Communication
2.5 Documentation
Using Technology to Access Information
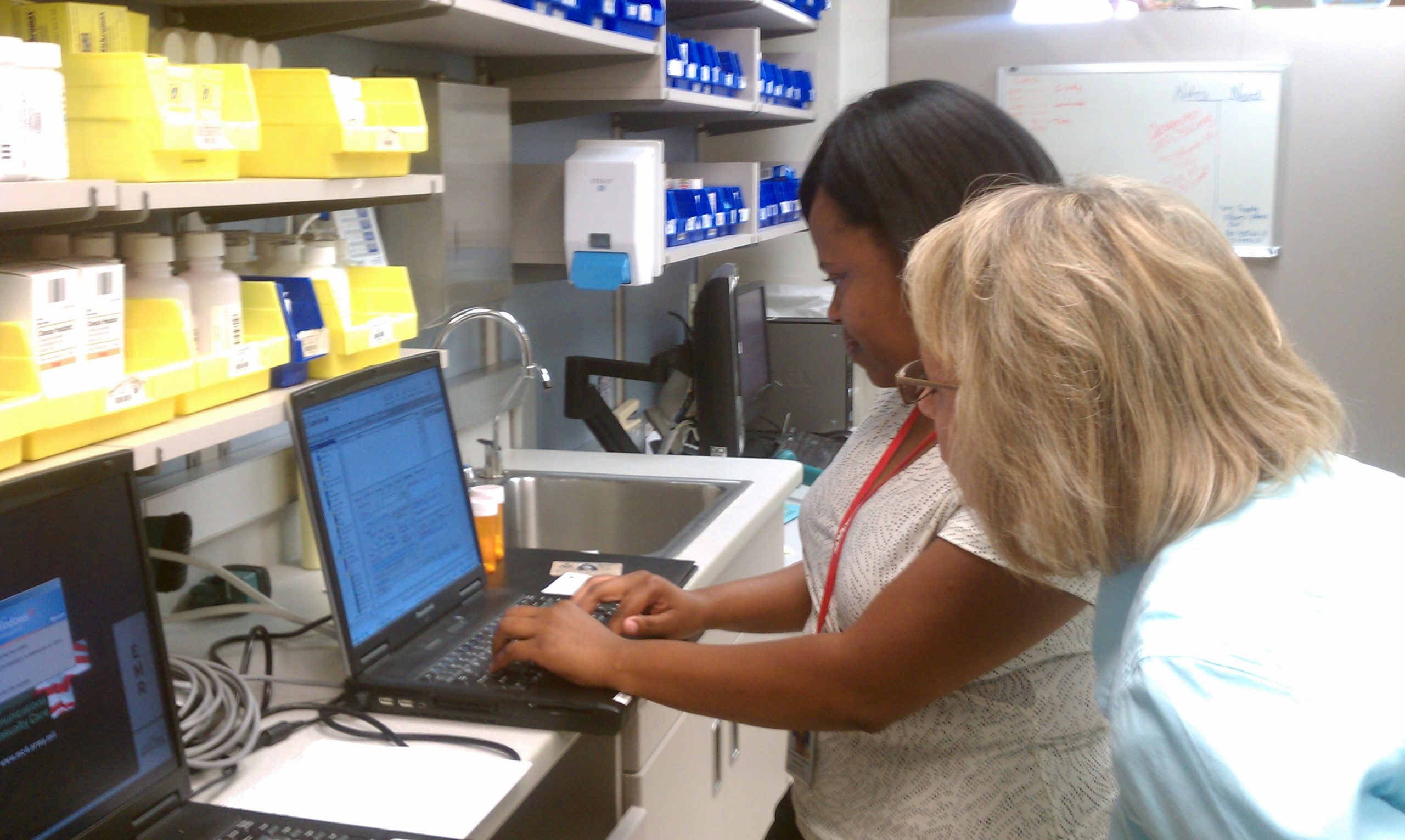
Most patient information in acute care, long-term care, and other clinical settings is now electronic and uses intranet technology for secure access by providers, nurses, and other health care team members to maintain patient confidentiality. Intranet refers to a private computer network within an institution. An electronic health record (EHR) is a real-time, patient-centered record that makes information available instantly and securely to authorized users.[1] Computers used to access an EHR can be found in patient rooms, on wheeled carts, in workstations, or even on handheld devices. See Figure 2.11[2] for an image of a nurse documenting in an EHR.
