Integumentary
10.4 Pressure Injuries
The remainder of this chapter will focus on applying the nursing process to a specific type of wound called a pressure injury. Pressure injuries are defined as, “Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.” (Note that the 2016 NPUAP Pressure Injury Staging System now uses the term “pressure injury” instead of the historic term “pressure ulcer” because a pressure injury can occur without an ulcer present.) Pressure injuries commonly occur on the sacrum, heels, ischia, and coccyx and form when the skin layer of tissue gets caught between an external hard surface, such as a bed or chair, and the internal hard surface of a bone.
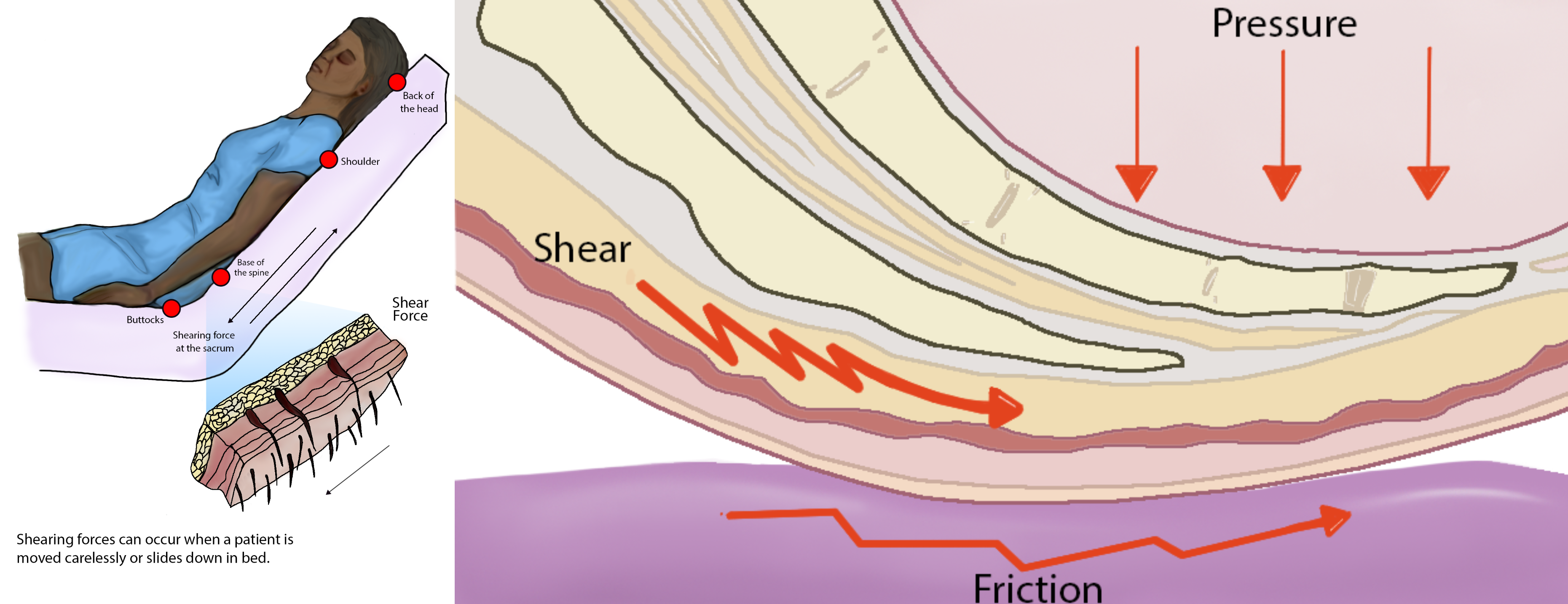
Shear occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue. For example, when a patient slides down in bed, the outer layer of skin remains immobile because it remains attached to the sheets due to friction. However, the deeper layer of tissue (attached to bone) moves as the patient slides down. This opposing movement of the outer layer of skin and the underlying tissues causes the capillaries to stretch and tear, which then causes decreased blood flow and oxygenation of the surrounding tissues resulting in a pressure injury.[1]
Friction refers to rubbing the skin against a hard object, such as the bed or the arm of a wheelchair. This rubbing causes heat, which can remove the top layer of skin and often results in skin damage. See Figure 10.13[2] for an illustration of shear and friction forces in the development of pressure injuries.
Hospital-acquired or worsening pressure injuries during hospitalization are considered “never events” meaning they are a serious, preventable medical errors that should never occur and require reporting to The Joint Commission. Additionally, the Centers for Medicare and Medicaid Services (CMS) and many private insurers will no longer pay for additional costs associated with “never events.”[3],[4] Pressure injuries can be prevented with diligent assessment and nursing interventions.
Staging
When assessed, pressure injuries are staged from 1 through 4 based on the extent of tissue damage. For example, Stage 1 pressure injuries have the least amount of tissue damage as evidenced by reddened, intact skin, whereas Stage 4 pressure injuries have the greatest amount of damage with deep, open ulcers affecting underlying tissue, muscle, ligaments, or tendons. See Figure 10.14[5] for images of four stages of pressure injuries.[6] Each stage is further described in the following subsections.

Stage 1 Pressure Injuries
Stage 1 pressure injuries are intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred. Nonblanchable erythema is a medical term used to describe an area of reddened skin that does not turn white when pressed. See Figure 10.15[7] for an illustration of a Stage 1 pressure injury.
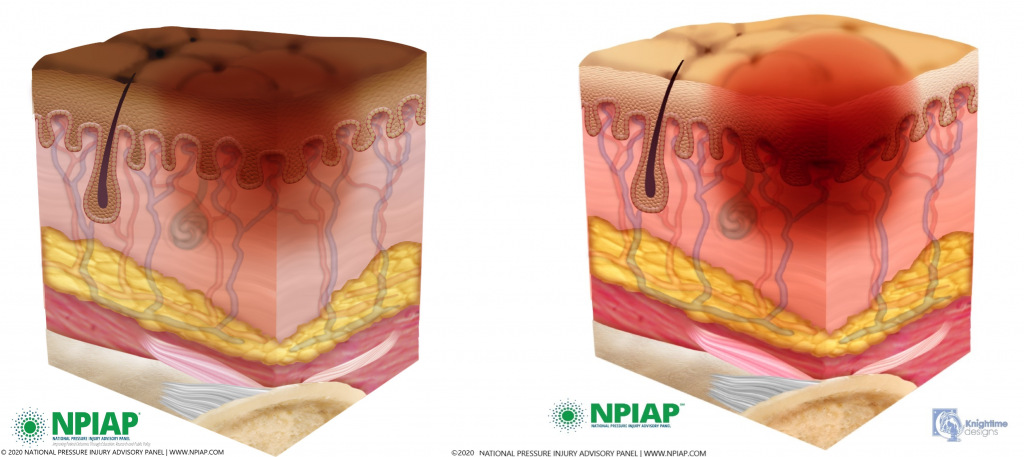
Stage 2 Pressure Injuries
Stage 2 pressure injuries are partial-thickness loss of skin with exposed dermis. The wound bed is viable and may appear like an intact or ruptured blister.[8] See Figure 10.16[9] for an illustration of a Stage 2 pressure injury.
