Communication
2.2 Basic Communication Concepts
Effective communication is one of the Standards of Professional Performance established by the American Nurses Association. The standard states, “The registered nurse communicates effectively in all areas of practice.”[1] There are several concepts related to effective communication such as demonstrating appropriate verbal and nonverbal communication, using assertive communication, being aware of personal space, and overcoming common barriers to effective communication.
Types of Communication
Verbal Communication
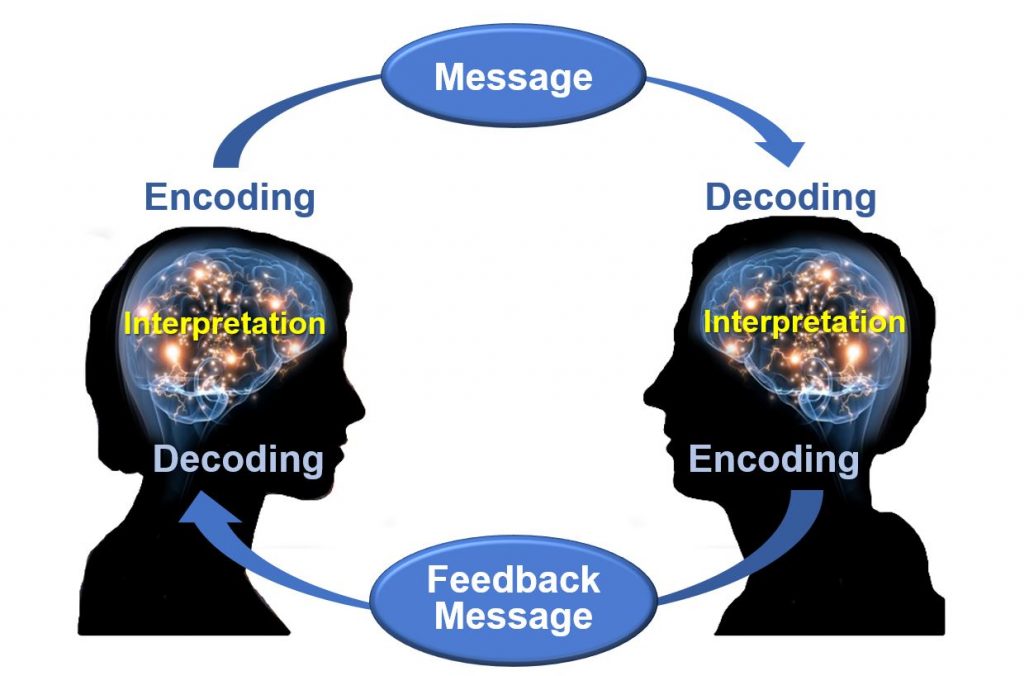
Effective communication requires each interaction to include a sender of the message, a clear and concise message, and a receiver who can decode and interpret that message. The receiver also provides a feedback message back to the sender in response to the received message. See Figure 2.1[2] for an image of effective communication between a sender and receiver.
Nurses assist patients and their family members to understand health care needs and treatments by using verbal, nonverbal, and written communication. Verbal communication is more than just talking. Effective verbal communication is defined as an exchange of information using words understood by the receiver in a way that conveys professional caring and respect.[3] Nurses who speak using extensive medical jargon or slang may create an unintended barrier to their own verbal communication processes. When communicating with others, it is important for the nurse to assess the receiver’s preferred method of communication and individual receiver characteristics that might influence communication, and subsequently adapt communication to meet the receiver’s needs. For example, the nurse may adapt postsurgical verbal instruction for a pediatric versus an adult patient. Although the information requirements regarding signs of infection, pain management, etc., might be similar, the way in which information is provided may be quite different based on developmental level. Regardless of the individual adaptations that are made, the nurse must be sure to always verify patient understanding.