The EHR for each patient contains a great deal of information. The most frequent pieces of information that nurses access include the following:
- History and Physical (H&P): A history and physical (H&P) is a specific type of documentation created by the health care provider when the patient is admitted to the facility. An H&P includes important information about the patient’s current status, medical history, and the treatment plan in a concise format that is helpful for the nurse to review. Information typically includes the reason for admission, health history, surgical history, allergies, current medications, physical examination findings, medical diagnoses, and the treatment plan.
- Provider orders: This section includes the prescriptions, or medical orders, that the nurse must legally implement or appropriately communicate according to agency policy if not implemented.
- Medication Administration Records (MARs): Medications are charted through electronic medication administration records (MARs). These records interface the medication orders from providers with pharmacists and are also the location where nurses document medications administered.
- Treatment Administration Records (TARs): In many facilities, treatments are documented on a treatment administration record.
- Laboratory results: This section includes results from blood work and other tests performed in the lab.
- Diagnostic test results: This section includes results from diagnostic tests ordered by the provider such as X-rays, ultrasounds, etc.
- Progress notes: This section contains notes created by nurses and other health care providers regarding patient care. It is helpful for the nurse to review daily progress notes by all team members to ensure continuity of care.
View a video of how to read a patient’s chart.[3]
Legal Documentation
Nurses and health care team members are legally required to document care provided to patients. In a court of law, the rule of thumb used is, “If it wasn’t documented, it wasn’t done.” Documentation should be objective, factual, professional, and use proper medical terminology, grammar, and spelling. All types of documentation must include the date, time, and signature of the person documenting. Any type of documentation in the EHR is considered a legal document and must be completed in an accurate and timely manner. Abbreviations should be avoided in legal documentation.
Documentation is used for many purposes. It is used to ensure continuity of care across health care team members and across shifts; monitor standards of care for quality assurance activities; and provide information for reimbursement purposes by insurance companies, Medicare, and Medicaid. Documentation may also be used for research purposes or, in some instances, for legal concerns in a court of law.
Documentation by nurses includes recording patient assessments, writing progress notes, and creating or addressing information included in nursing care plans. Nursing care plans are further discussed in the “Planning” section of the “Nursing Process” chapter.
Common Types of Documentation
Common formats used to document patient care include charting by exception, focused DAR notes, narrative notes, SOAPIE progress notes, patient discharge summaries, and Minimum Data Set (MDS) charting.
Charting by Exception
Charting by exception (CBE) documentation was designed to decrease the amount of time required to document care. CBE contains a list of normal findings. After performing an assessment, nurses confirm normal findings on the list found on assessment and write only brief progress notes for abnormal findings or to document communication with other team members.
Focused DAR Notes
Focused DAR notes are a type of progress note that are commonly used in combination with charting by exception documentation. DAR stands for Data, Action, and Response. Focused DAR notes are brief. Each note is focused on one patient problem for efficiency in documenting and reading.
- Data: This section contains information collected during the patient assessment, including vital signs and physical examination findings found during the “Assessment” phase of the nursing process. The Assessment phase is further discussed in the “Nursing Process” chapter.
- Action: This section contains the nursing actions that are planned and implemented for the patient’s focused problem. This section correlates to the “Planning” and “Implementation” phases of the nursing process and are further discussed in the “Nursing Process” chapter.
- Response: This section contains information about the patient’s response to the nursing actions and evaluates if the planned care was effective. This section correlates to the “Evaluation” phase of the nursing process that is further discussed in the “Nursing Process” chapter.
View sample charting by exception paper documentation with associated DAR notes for abnormal findings.
For more information about writing DAR notes, visit What is F-DAR Charting?