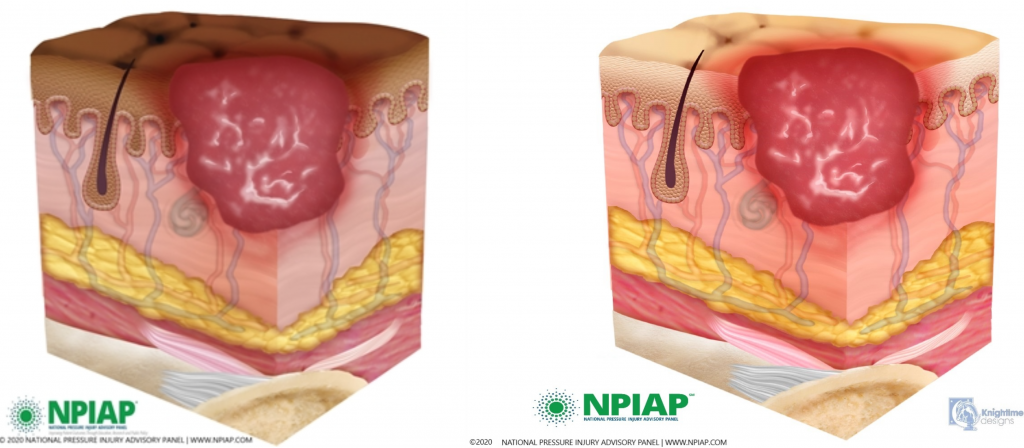
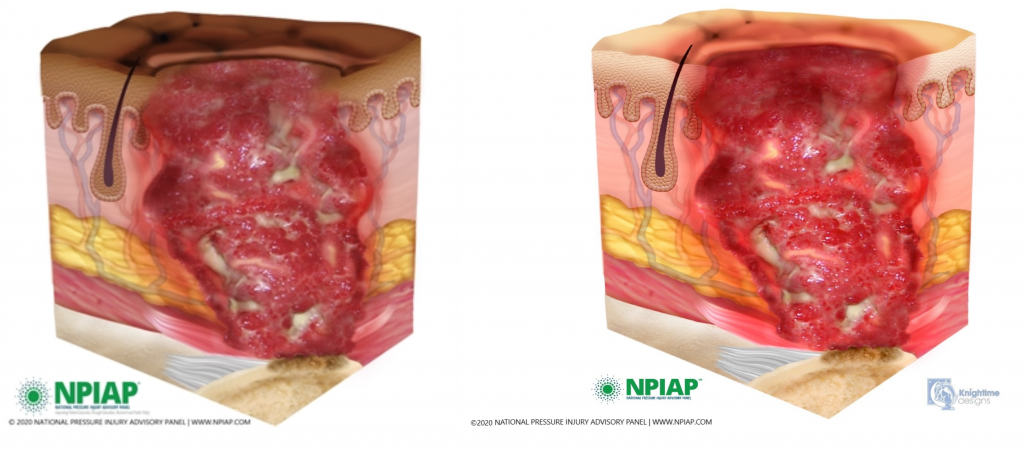
Stage 3 Pressure Injuries
Stage 3 pressure injuries are full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed. The depth of tissue damage varies by anatomical location. See Figure 10.17[10] for an illustration of a Stage 3 pressure injury.
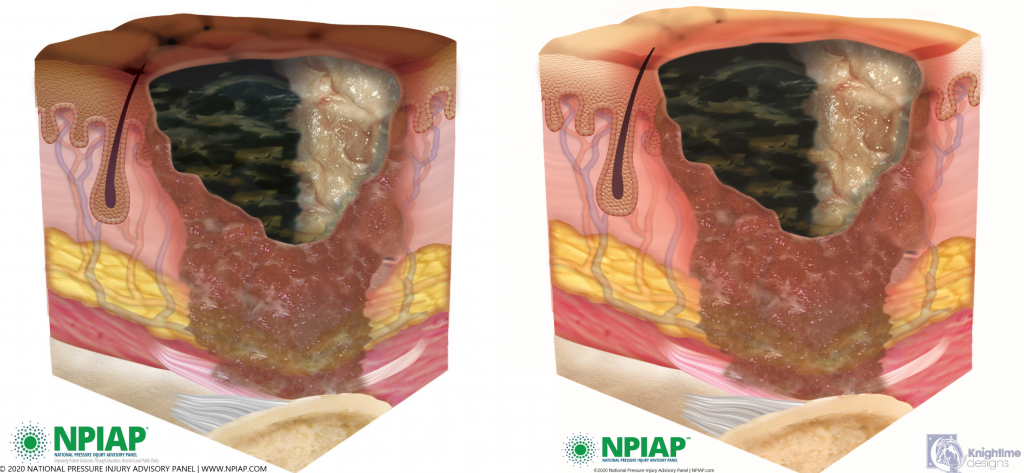
Undermining and tunneling may occur in Stage 3 and 4 pressure injuries. Undermining occurs when the tissue under the wound edge becomes eroded, resulting in a pocket beneath the skin. Tunneling refers to passageways underneath the skin surface that extend from a wound and can take twists and turns.
Slough and eschar may also be present in Stage 3 and 4 pressure injuries. Slough is inflammatory exudate that is usually light yellow, soft, and moist. Eschar is dark brown/black, dry, thick, and leathery dead tissue. If slough or eschar obscures the wound so that tissue loss cannot be assessed, the pressure injury is referred to as unstageable.[11] In most wounds, slough and eschar must be removed by debridement for healing to occur.
Stage 4 Pressure Injuries
Stage 4 pressure injuries are full-thickness tissue loss, like in Stage 3 pressure injuries, but also have exposed cartilage, tendon, ligament, muscle, or bone. Osteomyelitis (bone infection) may also be present.[12] See Figure 10.18[13] for an illustration of a Stage 4 pressure injury.
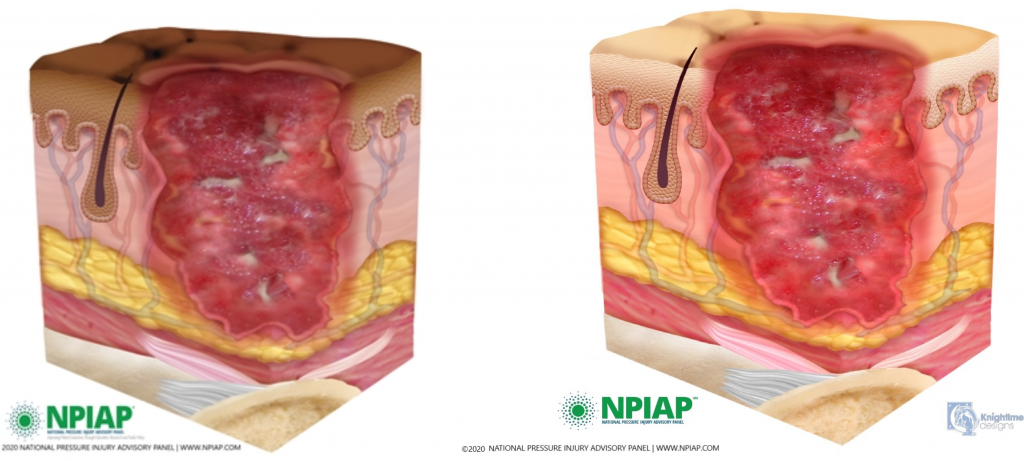
Unstageable Pressure Injuries
Unstageable pressure injuries are full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar were to be removed, a Stage 3 or Stage 4 pressure injury would likely be revealed. However, dry and adherent eschar on the heel or ischemic limb is not typically removed.[14] See Figure 10.19[15] for an illustration of an unstageable pressure ulcer due to the presence of eschar (on the left side of the wound) and slough (on the right side of the wound).
