes as we become more aware of unacceptable health disparities and work together to overcome them.[12]
- Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Smedley, B. D., Stith, A. Y., Nelson, A. R. (Eds.). (2003). Unequal treatment: Confronting racial and ethnic disparities in health care. National Academies Press. https://doi.org/10.17226/12875 ↵
- Meedzan, N. (2015). Cultural immersion experiences in nursing education. In S. Breakey, I. Corless, N. Meedzan, & P. Nicholas (Eds.) Global nursing in the 21st century. Springer. pp. 441-452. ↵
- Hart, P. L., & Mareno, N. (2016). Nurses’ perceptions of their cultural competence in caring for diverse patient populations. Online Journal of Cultural Competence in Nursing & Healthcare, 6(1), 121–137. https://doi.org/10.9730/ojccnh.org/v6n1a10 ↵
- Ong-Flaherty, C. (2015). Critical cultural awareness and diversity in nursing: A minority perspective. Nurse Leader, 13(5), 58-62. http://dx.doi.org/10.1016/j.mnl.2015.03.012 ↵
- Healthy People 2020. (2020). Social Determinants of Health. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health ↵
- U.S. Department of Health and Human Services. Healthy People 2020. Lesbian, gay, bisexual, and transgender health. https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bisexual-and-transgender-health ↵
- Agency for Healthcare Research and Quality. (2020). 2019 National healthcare quality and disparities report. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr19/index.html ↵
- Agency for Healthcare Research and Quality. (2020). 2019 National healthcare quality and disparities report. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr19/index.html ↵
- Householder, M. (2016, April 12). Health workers get lead-test help from Flint student nurses. Associated Press. https://detroit.cbslocal.com/2016/04/12/health-workers-get-lead-test-help-from-flint-student-nurses/. ↵
- “Flint_Water_Crisis.jpg” by Shannon Nobles is licensed under CC BY-SA 4.0 ↵
- Zeran, V. (2016). Cultural competency and safety in nursing education: A case study. Northern Review, 43, 105–115. https://thenorthernreview.ca/index.php/nr/article/view/591 ↵
- Colorado Nurses Foundation and Colorado Nurses Association. (2020). Owning our biases: How nursing can change the healthcare landscape. Colorado Nurse, 120(3). https://assets.nursingald.com/uploads/publication/pdf/2103/Colorado_Nurse_8_20.pdf ↵
Patient Scenario
Mrs. Jones is a 38-year-old woman who presents to the pediatrician office with her three-year-old daughter, Aubrey. Mrs. Jones explains that her daughter has been experiencing infrequent bowel movements. She states, "Aubrey only passes stool 1 to 2 times per week. She strains to pass the stool and it is dry and hard when it passes." Aubrey nods and says, “My tummy hurts a lot when that happens.”
Applying the Nursing Process
Assessment: The nurse notes the mother's report of Aubrey experiencing increased difficulty passing stool, infrequent bowel movements, and only passing stool one to two times per week with hard, dry feces. She records Aubrey's complaint that her “tummy hurts a lot when that happens.” The nurse assesses Aubrey's abdomen and finds it rounded and firm with decreased bowel sounds present in all four quadrants.
Based on the assessment information that has been gathered, the nurse creates the following nursing care plan for Aubrey:
Nursing Diagnosis: Constipation related to insufficient fluid and fiber intake as manifested by decreased stool frequency, hypoactive bowel sounds, straining with defecation, hard dry stools, and patient reports “my tummy hurts a lot when that happens.”
Overall Goal: The patient will have soft bowel movements without difficulty.
SMART Expected Outcome: The patient will have a soft, formed stool every 24-48 hours.
Planning and Implementing Nursing Interventions:
The nurse will provide education to the patient and her mother regarding the importance of adequate fluid sources and fiber intake in addition to medications prescribed by the provider. The nurse will encourage water for hydration and provide education regarding beverage sources that may contribute to constipation. The nurse will describe the value of fresh fruits, vegetables, and whole grains in diet and describe strategies for encouraging toddler consumption of these foods. The nurse will encourage scheduling regular times to attempt elimination. The nurse will provide positive reinforcement to the child regarding using of the toilet regularly for bowel elimination and encourage the mother to track bowel movements and intake using an elimination diary.
Sample Documentation:
Mother presents with the patient to the clinic reporting infrequent bowel movements. She states, "Aubrey only passes stool 1 to 2 times per week. She strains to pass the stool and it is dry and hard when it passes." The patient reports, “My tummy hurts a lot when that happens.” The patient’s abdomen is firm and round with decreased bowel sounds present in all four quadrants. Patient education was provided to improve bowel elimination.
Evaluation:
The nurse calls Aubrey's mother in two days. The mother reports that Aubrey had a soft, formed bowel movement on each of the past two days. The SMART outcome was initially "met." The nurse encourages the mother to continue the planned interventions and to follow-up with the provider at the next clinic visit.
Patient Scenario
Mrs. Jones is a 38-year-old woman who presents to the pediatrician office with her three-year-old daughter, Aubrey. Mrs. Jones explains that her daughter has been experiencing infrequent bowel movements. She states, "Aubrey only passes stool 1 to 2 times per week. She strains to pass the stool and it is dry and hard when it passes." Aubrey nods and says, “My tummy hurts a lot when that happens.”
Applying the Nursing Process
Assessment: The nurse notes the mother's report of Aubrey experiencing increased difficulty passing stool, infrequent bowel movements, and only passing stool one to two times per week with hard, dry feces. She records Aubrey's complaint that her “tummy hurts a lot when that happens.” The nurse assesses Aubrey's abdomen and finds it rounded and firm with decreased bowel sounds present in all four quadrants.
Based on the assessment information that has been gathered, the nurse creates the following nursing care plan for Aubrey:
Nursing Diagnosis: Constipation related to insufficient fluid and fiber intake as manifested by decreased stool frequency, hypoactive bowel sounds, straining with defecation, hard dry stools, and patient reports “my tummy hurts a lot when that happens.”
Overall Goal: The patient will have soft bowel movements without difficulty.
SMART Expected Outcome: The patient will have a soft, formed stool every 24-48 hours.
Planning and Implementing Nursing Interventions:
The nurse will provide education to the patient and her mother regarding the importance of adequate fluid sources and fiber intake in addition to medications prescribed by the provider. The nurse will encourage water for hydration and provide education regarding beverage sources that may contribute to constipation. The nurse will describe the value of fresh fruits, vegetables, and whole grains in diet and describe strategies for encouraging toddler consumption of these foods. The nurse will encourage scheduling regular times to attempt elimination. The nurse will provide positive reinforcement to the child regarding using of the toilet regularly for bowel elimination and encourage the mother to track bowel movements and intake using an elimination diary.
Sample Documentation:
Mother presents with the patient to the clinic reporting infrequent bowel movements. She states, "Aubrey only passes stool 1 to 2 times per week. She strains to pass the stool and it is dry and hard when it passes." The patient reports, “My tummy hurts a lot when that happens.” The patient’s abdomen is firm and round with decreased bowel sounds present in all four quadrants. Patient education was provided to improve bowel elimination.
Evaluation:
The nurse calls Aubrey's mother in two days. The mother reports that Aubrey had a soft, formed bowel movement on each of the past two days. The SMART outcome was initially "met." The nurse encourages the mother to continue the planned interventions and to follow-up with the provider at the next clinic visit.