View a video explaining F-DAR charting.[4]
Narrative Notes
Narrative notes are a type of progress note that chronicles assessment findings and nursing activities for the patient that occurred throughout the entire shift or visit. View sample narrative note documentation according to body system in each assessment chapter of the Open RN Nursing Skills textbook.
SOAPIE Notes
SOAPIE is a mnemonic for a type of progress note that is organized by six categories: Subjective, Objective, Assessment, Plan, Interventions, and Evaluation. SOAPIE progress notes are written by nurses, as well as other members of the health care team.
- Subjective: This section includes what the patient said, such as, “I have a headache.” It can also contain information related to pertinent medical history and why the patient is in need of care.
- Objective: This section contains the observable and measurable data collected during a patient assessment, such as the vital signs, physical examination findings, and lab/diagnostic test results.
- Assessment: This section contains the interpretation of what was noted in the Subjective and Objective sections, such as a nursing diagnosis in a nursing progress note or the medical diagnosis in a progress note written by a health care provider.
- Plan: This section outlines the plan of care based on the Assessment section, including goals and planned interventions.
- Interventions: This section describes the actions implemented.
- Evaluation: This section describes the patient response to interventions and if the planned outcomes were met.
Patient Discharge Summary
When a patient is discharged from an agency, a discharge summary is documented in the patient record, along with clear verbal and written patient education and instructions provided to the patient. Discharge summary information is frequently provided in a checklist format to ensure accuracy and includes the following:
- Time of departure and method of transportation out of the hospital (e.g., wheelchair)
- Name and relationship of person accompanying the patient at discharge
- Condition of the patient at discharge
- Patient education completed and associated educational materials or other information provided to the patient
- Discharge instructions on medications, treatments, diet, and activity
- Follow-up appointments or referrals given
See Figure 2.12[5] for an image of a nurse providing discharge instructions to a patient. Discharge teaching typically starts at admission and continues throughout the patient’s stay.

Minimum Data Set (MDS) Charting
In long-term care settings, additional documentation is used to provide information for reimbursement by private insurance, Medicare, and Medicaid. The Resident Assessment Instrument Minimum Data Set (MDS) is a federally mandated assessment tool created by registered nurses in skilled nursing facilities to track a patient’s goal achievement, as well as to coordinate the efforts of the health care team to optimize the resident’s quality of care and quality of life.[6] This tool also guides nursing care plan development.
- HealthIT.gov. (2019, September 10). What is an electronic health record (EHR)? https://www.healthit.gov/faq/what-electronic-health-record-ehr ↵
- "Winn_Army_Community_Hospital_Pharmacy_Stays_Online_During_Power_Outage.jpg" by Flickr user MC4 Army is licensed under CC BY 2.0 ↵
- RegisteredNurseRN. (2015, October 16). Charting for nurses | How to understand a patient's chart as a nursing student or new nurse. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/lNwRvKaNsGc ↵
- RegisteredNurseRN. (2015, October 27). FDAR for nurses | How to chart in F-DAR format with examples. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/BXf7wj9Wmfc ↵
- "1934626790-huge.jpg" by TommyStockProject is used under license from Shutterstock.com ↵
- Centers for Medicare & Medicaid Services. (2019, October). Long-term care facility resident assessment instrument 3.0 user’s manual. https://downloads.cms.gov/files/mds-3.0-rai-manual-v1.17.1_october_2019.pdf ↵
Pain management requires collaboration with the interdisciplinary team, including nurses, health care providers, pharmacists, and sometimes pain specialists. There are many different types of pain medications (called analgesics) that can be administered by various routes. Analgesics are classified as nonopioids, opioids, or adjuvants. An adjuvant is a medication that has been found in clinical practice to have either an independent analgesic effect or additive analgesic properties when administered with opioids. Examples of adjuvant medications include antidepressants (e.g., amitriptyline) and anti-seizure medications (e.g., gabapentin).