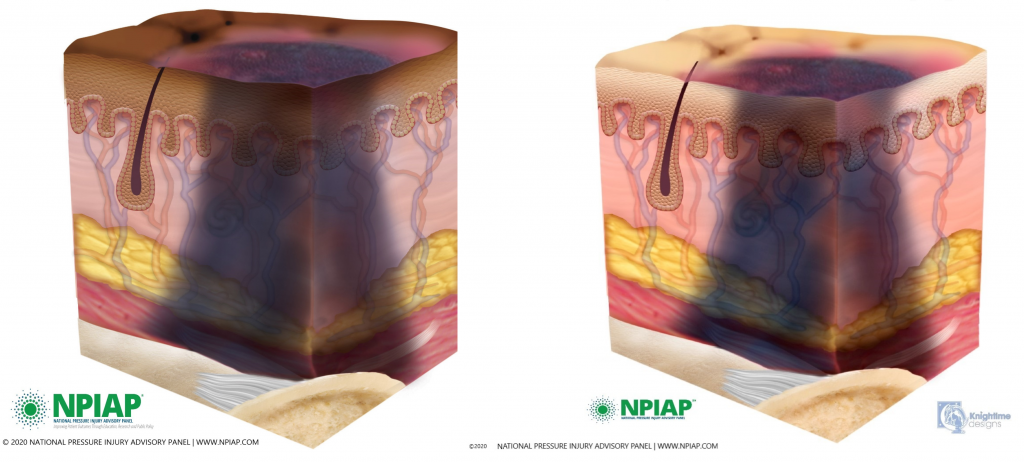
Deep Tissue Pressure Injuries
Deep tissue pressure injuries consist of persistent nonblanchable and deep red, maroon, or purple discoloration of an area. These discolorations typically reveal a dark wound bed or blood-filled blister. Be aware that the discoloration may appear differently in darkly pigmented skin. Deep tissue injury results from intense and/or prolonged pressure, as well as shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or it may resolve without tissue loss.[16],[17] See Figure 10.20 for an illustration of a deep tissue injury.
Video Review of Assessing Pressure Injuries[18]
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- “Shear Force” and “Shear Force Closeup” by Meredith Pomietlo at Chippewa Valley Technical College are licensed under CC BY 4.0 ↵
- Agency for Healthcare Research and Quality. (2019, September). Never events. psnet.ahrq.gov/primer/never-events ↵
- AMN Healthcare Education Services. (2020). Pressure injury: Never event. rn.com/clinical-insight-pressure-injury/ ↵
- “Wound stage.jpg” by Babagolzadeh is licensed under CC BY-SA 3.0 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- "Stage1-Darkly_Pigmented" and “Skin_01__healthy_skin_-_l_pigmen.jpg” provided by National Pressure Injury Advisory Panel are used with permission for educational purposes. Access for free at https://npiap.com/page/PressureInjuryStages ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- "20201202_114031_31850.jpg" and “stage_2_april_2020.jpg” provided by National Pressure Injury Advisory Panel are used with permission for educational purposes. Access for free at https://npiap.com/page/PressureInjuryStages. ↵
- "20201202_114132_23541.jpg" and ”stage_3_april_2020.jpg” provided by National Pressure Injury Advisory Panel are used with permission for educational purposes. Access for free at https://npiap.com/page/PressureInjuryStages ↵
- Davis, C. P. Normal flora. (1996). In S. Baron (Ed.), Medical Microbiology (4th ed.). University of Texas Medical Branch at Galveston. https://www.ncbi.nlm.nih.gov/books/NBK7617/ ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- "20201202_114459_31029.jpg" and "stage_4_april_2020.jpg” provided by National Pressure Injury Advisory Panel are used with permission for educational purposes. Access for free at https://npiap.com/page/PressureInjuryStages ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Stasis dermatitis and ulcers; [updated 2020, Dec 3; reviewed 2018, Oct 14; cited 2020, Dec 10]. https://medlineplus.gov/ency/article/000834.htm ↵
- "Unstageable- Darkly Pigmented_Skin.jpg" and “unstageable-halfslough__1_.jpg” provided by National Pressure Injury Advisory Panel are used with permission for educational purposes. Access for free at https://npiap.com/page/PressureInjuryStages ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- “DTPI-Darkly Pigmented Skin" and "deep_tissue_pressure_injury_.jpg” provided by National Pressure Injury Advisory Panel are used with permission for educational purposes. Access for free at https://npiap.com/page/PressureInjuryStages ↵
- RegisteredNurseRN. (2018, March 7). Pressure ulcers (injuries) stages, prevention, assessment | Stage 1, 2, 3, 4 unstageable NCLEX. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/MDtPik1UE6k ↵
Answer Key to Chapter 14 Learning Activities
Scenario 1
- It would be important to assess Mr. Jones's swallowing, bowel sounds, ability to pass flatus, abdominal distention, and any complaints of nausea.
- When transitioning the patient from NPO status, the patient would be started on clear liquids to ensure dietary tolerance prior to progression toward solid foods.
Scenario 2
- Mrs. Casey's BMI is 15, placing her in the "Underweight" category since it is below 18.5.
- Mrs. Casey's hemoglobin (hgb), white blood cells (WBC), magnesium, and albumin levels are all low, which may be caused by poor intake of protein. Magnesium levels may be low due to intake or can also be caused by excessive alcohol intake.
- The nurse should perform a general survey on Mrs. Casey, paying close attention to her energy level and mobility deficits as a result of the stroke. The nurse should ask Mrs. Casey about her typical 24-hour food intake, appetite, food allergies, and food shopping and preparation activities.
- Imbalanced Nutrition: Less than Body Requirements related to insufficient dietary intake as evidenced by BMI 15 and albumin level 10 g/mL.
- Mrs. Casey's BMI will increase to at least 16 in the next month with a continued upward trend.
- The nurse will contact the provider and request a referral for a dietician. The nurse will contact the facility's social worker regarding promoting nutritional intake with Meals on Wheels and other services. The nurse will monitor food/fluid ingested daily and caloric intake in collaboration with the dietician and encourage nutritional supplements as prescribed. The nurse will encourage the patient to select or order preferred foods for mealtimes. The nurse will ensure that oral care is performed before meals and that foods are presented in an attractive, pleasing manner. The patient will be placed in a seated position before eating, the meal tray set up, and assistance provided according to the patient's needs.