Nonverbal Communication
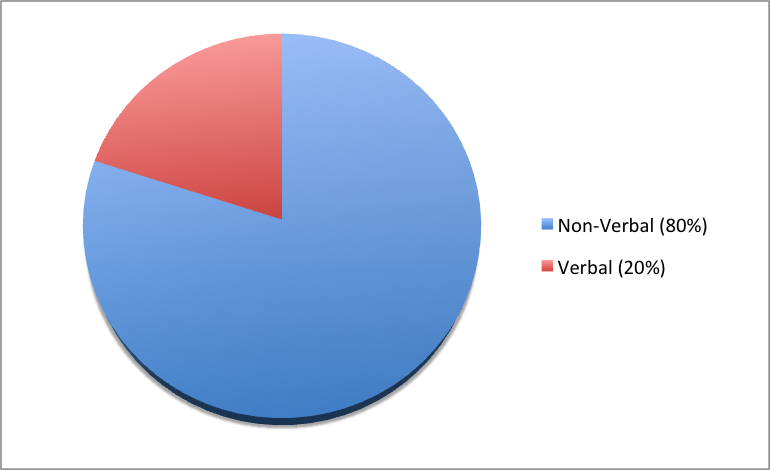
In addition to communicating verbally, the nurse must also be aware of messages sent by nonverbal communication. Nonverbal communication can have a tremendous impact on the communication experience and may be much more powerful than the verbal message itself. You may have previously learned that 80% of communication is nonverbal communication (see Figure 2.2[4]). The importance of nonverbal communication during communication has also been described in percentages of 55, 38, and 7, meaning 55% of communication is body language, 38% is tone of voice, and 7% is the actual words spoken.[5]
Nonverbal communication includes body language and facial expressions, tone of voice, and pace of the conversation. For example, compare the nonverbal communication messages in Figures 2.3[6] and 2.4.[7] What nonverbal cues do you notice about both toddlers?


Nurses should be attentive to their nonverbal communication cues and the messages they provide to patients and their families. Nurses should be purposeful in their use of nonverbal communication that conveys a feeling of caring.[8] What nonverbal cues do you notice about the nurse in Figure 2.5[9] that provide a perception of professional caring?

Nurses use nonverbal communication such as directly facing patients at eye level, leaning slightly forward, and making eye contact to communicate they care about what the person is telling them and they have their full attention.[10]
![]()
It is common for health care team members in an acute care setting to enter a patient’s room and begin interacting with a patient who is seated or lying in bed. However, it is important to remember that initial or sensitive communication exchanges are best received by the patient if the nurse and patient are at eye level. Bringing a chair to the patient’s bedside can help to facilitate engagement in the communication exchange. SOLER is common mnemonic used to facilitate nonverbal communication (sit with open posture and lean in with good eye contact in a relaxed manner).
Communication Styles
In addition to verbal and nonverbal communication, people communicate with others using three styles. A passive communicator puts the rights of others before their own. Passive communicators tend to be apologetic or sound tentative when they speak and often do not speak up if they feel as if they are being wronged. Aggressive communicators, on the other hand, come across as advocating for their own rights despite possibly violating the rights of others. They tend to communicate in a way that tells others their feelings don’t matter. However, assertive communicators respect the rights of others while also standing up for their own ideas and rights when communicating. An assertive person is direct, but not insulting or offensive.[11] Assertive communication refers to a way of conveying information that describes the facts and the sender’s feelings without disrespecting the receiver’s feelings. Using “I” messages such as, “I feel…,” “I understand…,” or “Help me to understand…” are strategies for assertive communication. This method of communicating is different from aggressive communication that uses “you” messages and can feel as if the sender is verbally attacking the receiver rather than dealing with the issue at hand. For example, instead of saying to a coworker, “Why is it always so messy in your patients’ rooms? I dread following you on the next shift!,” an assertive communicator would use “I” messages to say, “I feel frustrated spending the first part of my shift decluttering our patients’ rooms. Help me understand why it is a challenge to keep things organized during your shift?”