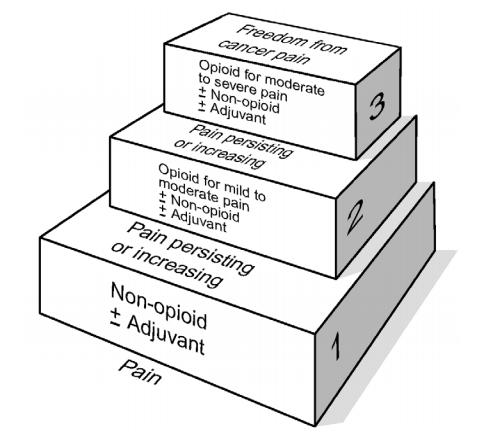
A general rule of thumb when administering analgesics is to use the lowest dose of medication, with fewest potential side effects and the least invasive route of administration, to effectively treat the level of pain as reported by the patient. The WHO ladder was originally developed by the World Health Organization for selecting analgesics for patients with cancer pain, but it can be broadened to illustrate this rule of thumb for managing pain appropriately for all patients. See Figure 11.6[1] for an image of the WHO ladder.
For example, if a patient reports a pain level of “2,” then a nurse typically starts at the lowest rung of the WHO ladder and administers a prescribed nonopioid via the oral route. If the nonopioid is not effective, then a prescribed adjuvant medication may be administered, or the nurse may decide to step up a rung on the ladder and administer a prescribed oral opioid for mild to moderate pain. On the other hand, if a patient reports severe pain, the nurse may start at the top rung of the ladder and administer a prescribed opioid for moderate to severe pain via the intravenous route for rapid relief.
Nonopioid Analgesics
Nonopioid analgesics include acetaminophen and NSAIDs.
Acetaminophen
Acetaminophen (Tylenol) is used to treat mild pain and fever but does not have anti-inflammatory properties. Acetaminophen is safe for all ages and can be administered using various routes, such as orally, rectally, and intravenously. Many over-the-counter (OTC) medications contain acetaminophen, along with other medications. See Figure 11.7[2] for an image of acetaminophen (Tylenol) and acetaminophen and diphenhydramine (Tylenol PM).
A potential severe side effect of acetaminophen is hepatotoxicity (severe liver damage). Severe liver damage may occur if an adult patient takes more than 4,000 mg of acetaminophen in 24 hours (or 3,200 mg for older adults or 2,000 mg for chronic alcoholics) or consumes three or more alcoholic drinks every day while using acetaminophen.
Because some medications are combined with acetaminophen or are prescribed “as needed,” the nurse must calculate the cumulative dose of acetaminophen over the previous 24-hour period before administering an additional dose. For example, Percocet 5/325 contains a combination of oxycodone 5 mg and acetaminophen 325 mg and may be prescribed as “1-2 tablets every 4-6 hours as needed for pain.” If two tablets are truly administered every four hours over a 24-hour period, this would add up to 3,900 mg of acetaminophen, exceeding the recommended guidelines for a geriatric patient, with the potential for causing liver damage.

NSAIDs
Nonsteroidal anti-inflammatories (NSAIDs) provide mild to moderate pain relief and also reduce fever and inflammation by inhibiting the production of prostaglandins. They can also be used as an adjuvant with opioids for severe pain. Examples of NSAIDs include ibuprofen, naproxen, and ketorolac. All NSAIDs, except aspirin, increase the risk of heart attack, heart failure, and stroke, with the risk being higher if the patient takes more than is directed or takes it for longer than directed. Common side effects include dyspepsia, nausea, and vomiting, so it is helpful to administer this medication with food. Older adults and those taking NSAIDs concurrently with other drugs, such as warfarin or corticosteroids, are at elevated risk for gastrointestinal bleeding. Renal failure can also occur with NSAIDs.
- Ibuprofen (Motrin) is safe for infants 6 months or older. It is typically prescribed every 6 to 8 hours.
- Naproxen (Naprosyn) is longer-acting than ibuprofen and is typically prescribed 2 or 3 times a day with a full glass of water.
- Ketorolac (Toradol) is commonly used to treat “breakthrough” pain that occurs during the treatment of severe acute pain already being treated with opioids. It is indicated for the short-term management (up to 5 days in adults) of moderate to severe acute pain that requires analgesia at the opioid level. Ketorolac is safe for adults, but the dosage should be reduced for patients ages 65 and over.