- The nurse will evaluate the effectiveness of interventions by monitoring the patient's weekly weights and assessing if her BMI is trending upward according to the previously established SMART goal.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 15 Learning Activities
Scenario A Answer Key:
- Interpret Mr. Smith's ABG result on admission. The pH is low indicating acidosis. The elevated PaCO2 indicates respiratory acidosis, and the normal HCO3 level indicates is it uncompensated respiratory acidosis.
- Explain the likely cause of the ABG results. The exacerbation of heart failure is likely causing fluid in his alveoli, decreasing ventilation, and causing the retention of carbon dioxide and decreased oxygenation.
- Create a nursing diagnosis for Mr. Smith's fluid status in PES format based on his admission data: Excess Fluid Volume related to excessive fluid intake as evidenced by adventitious breath sounds, edema, and weight gain of 15 pounds over a short period of time.
- What is Mr. Smith’s fluid balance this morning? Support your answer with data. He is demonstrating Deficient Fluid Volume as evidenced by the following signs and symptoms: feeling thirsty and dizzy, having low systolic blood pressure and elevated heart rate and respiratory rate, and lab work showing elevated serum sodium and BUN results.
- What is the probably cause of his fluid balance? Excessive IV diuretics are likely causing dehydration.
- Interpret Mr. Smith's lab results. What are the potential causes of these results? In addition to the lab results indicating fluid volume deficit explained in Answer 4, he is also demonstrating hypokalemia that is likely caused by the diuretics. His creatinine is also elevated, which could indicate kidney disease.
- Create a nursing diagnosis statement in PES format for Mr. Smith's current fluid status: Deficient Fluid Volume related to insufficient fluid intake as evidenced by alteration in mental status, decreased blood pressure, increased heart rate, thirst, and sudden weight loss.
- Create a new expected outcome in SMART format for Mr. Smith: Mr. Smith will demonstrate fluid balance within 24 hours as evidenced by moist mucus membranes and 24-hour intake and output balance.
- In addition to providing intravenous fluids, what additional interventions will you implement for Mr. Smith? Additional interventions include weigh daily, monitor intake and output every four hours, provide fresh water and fluids preferred by the patient, administer oral potassium replacements as ordered, and monitor for signs of fluid volume excess while receiving IV fluids.
- How will you evaluate if the nursing interventions are effective? As stated in the SMART outcome, the nurse will evaluate for moist mucus membranes and balanced intake and output in 24 hours.
Scenario B Answer Key:
1. What is Mr. M.’s fluid balance? Provide data supporting the imbalance. Mr. M. is exhibiting Deficient Fluid Volume. His blood pressure is decreased and his heart rate is tachycardic. His serum osmolarity, hematocrit, urine specific gravity, and BUN are elevated.
2. What is your interpretation of Mr. M.’s ABGs?
Step 1: pH 7.30 is below 7.35, so it is acidic and abnormal. We know this will be an acidosis.
Step 2: PaCO2 50. This is above 45, so it is acidic. The PaCO2 is moving in the opposite direction of the pH, so we know this will be respiratory in nature. This is called Respiratory Acidosis.
Step 3: HCO3 24. This is a normal HCO3 level so we know the problem is not metabolic in nature. We also know the kidneys are not trying to compensate for the lung problems.
Step 4: Compensation: The pH is abnormal, so there is not complete compensation. The HCO3 is normal, so the kidneys are not trying to compensate for the lungs. We call this uncompensated.
Interpretation: Uncompensated Respiratory Acidosis
3. What is your interpretation of Mr. M.’s electrolyte studies?
Potassium: 5.9 - elevated, most likely due to acidosis occurring
Magnesium: 1.0 - low, most likely due to alcoholism or inadequate nutrition
Calcium: 10.2 - elevated, most likely due to acidosis occurring
Sodium: 137 - normal
4. Is Mr. M. stable or unstable? Why? Mr. M. is unstable. He is hypotensive and tachycardic. Also, his respiratory rate is low and labored, and O2 saturations are quite low. His acid-base balance is quite abnormal. He is developing hypovolemic shock and could experience cardiac and respiratory arrest if not treated emergently.
5. For what complications will you monitor? Mr. M. could have a respiratory arrest due to his severe acidosis, decreased level of consciousness, and respiratory distress. The elevated potassium and decreased magnesium put Mr. M. at risk for cardiac arrhythmias. His elevated calcium level could cause nausea and vomiting, which puts him at risk for aspiration with his associated lethargy.
6. Write an SBAR communication you would have with the health care provider to notify them about Mr. M.’s condition.
S: Hi, Dr. X. This is ________, a nursing student working with Mr. M. This morning Mr. M. is lethargic and having labored respirations.
B: Mr. M. was admitted during the night with pneumonia. He has a history of alcohol abuse and coronary artery disease.
A: Mr. M.’s vital signs are the following: BP 80/45, HR 110, RR 8, O2 saturation 80% on 3 L/NC. He has coarse crackles throughout his lung fields, and he is using accessory muscles to breathe. Mr. M. is lethargic and having difficulty following commands.
R: I am concerned that Mr. M.’s respiratory status is declining. I recommend increasing his oxygen and checking arterial blood gasses and electrolyte studies. I also would like you to come see Mr. M.
7. Create a NANDA-I diagnosis for Mr. M. in PES format. Fluid Volume Deficit related to insufficient fluid intake as evidenced by BP 80/45, HR 110, and elevated serum osmolarity, hematocrit, BUN, and urine specific gravity results.
8. Identify an expected outcome for Mr. M. in SMART format. Mr. M. will demonstrate improving fluid balance as demonstrated by blood pressure and heart rate returning within normal range within 8 hours.
9. What interventions will you plan for Mr. M.? Mr. M. will need either a BiPAP or intubation and mechanical ventilation for his respiratory status. He will need magnesium supplementation, and his calcium and potassium will need to be monitored closely. He may need insulin to help decrease his potassium. Any potassium contained in IV fluids should be stopped to prevent further potassium buildup. He will also need antibiotics for his pneumonia and IV fluids to treat his hypotension and tachycardia.
10. How will you evaluate if your interventions are effective? Based on the SMART goal established, the nurse will monitor Mr. M.'s blood pressure and heart rate and evaluate if they have returned to normal within 8 hours. Additionally, the ABGs for Mr. M. should return to closer to normal. He will show improvement with his level of consciousness. Magnesium levels will return to normal. As Mr. M.’s pH normalizes, the calcium and potassium levels should return to normal. Mr. M.’s fever should subside and his vital signs should return to normal as the infection is treated and IV fluids are given.
11. Write a nursing note about Mr. M.’s condition and your actions taken. This can be in the form of a DAR, SOAP, or summary nursing note.
01/31/20xx 0900
D: On morning assessment, pt noted to be lethargic, unable to follow commands consistently, and using accessory muscles with breathing. Coarse crackles noted throughout lung fields. VS are BP 80/45, HR 110, RR 8, O2 sat 80% on 3L per nasal cannula, and temp 38.1 C.
A: Dr. X. notified and orders rec’d to increase O2 to 10L per non-rebreather mask and to check electrolytes and ABGs.