Using assertive communication is an effective way to solve problems with patients, coworkers, and health care team members.
View this humorous video demonstrating assertive communication techniques being used by the actors on a TV show:
Everybody Loves Raymond Uses Active Listening – from Parent Effectiveness Training.
Personal Space
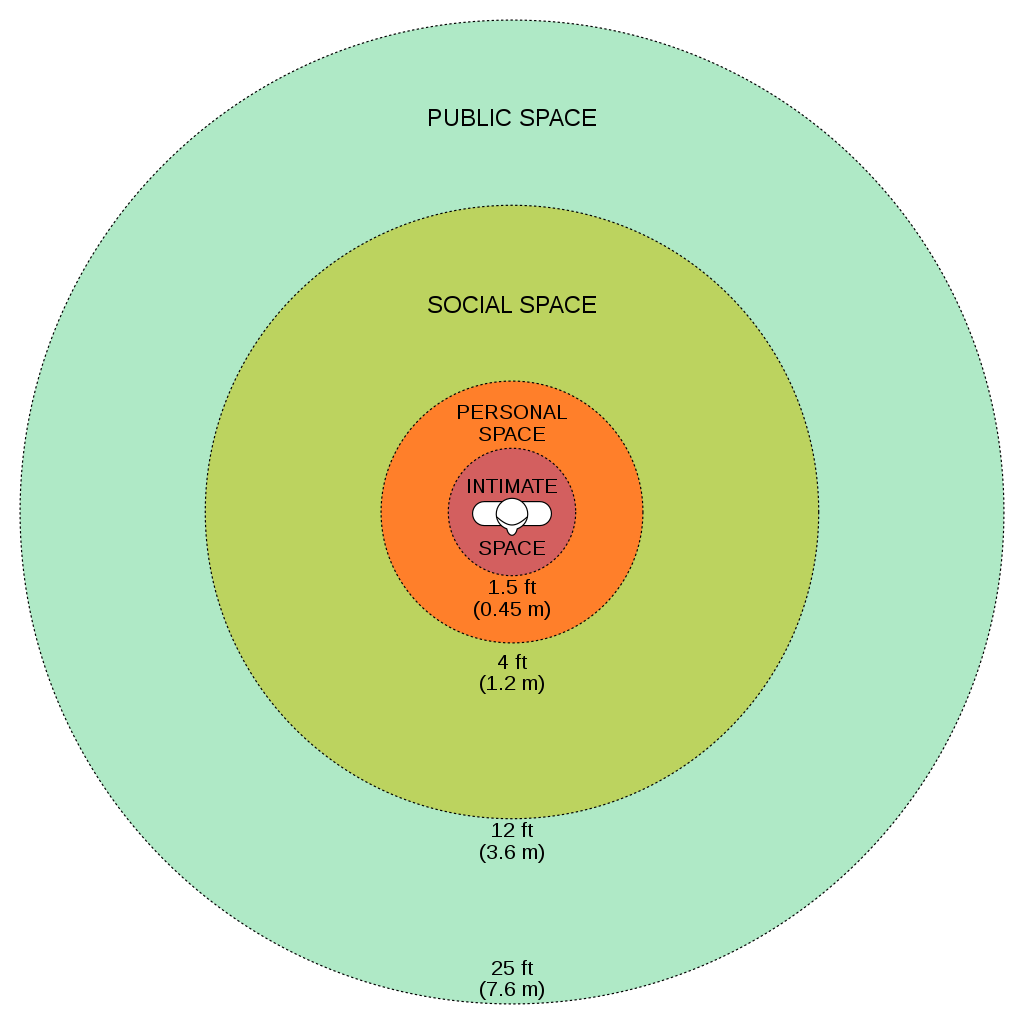
While being aware of verbal and nonverbal messages and communicating assertively, it is also important to be aware of others’ personal space. Proxemics is the study of personal space and provides guidelines for professional communication. The public zone is over 10 feet of distance between people and generally avoids physical contact. The social zone is four to 10 feet of distance between people. It is used during social interactions and business settings. The personal zone is 18 inches to four feet of space and is generally reserved for friends and family. Less than 18 inches is reserved for close relationships but may be invaded when in crowds or playing sports.[12] Nurses usually communicate within the social zone to maintain professional boundaries. However, when assessing patients and performing procedures, nurses often move into a patient’s personal zone. Nurses must be aware of patients’ feelings of psychological discomfort that can occur when invading this zone. Additionally, cultural considerations may impact the appropriateness of personal space when providing patient care. See Figure 2.6 for example of personal space zones.[13]
Overcoming Common Barriers to Communication
It is important for you to reflect on personal factors that influence your ability to communicate effectively. There are many factors that can cause the message you are trying to communicate to become distorted and not perceived by the receiver in the way you intended. It is important to seek feedback that your message is clearly understood. Nurses must be aware of these potential barriers and try to reduce their impact by continually seeking feedback and checking understanding.[14]
Common barriers to communication in health care and strategies to overcome them are described in the following box.[15]
Common Barriers to Communication in Health Care
- Jargon: Avoid using medical terminology, complicated, or unfamiliar words. When communicating with patients, explain information in plain language that is easy to understand by those without a medical or nursing background.
- Lack of attention: Nurses are typically very busy with several tasks to complete for multiple patients. It is easy to become focused on the tasks instead of the patient. When entering a patient’s room, it is helpful to pause, take a deep breath, and mindfully focus on the patient in front of you to give them your full attention. Patients should feel as if they are the center of your attention when you are with them, no matter how many other things you have going on.