View a supplementary video on "How Do Pain Relievers Work?"
Opioid Analgesics
Opioids are used to treat moderate to severe pain and work by blocking the release of neurotransmitters involved in the processing of pain. Different opioids have different amounts of analgesia, ranging from codeine used to treat mild to moderate pain, up to morphine, used to treat severe pain and considered to be at the top of the WHO ladder. See Table 11.4a for a summary of common opioids. As always, check a drug reference for current dosage ranges before administering medications.
Table 11.4a Common Opioid Analgesics
| Generic Name | Trade Name(s) | Route | Adult Dosages |
|---|---|---|---|
| Codeine with acetaminophen | Tylenol #3 | PO | 30 mg/300 mg |
| Hydrocodone with acetaminophen | Lortab, Norco, Vicodin | PO
|
5 mg/300 mg or 325 mg
10 mg/320 mg or 325 mg 5mg/500 mg |
| Oxycodone (immediate release and extended release)
OR Oxycodone with acetaminophen |
Oxycodone IR & OxyContin (ER)
Percocet & Roxicet |
PO
PO |
5 mg - 10 mg
5 mg/325 mg |
| Fentanyl | Duragesic, Sublimaze | Transdermal
IM IV |
12 mcg - 100 mcg/hr
0.5 - 1 mcg/kg 0.5 - 1 mcg/kg |
| Hydromorphone | Dilaudid | PO
Rectal SubQ, IM, & IV |
4 - 8 mg
3 mg 1.5 mg (may be increased) |
| Morphine | Duramorph, MS Contin, Oramorph SR, & Roxanol | PO & Rectal
SubQ, IM, & IV |
30 mg (may be increased)
4 - 10 mg (may be increased) |
Morphine is also commonly used to treat cancer pain and end-of-life pain because there is no “ceiling effect,” meaning the higher the dose, the higher the level of analgesia. Morphine is administered via various routes of administration, including orally, rectally, subcutaneously, intramuscularly, and intravenously. See Figure 11.8[3] for an image of a vial of morphine for injection or intravenous use.

Other types of opioids can be administered through the skin, such as the fentanyl transdermal patch. See Figure 11.9[4] for an image of a fentanyl transdermal patch.

Alternative Routes of Administration of Opioids