R: O2 increased and labs drawn and resulted as follows: pH 7.30, PaCO2 50, PaO2 59, HCO3 24, SaO2 80. Potassium 5.9, Magnesium 1.0, Calcium 10.2, Sodium 137. Will continue to monitor patient closely and will update Dr. X. of changes.
________,SN
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 15 Learning Activities
Scenario A Answer Key:
- Interpret Mr. Smith's ABG result on admission. The pH is low indicating acidosis. The elevated PaCO2 indicates respiratory acidosis, and the normal HCO3 level indicates is it uncompensated respiratory acidosis.
- Explain the likely cause of the ABG results. The exacerbation of heart failure is likely causing fluid in his alveoli, decreasing ventilation, and causing the retention of carbon dioxide and decreased oxygenation.
- Create a nursing diagnosis for Mr. Smith's fluid status in PES format based on his admission data: Excess Fluid Volume related to excessive fluid intake as evidenced by adventitious breath sounds, edema, and weight gain of 15 pounds over a short period of time.
- What is Mr. Smith’s fluid balance this morning? Support your answer with data. He is demonstrating Deficient Fluid Volume as evidenced by the following signs and symptoms: feeling thirsty and dizzy, having low systolic blood pressure and elevated heart rate and respiratory rate, and lab work showing elevated serum sodium and BUN results.
- What is the probably cause of his fluid balance? Excessive IV diuretics are likely causing dehydration.
- Interpret Mr. Smith's lab results. What are the potential causes of these results? In addition to the lab results indicating fluid volume deficit explained in Answer 4, he is also demonstrating hypokalemia that is likely caused by the diuretics. His creatinine is also elevated, which could indicate kidney disease.
- Create a nursing diagnosis statement in PES format for Mr. Smith's current fluid status: Deficient Fluid Volume related to insufficient fluid intake as evidenced by alteration in mental status, decreased blood pressure, increased heart rate, thirst, and sudden weight loss.
- Create a new expected outcome in SMART format for Mr. Smith: Mr. Smith will demonstrate fluid balance within 24 hours as evidenced by moist mucus membranes and 24-hour intake and output balance.
- In addition to providing intravenous fluids, what additional interventions will you implement for Mr. Smith? Additional interventions include weigh daily, monitor intake and output every four hours, provide fresh water and fluids preferred by the patient, administer oral potassium replacements as ordered, and monitor for signs of fluid volume excess while receiving IV fluids.
- How will you evaluate if the nursing interventions are effective? As stated in the SMART outcome, the nurse will evaluate for moist mucus membranes and balanced intake and output in 24 hours.
Scenario B Answer Key:
1. What is Mr. M.’s fluid balance? Provide data supporting the imbalance. Mr. M. is exhibiting Deficient Fluid Volume. His blood pressure is decreased and his heart rate is tachycardic. His serum osmolarity, hematocrit, urine specific gravity, and BUN are elevated.
2. What is your interpretation of Mr. M.’s ABGs?
Step 1: pH 7.30 is below 7.35, so it is acidic and abnormal. We know this will be an acidosis.
Step 2: PaCO2 50. This is above 45, so it is acidic. The PaCO2 is moving in the opposite direction of the pH, so we know this will be respiratory in nature. This is called Respiratory Acidosis.
Step 3: HCO3 24. This is a normal HCO3 level so we know the problem is not metabolic in nature. We also know the kidneys are not trying to compensate for the lung problems.
Step 4: Compensation: The pH is abnormal, so there is not complete compensation. The HCO3 is normal, so the kidneys are not trying to compensate for the lungs. We call this uncompensated.
Interpretation: Uncompensated Respiratory Acidosis
3. What is your interpretation of Mr. M.’s electrolyte studies?
Potassium: 5.9 - elevated, most likely due to acidosis occurring
Magnesium: 1.0 - low, most likely due to alcoholism or inadequate nutrition
Calcium: 10.2 - elevated, most likely due to acidosis occurring
Sodium: 137 - normal
4. Is Mr. M. stable or unstable? Why? Mr. M. is unstable. He is hypotensive and tachycardic. Also, his respiratory rate is low and labored, and O2 saturations are quite low. His acid-base balance is quite abnormal. He is developing hypovolemic shock and could experience cardiac and respiratory arrest if not treated emergently.
5. For what complications will you monitor? Mr. M. could have a respiratory arrest due to his severe acidosis, decreased level of consciousness, and respiratory distress. The elevated potassium and decreased magnesium put Mr. M. at risk for cardiac arrhythmias. His elevated calcium level could cause nausea and vomiting, which puts him at risk for aspiration with his associated lethargy.
6. Write an SBAR communication you would have with the health care provider to notify them about Mr. M.’s condition.
S: Hi, Dr. X. This is ________, a nursing student working with Mr. M. This morning Mr. M. is lethargic and having labored respirations.
B: Mr. M. was admitted during the night with pneumonia. He has a history of alcohol abuse and coronary artery disease.
A: Mr. M.’s vital signs are the following: BP 80/45, HR 110, RR 8, O2 saturation 80% on 3 L/NC. He has coarse crackles throughout his lung fields, and he is using accessory muscles to breathe. Mr. M. is lethargic and having difficulty following commands.
R: I am concerned that Mr. M.’s respiratory status is declining. I recommend increasing his oxygen and checking arterial blood gasses and electrolyte studies. I also would like you to come see Mr. M.
7. Create a NANDA-I diagnosis for Mr. M. in PES format. Fluid Volume Deficit related to insufficient fluid intake as evidenced by BP 80/45, HR 110, and elevated serum osmolarity, hematocrit, BUN, and urine specific gravity results.
8. Identify an expected outcome for Mr. M. in SMART format. Mr. M. will demonstrate improving fluid balance as demonstrated by blood pressure and heart rate returning within normal range within 8 hours.
9. What interventions will you plan for Mr. M.? Mr. M. will need either a BiPAP or intubation and mechanical ventilation for his respiratory status. He will need magnesium supplementation, and his calcium and potassium will need to be monitored closely. He may need insulin to help decrease his potassium. Any potassium contained in IV fluids should be stopped to prevent further potassium buildup. He will also need antibiotics for his pneumonia and IV fluids to treat his hypotension and tachycardia.
10. How will you evaluate if your interventions are effective? Based on the SMART goal established, the nurse will monitor Mr. M.'s blood pressure and heart rate and evaluate if they have returned to normal within 8 hours. Additionally, the ABGs for Mr. M. should return to closer to normal. He will show improvement with his level of consciousness. Magnesium levels will return to normal. As Mr. M.’s pH normalizes, the calcium and potassium levels should return to normal. Mr. M.’s fever should subside and his vital signs should return to normal as the infection is treated and IV fluids are given.
11. Write a nursing note about Mr. M.’s condition and your actions taken. This can be in the form of a DAR, SOAP, or summary nursing note.
01/31/20xx 0900
D: On morning assessment, pt noted to be lethargic, unable to follow commands consistently, and using accessory muscles with breathing. Coarse crackles noted throughout lung fields. VS are BP 80/45, HR 110, RR 8, O2 sat 80% on 3L per nasal cannula, and temp 38.1 C.