- Noise and other distractions: Health care environments can be very noisy with people talking in the room or hallway, the TV blaring, alarms beeping, and pages occurring overhead. Create a calm, quiet environment when communicating with patients by closing doors to the hallway, reducing the volume of the TV, or moving to a quieter area, if possible.
- Light: A room that is too dark or too light can create communication barriers. Ensure the lighting is appropriate according to the patient’s preference.
- Hearing and speech problems: If your patient has hearing or speech problems, implement strategies to enhance communication. See the “Adapting Your Communication” section below for strategies to address hearing and speech problems.
- Language differences: If English is not your patient’s primary language, it is important to seek a medical interpreter and to also provide written handouts in the patient’s preferred language when possible. Most agencies have access to an interpreter service available by phone if they are not available on-site.
- Differences in cultural beliefs: The norms of social interaction vary greatly in different cultures, as well as the ways that emotions are expressed. For example, the concept of personal space varies among cultures, and some patients are stoic about pain whereas others are more verbally expressive. Read more about caring for diverse patients in the “Diversity” chapter.
- Psychological barriers: Psychological states of the sender and the receiver affect how the message is sent, received, and perceived. For example, if nurses are feeling stressed and overwhelmed with required tasks, the nonverbal communication associated with their messages such as lack of eye contact, a hurried pace, or a short tone can affect how the patient perceives the message. If a patient is feeling stressed, they may not be able to “hear” the message or they may perceive it differently than it was intended. It is important to be aware of signs of the stress response in ourselves and our patients and implement appropriate strategies to manage the stress response. See the box below for more information about strategies to manage the stress response.
- Physiological barriers: It is important to be aware of patients’ potential physiological barriers when communicating. For example, if a patient is in pain, they are less likely to hear and remember what was said, so pain relief should be provided as needed before providing patient education. However, it is also important to remember that sedatives and certain types of pain medications often impair the patient’s ability to receive and perceive messages so health care documents cannot be signed by a patient after receiving these types of medications.