Analgesic medications can be administered via several routes, including orally, rectally, subcutaneously, and intravenously. Intramuscular routes are typically avoided. Other routes of administration include patient-controlled analgesia (PCA), intrathecally, and by epidural.
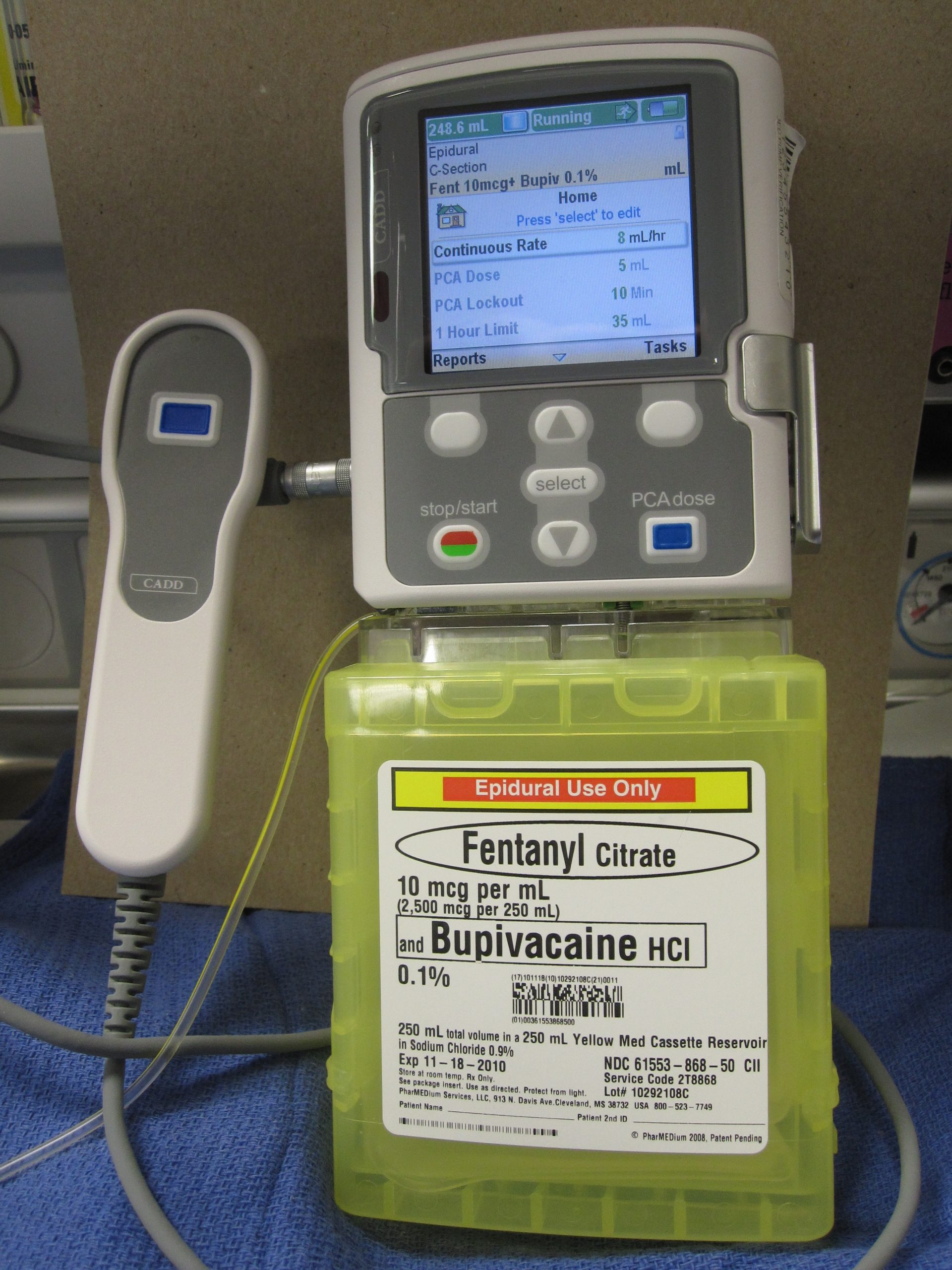
Patient Controlled Analgesia
Patient-controlled analgesia (PCA) is a method of pain management that allows hospitalized patients with severe pain to safely self-administer opioid medications using a programmed pump according to their level of discomfort. See Figure 11.10[5] for an image of a PCA pump. A computerized pump contains a syringe of pain medication and is connected directly to a patient's intravenous (IV) line. Pain medication includes morphine, hydromorphone, and fentanyl. Doses of medication can be self-administered as needed by the patient by pressing a button. However, the pump is programmed to only allow administration of medication every set number of minutes with a maximum dose of medication every hour. These pump settings, and the design of the system requiring the patient to be alert enough to press the button, are safety measures to prevent overmedication that can cause sedation and respiratory depression. For this reason, no one but the patient should press the button for administration of medication (not even the nurse.)
In other cases, the PCA pump delivers a small, continuous flow of pain medication intravenously with the option of the patient self-delivering additional medication as needed, according to the limits set on the pump.
To document the amount and frequency of pain medication the patient is receiving, as well as to prevent drug diversion, the settings on the pump are checked at the end of every shift as part of the bedside report. The incoming and outgoing nurses double-check and document the pump settings, the amount of medication administered during the previous shift, and the amount of medication left in the syringe.