A: Dr. X. notified and orders rec’d to increase O2 to 10L per non-rebreather mask and to check electrolytes and ABGs.
R: O2 increased and labs drawn and resulted as follows: pH 7.30, PaCO2 50, PaO2 59, HCO3 24, SaO2 80. Potassium 5.9, Magnesium 1.0, Calcium 10.2, Sodium 137. Will continue to monitor patient closely and will update Dr. X. of changes.
________,SN
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 16 Learning Activities
1. Mrs. Gonzalez should be offered therapeutic reassurance that although urinary incontinence can be the result of aging, there are interventions that can be helpful. These include pelvic muscle exercises, timed voiding to assist in regaining bladder control, avoidance of triggering agents such as caffeine, weight control, and avoidance of heavy lifting, etc. Additional medical intervention may include biofeedback sensors, pessaries, anticholinergic medications, or surgical intervention. The patient should also be educated on protective products that can help protect the skin from breakdown and assist with odor control.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 19 Learning Activities
The SPICES tool can assess many common problems for aging adults.
S: Sleep Disorders
Examples of questions might include the following:
What length of rest periods do you have during the night? Do you rise frequently? How many times per night? Do you nap during the day? Where do you sleep?
P: Problems with Eating or Feeding
Examples of questions might include the following:
Do you notice difficulty swallowing foods or beverages? Do you choke after swallowing? Do you ever experience a sensation of food being caught in the throat?
I: Incontinence
Examples of questions might include the following:
Do you experience frequent urination? Do you feel a sense of urgency or that you will not reach the bathroom in time to void? Do you feel that you are able to empty your bladder completely?
C: Confusion
Examples of questions might include the following:
Who are you? Where are you? Who is the President? Do you ever experience difficulty remembering why you entered a certain room? Do you find yourself forgetting things or people you previously knew? Do your loved ones report that you have memory issues?
E: Evidence of Falls
Examples of questions might include the following:
Have you experienced a recent fall? What are the bruises on your arms or legs attributed to? Do you feel unsteady or stumble when first arising out of bed?
S: Skin Breakdown
Examples of questions might include the following:
Do you have any open areas on your skin? Do you have areas of redness that do not go away? Are you able to reposition yourself frequently or do you rely on the assistance of others?
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 16 Learning Activities
1. Mrs. Gonzalez should be offered therapeutic reassurance that although urinary incontinence can be the result of aging, there are interventions that can be helpful. These include pelvic muscle exercises, timed voiding to assist in regaining bladder control, avoidance of triggering agents such as caffeine, weight control, and avoidance of heavy lifting, etc. Additional medical intervention may include biofeedback sensors, pessaries, anticholinergic medications, or surgical intervention. The patient should also be educated on protective products that can help protect the skin from breakdown and assist with odor control.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 17 Learning Activities
Scenario A
1. What actions should the nurse take to support Mr. Lyn? The grieving process is variable for every individual. Mr. Lyn's outward expression of grief should be supported by the nurse. The nurse can assist Mr. Lyn to cope by using supportive presence and encouraging reminiscence by sharing good memories of his life with Mrs. Lyn. It is helpful to offer the services of the agency chaplain, as well as to offer prayer and spiritual support based on Mr. Lyn's beliefs and the nurse's comfort level. The nurse can also encourage Mr. Lyn to contact other family members and friends for additional social support.
2. What medication is helpful to administer to treat dyspnea at end of life? Roxanol, a highly concentrated solution of morphine, can be administered sublingually as ordered for pain and air hunger.
3. Mr. Lyn tells the nurse, "My daughter lives six hours away and would like to be here when the time comes. How much longer does she have to live?" What is the nurse's best response? Although we never know exactly when death will occur, there are recognizable signs that occur as death becomes imminent, such as noisy or irregular breathing, increased lethargy, and a type of bruising called "mottling." Mrs. Lyn is demonstrating new changes in her breathing status, so death may occur in the next few days.
4. The daughter arrives and seems hesitant to talk to or touch the patient. What tasks can the nurse coach family members to do at the end of a patient's life? Nurses can encourage family members to talk with and touch their loved one. They can encourage family members to reminisce about happy stories and say "I love you" or say "Goodbye."
5. Mrs. Lyn dies the following evening. What postmortem care should the nurse provide? After verifying the lack of an apical heartbeat for a full minute, the nurse should follow agency policy regarding notifications and postmortem care. The nurse should document the date and time of assessment, the physician contacted, the individuals present at the time of death, the lack of response to stimuli and absence of an apical pulse, and the arrangements for transport to the morgue or funeral home. Typically, the patient is bathed, dressed, and positioned to show respect and provide dignity. Cultural practices should be honored. The nurse can offer to contact other family members to inform them of the death and support families in their ways of saying goodbye.
Scenario B
- According to Kubler-Ross’ theory of grief/loss, what stage of grief is Terry currently experiencing? Terry is demonstrating the stage of denial according to Kubler-Ross’ theory of grief/loss.
- How would you explain palliative care to him? Palliative care is a way to manage your symptoms and optimize your quality of life. A team will assist you in making difficult decisions and can provide support to you and your family members
- How would you explain advance directives to him? Advance directives are a legal way for you to establish your wishes for health care. A living will is a document that you can complete that describes your wishes if you are no longer able to speak for yourself. For example, you can decide if you would ever want a feeding tube placed if you are no longer able to eat. You can also identify a health care power of attorney who will serve as your decision maker when you can no longer speak for yourself. Would you like me to ask a social worker to visit so you can talk more about these options?
- Identify a SMART outcome. "Terry will discuss the meaning of the cancer diagnosis to his life before discharge."
- List sample nursing interventions that may help Terry to cope with this new diagnosis. Use a calm, reassuring approach. Provide an atmosphere of acceptance. Seek to understand the patient's perspective. Provide Terry realistic choices about aspects of his care when possible. Encourage verbalization of feelings, perceptions, and fears. Encourage support from family and friends.
Answers to interactive elements are given within the interactive element.