- Physical barriers for nonverbal communication: Providing information via e-mail or text is often less effective than face-to-face communication. The inability to view the nonverbal communication associated with a message such as tone of voice, facial expressions, and general body language often causes misinterpretation of the message by the receiver. When possible, it is best to deliver important information to others using face-to-face communication so that nonverbal communication is included with the message.
- Differences in perception and viewpoints: Everyone has their own beliefs and perspectives and wants to feel “heard.” When patients feel their beliefs or perspectives are not valued, they often become disengaged from the conversation or the plan of care. Nurses should provide health care information in a nonjudgmental manner, even if the patient’s perspectives, viewpoints, and beliefs are different from their own.
Managing the Stress Response[16]
The stress response is a common psychological barrier to effective communication. It can affect the message sent by the sender or how it is received by the receiver. The stress response is a common reaction to life events, such as a nurse feeling stressed by being overwhelmed with tasks to complete for multiple patients, or a patient feeling stressed when admitted to a hospital or receiving a new diagnosis. Symptoms of the stress response include irritability, sweaty palms, a racing heart, difficulty concentrating, and impaired sleep. It is important to recognize symptoms of the stress response in ourselves and our patients and use strategies to manage the stress response when communicating. Strategies to manage the stress response are as follows:
- Use relaxation breathing. Become aware of your breathing. Take a deep breath in your nose and blow it out through your mouth. Repeat this process at least three times in succession and then as often as needed throughout the day.
- Make healthy diet choices. Avoid caffeine, nicotine, and junk food because these items can increase feelings of anxiety or being on edge.
- Make time for exercise. Exercise stimulates the release of natural endorphins that reduce the body’s stress response and also helps to improve sleep.
- Get enough sleep. Set aside at least 30 minutes before going to bed to wind down from the busyness of the day. Avoid using electronic devices like cell phones before bedtime because the backlight can affect sleep.
- Use progressive relaxation. There are several types of relaxation techniques that focus on reducing muscle tension and using mental imagery to induce calmness. Progressive relaxation generally includes the following steps:
- Start by lying down somewhere comfortable and firm, like a rug or mat on the floor. Get yourself comfortable.
- Relax and try to let your mind go blank. Breathe slowly, deeply, and comfortably, while gradually and consciously relaxing all your muscles, one by one.
- Work around the body one main muscle area at a time, breathing deeply, calmly, and evenly. For each muscle group, clench the muscles tightly and hold for a few seconds, and then relax them completely. Repeat the process, noticing how it feels. Do this for each of your feet, calves, thighs, buttocks, stomach, arms, hands, shoulders, and face.
- American Nurses Association. (2015). Nursing: Scope and standards of practice (3rd ed.). American Nurses Association. ↵
- “Osgood-Schramm-model-of-communication.jpg“ by Jordan Smith at eCampus Ontario is licensed under CC BY 4.0. Access for free at https://ecampusontario.pressbooks.pub/communicationatwork/chapter/1-3-the-communication-process/ ↵
- This work is a derivative of Human Relations by LibreTexts and is licensed under CC BY-NC-SA 4.0 ↵
- “Constituents of Communication.png” by jb11ko, lb13an, ad14xz, jb12xu is licensed under CC BY-SA 4.0 ↵
- Thompson, J. (2011). Is nonverbal communication a numbers game? Psychology Today. https://www.psychologytoday.com/us/blog/beyond-words/201109/is-nonverbal-communication-numbers-game ↵
- “I’m angry” by WiLPrZ is licensed under CC BY-NC-ND 2.0 ↵
- “Happy Toddler” by Chris Bloom is licensed under CC BY-SA 2.0 ↵
- This work is a derivative of Human Relations by LibreTexts and is licensed under CC BY-NC-SA 4.0 ↵
- "PIXNIO-42752-4542x3003.jpg" by James Gathany, Judy Schmidt, USCDCP is in the Public Domain ↵