Intrathecal Pump
Another type of pump used to deliver pain medication is the intrathecal pump. This pump is surgically implanted under the skin and delivers small quantities of pain medication, such as morphine, directly into the spinal fluid. It is used to treat pain and muscle spasticity when other methods have not effectively treated the pain. It is typically used for patients with severe chronic pain, such as cancer pain, back pain, or nerve pain. However, the FDA urges cautious use because it has received numerous Medical Device Reports (MDRs) describing adverse events with implanted pumps. These reports describe pump failures, dosing errors, and other potential safety issues. Patient symptoms described in these reports include pain, opioid withdrawal, fever, vomiting, muscle spasm, cognitive changes, weakness, and cardiac and respiratory distress.[6]
Epidural
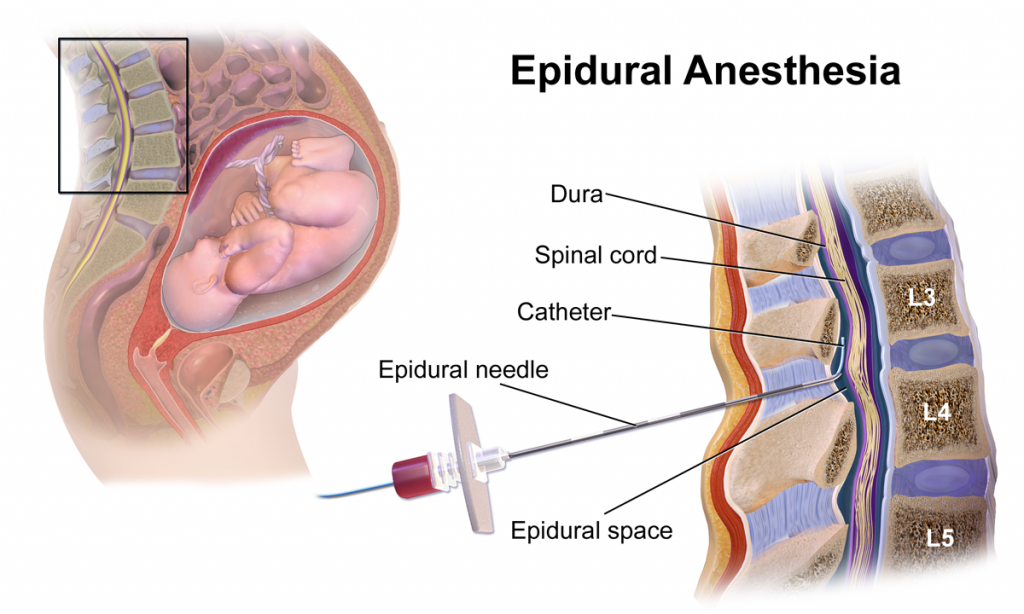
A third route of alternative administration of pain medication is epidural anesthesia. See Figure 11.11[7] for an image of an epidural anesthesia. Morphine is administered into the spinal fluid via an epidural catheter for severe pain management associated with surgical procedures or during labor and delivery. It is also used to treat chronic pain that has not responded to other treatments. Epidural administration of 5 mg of morphine provides adequate postoperative analgesia for up to 24 hours.[8]
Adverse Effects of Opioids
Respiratory Depression
The most serious potential adverse effect of opioids is respiratory depression. Respiratory depression is usually preceded by sedation. The nurse must carefully monitor patients receiving opioids for oversedation, which results in decreased respiratory rate. Patients at greatest risk are those who have never received an opioid and are receiving their first dose, those receiving an increased dose of opioids, or those taking benzodiazepines or other sedatives concurrently with opioids. If a patient develops opioid-induced respiratory depression, the opioid is reversed with naloxone (Narcan) that immediately reverses all analgesic effect.[9] See Figure 11.12[10] for an image of a naloxone rescue kit to treat respiratory depression caused by opioids.

Opioids can cause several other common adverse effects, such as constipation, nausea and vomiting, urinary retention, and pruritus (itching).