Template for Creating a Nursing Care Plan
Sample Abbreviated Care Plan for Scenario C
:root {
--primary: #525564 !important;
--accent: #888590 !important;
--primary-dark: #525564 !important;
--accent-dark: #888590 !important;
}
.nav-reading__next a:hover, .nav-reading__previous a:hover {
background: #3f4350; }
.header__logo--img, .header__logo--svg {
max-width: 242px;
max-height: 79px;
}
.header {
padding: 1.5rem 1rem 3em;
}
.reading-header {
margin-top: 1.3rem;
}
.a11y-toolbar {
width: auto;
right: 0px;
}
.nav-reading__up {
left: 30px;
left: 2.25rem;
top: -3.5rem;
transition: 0.75s all;
}
.nav-reading {
width: 100% !important;
}
main .front-matter h1, main .part h1, main .chapter h1, main .back-matter h1,
main .front-matter h2, main .part h2, main .chapter h2, main .back-matter h2,
main .front-matter h3, main .part h3, main .chapter h3, main .back-matter h3,
main .front-matter h4, main .part h4, main .chapter h4, main .back-matter h4,
main .front-matter h5, main .part h5, main .chapter h5, main .back-matter h5 {
color: #525564;
}
main .front-matter h1, main .part h1, main .chapter h1, main .back-matter h1 {
font-size:32px;
text-transform:uppercase;
}
main .front-matter h2, main .part h2, main .chapter h2, main .back-matter h2 {
font-size:28px;
font-weight:bold;
}
main .front-matter h3, main .part h3, main .chapter h3, main .back-matter h3 {
font-size:24px;
margin-top:1.5em !important;
margin-bottom:0.8em !important;
}
main .front-matter h4, main .part h4, main .chapter h4, main .back-matter h4 {
font-size:20px;
text-transform:uppercase;
font-weight:bold;
font-style:normal;
}
main .front-matter h5, main .part h5, main .chapter h5, main .back-matter h5 {
font-size:18px;
font-weight:bold;
}
div.footnotes li {
font-size: 12px;
}
section.front-matter header h1 + [data-type='author'], section.back-matter header h1 + [data-type='author'], section.chapter header h1 + [data-type='author'] {
margin-top: .5em;
font-size: 18px;
text-transform: uppercase;
font-weight: bold;
color: #96bfcc;
}
section.chapter header, section.front-matter header, section.back-matter header {
border-bottom: 1px solid #525564;
}
.chapter-number, .entry-title span {
color: #525564;
}
.textbox.shaded, .bcc-box.shaded {
background-color: #e6e7e8;
}
main div.textbox p,
main div.textbox h2,
main div.textbox h3,
main div.textbox h4,
main div.textbox ul {
margin-left:2%;
margin-right:2%;
}
.front-matter p, .part p, .chapter p, .back-matter p, body#tinymce.wp-editor p {
text-align: left;
}
.textbox, .bcc-box {
text-align: left;
background-color: white;
border-color: #525564;
padding: 2em 2em 2em 2em;
font-size: 16px;
line-height: 1.6;
}
section.chapter header, section.front-matter header, section.back-matter header {
border-bottom: 1px solid #525564;
}
.front-matter h2, .part h2, .chapter h2, .back-matter h2, body#tinymce.wp-editor h2 {
margin-top: 1em;
padding-bottom: 0;
font-family: 'Raleway', sans-serif;
font-size: 1.5em;
font-style: normal;
font-weight: 500;
line-height: 1.6em;
text-transform: none;
letter-spacing: normal;
word-spacing: normal;
}
.front-matter h4, .part h4, .chapter h4, .back-matter h4 {
color: #525564;
}
.textbox h2,
.textbox h3 {
margin-left: 1.5em;
font-weight: bolder;
}
div.textbox p, div.bcc-box p, div.textbox ul, div.bcc-box ul, div.textbox ol, div.bcc-box ol {
margin-left: 1.5em;
margin-right: 1.5em;
}
.textbox.textbox--learning-objectives .textbox__header, .bcc-box.textbox--learning-objectives .textbox__header {
background: #74828f;
}
div.textbox h1 {
color: #ffffff;
margin: .2em .5em .2em 1em !important;
text-transform: none !important;
}
.textbox.textbox--examples .textbox__header, .bcc-box.textbox--examples .textbox__header {
border-bottom: 5px solid #96bfcc;
}
.front-matter table p, .part table p, .chapter table p, .back-matter table p, body#tinymce.wp-editor table p {
font-size: 1em;
}
:root {
--reading-width: 60em !important;
}
.front-matter .wp-caption figcaption, .part .wp-caption figcaption, .chapter .wp-caption figcaption, .back-matter .wp-caption figcaption, .front-matter .wp-caption .wp-caption-text, .part .wp-caption .wp-caption-text, .chapter .wp-caption .wp-caption-text, .back-matter .wp-caption .wp-caption-text {
color: #000000;
}
.textbox.textbox--examples, .bcc-box.textbox--examples {
background: #f3f4f5;
}
.annotator-frame .annotator-bucket-bar {
background:none !important;
}
.embed-responsive {
position:relative;
display:block;
width:100%;
padding:0;
overflow:hidden;
}
.embed-responsive::before {
display:block;
content:"";
}
.embed-responsive .embed-responsive-item,
.embed-responsive iframe,
.embed-responsive embed,
.embed-responsive object,
.embed-responsive video {
position:absolute;
top:0;
bottom:0;
left:0;
width:100%;
height:100%;
border:0;
}
.embed-responsive-21by9::before {
padding-top:42.857143%;
}
.embed-responsive-16by9::before {
padding-top:56.25%;
}
.embed-responsive-4by3::before {
padding-top:75%;
}
.embed-responsive-1by1::before {
padding-top:100%;
}
figure figcaption {
padding-top:8px;
}
div.h5p-iframe-wrapper {
margin-top:20px;
}
p.small {
font-size:1rem;
}
table tr td,
table tr th {
vertical-align:top !important;
line-height:1.5em !important;
}
table.grid h5 {
font-weight:bold;
margin:5px 0;
}
header.textbox__header h2 {
color:#FFFFFF;
font-size:30px;
margin:0 30px;
text-transform:uppercase;
}
iv.footnotes li {
font-size: 12px;
}
section.chapter header h1 {
text-transform: uppercase;
font-size: 32px;
}
header.textbox__header h2 {
color: #FFFFFF;
font-size: 24px;
margin: 0 30px;
text-transform: none;
}
ol, p, ul, td {
font-size: 16px;
line-height: 1.6;
padding-top: 5px;
}
main#main div#content ul {
margin-top:0.75em;
margin-bottom:1em;
}
main#main div#content td > ul:first-child {
margin-top: 0 !important;
}
main#main div#content td ul {
list-style:disc;
}
main#main div#content section header ~ ol > li > ul ul {
list-style:circle;
}
main#main div#content section header ~ ol > li + li {
padding-top:20px
}
main#main div#content section header ~ ol > li li + li {
padding-top:15px
}
li > ul:last-child,
li > ol:last-child {
margin-bottom: 0 !important;
}
.front-matter h2, .part h2, .chapter h2, .back-matter h2, body#tinymce.wp-editor h2 {
margin-top: 1em;
padding-bottom: 0;
font-family: 'Raleway', sans-serif;
font-size: 28px;
font-style: normal;
font-weight: 500;
line-height: 1.6em;
text-transform: none;
letter-spacing: normal;
word-spacing: normal;
color: #525564;
margin-bottom: -0.5em;
}
.front-matter h4, .part h4, .chapter h4, .back-matter h4 {
color: #525564;
font-size: 22px;
font-weight: 700;
padding-bottom: 10px;
margin-bottom: -.95em !important;
}
.front-matter .wp-caption.alignnone, .part .wp-caption.alignnone, .chapter .wp-caption.alignnone, .back-matter .wp-caption.alignnone, .front-matter .wp-nocaption.alignnone, .part .wp-nocaption.alignnone, .chapter .wp-nocaption.alignnone, .back-matter .wp-nocaption.alignnone {
padding-left: 0;
margin: 0.5em 0 1.5em;
text-align: left;
width: auto !important;
}
.textbox.textbox--examples .textbox__header, .bcc-box.textbox--examples .textbox__header {
border-bottom:0 !important;
}
main div.textbox.textbox--examples {
margin-top:40px;
margin-bottom:40px;
}
main .arrow {
display:inline-block;
background-image: url(https://wtcs.pressbooks.pub/app/uploads/sites/10/2020/01/link-arrow.png);
background-size: auto 18px;
background-repeat: no-repeat;
background-position: top 3px left;
padding-left: 17px;