- Stickley, T. (2011). From SOLER to SURETY for effective non-verbal communication. Nurse Education in Practice, 11(6), 395-398. https://doi.org/10.1016/j.nepr.2011.03.021 ↵
- This work is a derivative of Human Relations by LibreTexts and is licensed under CC BY-NC-SA 4.0 ↵
- Psychology Today. (n.d.) Proxemics. https://www.psychologytoday.com/us/basics/proxemics ↵
- “Personal Space.svg” by WebHamster is licensed under CC BY-SA 3.0 ↵
- SkillsYouNeed. (n.d.). Barriers to effective communication. https://www.skillsyouneed.com/ips/barriers-communication.html ↵
- SkillsYouNeed. (n.d.). Barriers to effective communication. https://www.skillsyouneed.com/ips/barriers-communication.html ↵
- American Psychological Association. (2019). Healthy Ways to Handle Life's Stressors. https://www.apa.org/topics/stress/tips ↵
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
You are a nurse working in a long-term care facility. You have been assigned to care for Mr. Johns, a 74-year-old client recently diagnosed with a urinary tract infection, resulting in frequent incontinence. Mr. Johns suffered a CVA (stroke) six months ago and has difficulties ambulating and attending to his own needs because of weakness on his right side. Mr. Johns is alert and oriented to person, place, and time, but has decreased sensation on his entire right side. He spends most of his time in bed or sitting at his bedside in a wheelchair due to his difficulty with ambulation. He eats about 50% of his meals. While assessing Mr. Johns, you note that he is thin for his height, incontinent of foul-smelling urine, and has a deepened reddened area on his sacrum.
- What additional information, including lab work, would you like to gather to further assess Mr. Johns' potential for pressure injury development?
- What factors make him particularly vulnerable to the development of pressure injuries?
Angiogenesis: The process of wound healing when new capillaries begin to develop within the wound 24 hours after injury to bring in more oxygen and nutrients for healing.
Approximated edges: The well-closed edges of a wound healing by primary intention.
Arterial insufficiency: A condition caused by lack of adequately oxygenated blood supply to specific tissues.
Braden Scale: A standardized assessment tool used to assess and document a patient’s risk factors for developing pressure injuries.
Deep tissue pressure injuries: Persistent; non-blanchable; deep red, maroon, or purple discoloration of intact or nonintact skin revealing a dark wound bed or blood-filled blister. Pain and temperature change often precede skin color changes. Discoloration may appear differently in darkly pigmented skin.
Dehiscence: The separation of a surgical incision.
Dermis: The layer of skin underneath under the epidermis, containing hair follicles, sebaceous glands, blood vessels, endocrine sweat glands, and nerve endings.
Epidermis: The very thin, top layer of the skin that contains openings of the sweat gland ducts and the visible part of hair known as the hair shaft.
Epithelialization: The development of new epidermis and granulation tissue in a healing wound.
Eschar: Dark brown/black, dry, thick, and leathery dead tissue in wounds.
Excoriation: Redness and removal of the surface of the topmost layer of skin, often due to maceration or itching.
Friction: The rubbing of skin against a hard object, such as the bed or the arm of a wheelchair. This rubbing causes heat that can remove the top layer of skin and often results in skin damage.
Granulation tissue: New connective tissue in a healing wound with new, fragile, thin-walled capillaries.
Hemostasis phase of wound healing: The first stage of wound healing when clotting factors are released to form clots to stop the bleeding.
Hypodermis: The bottom layer of skin, also referred to as the subcutaneous layer, consisting mainly of adipose tissue or fat, along with some blood vessels and nerve endings. Beneath this layer lies muscles, tendons, ligaments, and bones.
Impaired skin integrity: Altered epidermis and/or dermis.
Impaired tissue integrity: Damage to deeper layers of the skin or other integumentary structures. The NANDA-I definition of impaired tissue integrity is, “Damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament.”
Inflammatory phase of wound healing: The second stage of healing when vasodilation occurs to move white blood cells into the wound to start cleaning the wound bed.