Constipation
Opioids slow peristalsis and cause increased reabsorption of fluid into the large intestine, resulting in slow-moving, hard stools. Nurses play an important role in preventing constipation for all patients taking opioids. A bowel management program should be initiated with the first dose and continued until the opioid is discontinued. A stool softener (such as docusate) is typically prescribed initially as part of the bowel management program. If needed, a stimulant laxative, such as sennoside (Senna), bisacodyl, or Milk of Magnesia may be added to maintain a normal bowel pattern. However, stimulants should not be taken long-term because they can be addictive. Patients taking opioids should be encouraged to increase fluid and fiber intake and ambulate, as appropriate.[11]
Nausea and Vomiting
Nausea and vomiting can occur with opioid administration due to several factors, such as the slowing of gastrointestinal mobility, constipation, or stimulation of the vestibular system. Tolerance will develop to these adverse effects within a few days. Treatment includes antiemetics, such as compazine or ondansetron.[12]
Urinary Retention
Urinary retention is common in opioid-naive patients or when opioids are delivered via the spinal route. Urinary catheterization may be required if the patient is unable to void. Tolerance to this effect occurs within a few days.[13]
Pruritus
Pruritus (itching) may occur, especially when opioids are administered via the spinal route. Antihistamines, such as diphenhydramine (Benadryl), may be used to treat pruritus, but the patient should be monitored for potential sedative effects of this medication.[14]
Adjuvant Medications
Adjuvants are medications that are not classified as analgesics but have been found to contribute to analgesic effects, especially when used in addition to opioids. Two common examples of adjuvant medications are amitriptyline and gabapentin.
Amitriptyline
Amitriptyline is a tricyclic antidepressant that is also believed to be effective in treating neuropathic pain, such as diabetic neuropathy, postherpetic neuralgia, or post‐stroke pain. The mechanism of action of amitriptyline in the treatment of neuropathic pain remains uncertain, although it is known to inhibit both serotonin and noradrenaline reuptake. It is usually administered at bedtime in an attempt to reduce any sedative effects during the day.[15]
Gabapentin
Gabapentin is an anticonvulsant that is also effective in treating neuropathic pain and restless leg syndrome. Patients taking gabapentin should be warned that their mental health may change in unexpected ways or they may become suicidal. Nurses should implement fall precautions for patients taking gabapentin because it can cause sleepiness, weakness, and unsteadiness.[16]
Nonpharmacological Interventions
Nonpharmacological interventions can be used with or without pharmacologic interventions and often provide tremendous benefits to the patient. A variety of techniques can be selected by the patient that best fit their needs and goals. Nonpharmacological interventions should be documented in the plan of care and their effectiveness evaluated in terms of their ability to meet the patient’s goals for pain relief. Table 11.4b provides examples of several types of nonpharmacological interventions.
Table 11.4b Nonpharmacological Interventions
| Intervention | Examples |
|---|---|
| Distraction | Describing photos, telling jokes, and playing games |
| Relaxation | Rhythmic breathing, meditation, prayer, imagery, and music therapy |
| Basic comfort measures | Proper positioning and therapeutic environment
Avoiding sudden movement Reducing pain stimuli within the environment |
| Cutaneous stimulation | Acupuncture and acupressure
Massage: 3-5 minutes offers benefits Transcutaneous Electrical Nerve Stimulation (TENS) unit: a specialized stimulator placed over the area of pain |
| Application of heat or cold | Heat: vasodilation increases blood flow; duration should be 5-20 minutes based on patient tolerance
Cold: vasoconstriction reduces blood flow; cold numbs nerve sensations; duration should be no longer than 20 minutes Cool baths and moist, cool compresses |
| Mind-body therapies | Biofeedback
Meditation and mindfulness |
| Aromatherapy | Lotions and moisturizing cream
Avoiding strong smells |
| Exercise | Physical activity
Tai chi Yoga |
| Therapy | Physical therapy
Occupational therapy |
See Figure 11.13[17] for images of various nonpharmacological interventions.

Patients may also consider using complementary health approaches to manage chronic pain. Complementary approaches include acupuncture, massage therapy, meditation, relaxation techniques, spinal manipulation, Tai Chi, yoga, and dietary supplements. Read more about complementary approaches using the hyperlink provided in the following box.
Read more about complementary approaches to treat pain from the National Center for Complementary and Integrative Health.
Read about pain management for older adults from the University of Iowa.