Maceration: A condition that occurs when skin has been exposed to moisture for too long causing it to appear soggy, wrinkled, or whiter than usual.
Maturation phase: The final stage of wound healing when collagen continues to be created to strengthen the wound and prevent it from reopening.
Necrosis: Tissue death.
Necrotic: Dead tissue that is black.
Nonblanchable erythema: Skin redness that does not turn white when pressed.
Osteomyelitis: Bone infection.
Pressure injuries: Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.
Primary intention: A type of wound that is sutured, stapled, glued, or otherwise closed so the wound heals beneath the closure.
Proliferative phase of wound healing: The third stage of wound healing that begins a few days after injury and includes four processes: epithelialization, angiogenesis, collagen formation, and contraction.
Purulent: Drainage that is thick; opaque; tan, yellow, green, or brown in color. New purulent drainage should always be reported to the health care provider.
Sanguineous: Drainage from a wound that is fresh bleeding.
Secondary intention: A type of healing that occurs when the edges of a wound cannot be brought together, so the wound fills in from the bottom up by the production of granulation tissue. An example of a wound healing by secondary intention is a pressure ulcer.
Serosanguinous: Serous drainage with small amounts of blood present.
Serous: Drainage from a wound that is clear, thin, watery plasma. It’s normal during the inflammatory stage of wound healing, and small amounts are considered normal wound drainage.
Shear: Damage that occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue.
Slough: Inflammatory exudate in wounds that is usually light yellow, soft, and moist.
Stage 1 pressure injuries: Intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred.
Stage 2 pressure injuries: Partial-thickness loss of skin with exposed dermis. The wound bed is viable and may appear like an intact or ruptured blister.
Stage 3 pressure injuries: Full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed. The depth of tissue damage varies by anatomical location. Undermining and tunneling may be present. If slough or eschar obscures the wound so that tissue loss cannot be assessed, the pressure injury is referred to as unstageable.
Stage 4 pressure injuries: Full-thickness tissue loss like Stage 3 pressure injuries but also have exposed cartilage, tendon, ligament, muscle, or bone.
Tertiary intention: The healing of a wound that has had to remain open or has been reopened, often due to severe infection.
Tunneling: Passageways underneath the surface of the skin that extend from a wound and can take twists and turns.
Undermining: A condition that occurs in wounds when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound's edge.
Unstageable pressure injuries: Full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar.
Venous insufficiency: A condition that occurs when the cardiovascular system cannot adequately return blood and fluid from the extremities to the heart.
Learning Objectives
- Assess patients for subjective and objective manifestations of alterations in comfort
- Identify factors related to comfort across the life span
- Adhere to standards of care for the patient experiencing pain
- Identify nonpharmacologic measures to minimize pain and discomfort
- Outline the plan for monitoring the patient response to the interventions for pain and discomfort
- Identify evidence-based practices related to assessing pain and providing comfort
Pain is a universal sensation that everyone experiences, and acute pain is a common reason why patients seek medical care. Nurses work with the interdisciplinary team to assess and manage pain in a multidimensional approach to provide comfort and prevent suffering. This chapter will review best practices and standards of care for the assessment and management of pain.
Learning Objectives
- Assess patients for subjective and objective manifestations of alterations in comfort
- Identify factors related to comfort across the life span
- Adhere to standards of care for the patient experiencing pain
- Identify nonpharmacologic measures to minimize pain and discomfort
- Outline the plan for monitoring the patient response to the interventions for pain and discomfort
- Identify evidence-based practices related to assessing pain and providing comfort
Pain is a universal sensation that everyone experiences, and acute pain is a common reason why patients seek medical care. Nurses work with the interdisciplinary team to assess and manage pain in a multidimensional approach to provide comfort and prevent suffering. This chapter will review best practices and standards of care for the assessment and management of pain.