padding-bottom: 10px;
}
main p.arrow {
background-position: top 8px left;
}
.star {
background-image: url(https://wtcs.pressbooks.pub/app/uploads/sites/10/2020/04/star.png);
background-size: auto 22px;
background-repeat: no-repeat;
background-position: top 3px left;
padding-left: 17px;
padding-right: 17px;
}
.video {
background-image: url(https://wtcs.pressbooks.pub/app/uploads/sites/10/2020/04/video-01.png);
background-size: auto 26px;
background-repeat: no-repeat;
background-position: top 3px left;
padding-left: 39px;
padding-right: 17px;
background-position: 2px;
background-position-x: 2px;
background-position-y: center;
}
ul.search-results h2 {
margin-bottom: .35em;
}
main .front-matter h2, main .part h2, main .chapter h2, main .back-matter h2 {
font-size: 20px;
font-weight: bold;
}
.textbox.textbox--exercises .textbox__header, .textbox--exercises.bcc-box .textbox__header {
background: #3F4350;
border-top-left-radius: 0;
border-top-right-radius: 0;
color: #fff;
font-size: 0.9em;
font-style: italic;
font-weight: normal;
margin: 0;
padding: 1.7777777778em 1.7777777778em 1.7777777778em 1.7777777778em;
text-align: left;
}
.textbox.textbox--exercises, .textbox--exercises.bcc-box {
margin-bottom: 1.35em;
padding: 0;
border-radius: 0;
border-style: none;
border-width: 0;
color: #000000;
background: #f6f6f6;
}
.textbox.textbox--exercises .textbox__header, .bcc-box.textbox--exercises .textbox__header {
border-bottom: 5px solid #3F4350;
}
div.textbox img.alignleft {
margin: -20px 20px 5px -15px;
width: 90px;
}
.textbox.textbox--learning-objectives, .textbox--learning-objectives.bcc-box {
margin-bottom: 1.35em;
padding: 0;
border-radius: 0;
border-style: none;
border-width: 0;
color: #000;
background: #f6f6f6;
}
p:empty {
display:none;
}
main div.textbox p, main div.bcc-box p, main div.textbox h2, main div.bcc-box h2, main div.textbox h3, main div.bcc-box h3, main div.textbox h4, main div.bcc-box h4, main div.textbox ul, main div.bcc-box ul {
margin-left: 2%;
margin-right: 2%;
}
div.textbox.min-height {
min-height: 200px;
}
div.learning-activities {
padding-left: 30px;
padding-right: 30px;
padding-bottom: 20px;
padding-top: 20px;
}
/*
ol.offset-start {
list-style: none;
counter-increment: start 1;
}
ol.offset-start-13 {
counter-increment: start 12;
}
ol.offset-start > li::before {
content: counter(start) ". ";
counter-increment: start;
}
*/
li.hide {
visibility:hidden;
height:0 !important;
max-height:0 !important;
margin:0 !important;
padding:0 !important;
}
li.hide + li {
padding-top:0 !important;
}
Answer Key to Chapter 17 Learning Activities
Scenario A
1. What actions should the nurse take to support Mr. Lyn? The grieving process is variable for every individual. Mr. Lyn's outward expression of grief should be supported by the nurse. The nurse can assist Mr. Lyn to cope by using supportive presence and encouraging reminiscence by sharing good memories of his life with Mrs. Lyn. It is helpful to offer the services of the agency chaplain, as well as to offer prayer and spiritual support based on Mr. Lyn's beliefs and the nurse's comfort level. The nurse can also encourage Mr. Lyn to contact other family members and friends for additional social support.
2. What medication is helpful to administer to treat dyspnea at end of life? Roxanol, a highly concentrated solution of morphine, can be administered sublingually as ordered for pain and air hunger.
3. Mr. Lyn tells the nurse, "My daughter lives six hours away and would like to be here when the time comes. How much longer does she have to live?" What is the nurse's best response? Although we never know exactly when death will occur, there are recognizable signs that occur as death becomes imminent, such as noisy or irregular breathing, increased lethargy, and a type of bruising called "mottling." Mrs. Lyn is demonstrating new changes in her breathing status, so death may occur in the next few days.
4. The daughter arrives and seems hesitant to talk to or touch the patient. What tasks can the nurse coach family members to do at the end of a patient's life? Nurses can encourage family members to talk with and touch their loved one. They can encourage family members to reminisce about happy stories and say "I love you" or say "Goodbye."
5. Mrs. Lyn dies the following evening. What postmortem care should the nurse provide? After verifying the lack of an apical heartbeat for a full minute, the nurse should follow agency policy regarding notifications and postmortem care. The nurse should document the date and time of assessment, the physician contacted, the individuals present at the time of death, the lack of response to stimuli and absence of an apical pulse, and the arrangements for transport to the morgue or funeral home. Typically, the patient is bathed, dressed, and positioned to show respect and provide dignity. Cultural practices should be honored. The nurse can offer to contact other family members to inform them of the death and support families in their ways of saying goodbye.
Scenario B
- According to Kubler-Ross’ theory of grief/loss, what stage of grief is Terry currently experiencing? Terry is demonstrating the stage of denial according to Kubler-Ross’ theory of grief/loss.
- How would you explain palliative care to him? Palliative care is a way to manage your symptoms and optimize your quality of life. A team will assist you in making difficult decisions and can provide support to you and your family members
- How would you explain advance directives to him? Advance directives are a legal way for you to establish your wishes for health care. A living will is a document that you can complete that describes your wishes if you are no longer able to speak for yourself. For example, you can decide if you would ever want a feeding tube placed if you are no longer able to eat. You can also identify a health care power of attorney who will serve as your decision maker when you can no longer speak for yourself. Would you like me to ask a social worker to visit so you can talk more about these options?
- Identify a SMART outcome. "Terry will discuss the meaning of the cancer diagnosis to his life before discharge."
- List sample nursing interventions that may help Terry to cope with this new diagnosis. Use a calm, reassuring approach. Provide an atmosphere of acceptance. Seek to understand the patient's perspective. Provide Terry realistic choices about aspects of his care when possible. Encourage verbalization of feelings, perceptions, and fears. Encourage support from family and friends.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 18 Learning Activities
1. These questions can be asked to gain insight into the patient's personal spiritual beliefs:
F--Faith or beliefs: What are your spiritual beliefs? Do you consider yourself spiritual? What things do you believe in that give meaning to life?
I--Importance and influence: Is faith/spirituality important to you? How has your illness and/or hospitalization affected your personal practices /beliefs?
C--Community: Are you connected with a faith center in the community? Does it provide support/comfort for you during times of stress? Is there a person/group/leader who supports/assists you in your spirituality?
A--Address: What support can we provide to support your spiritual beliefs/practices?
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 18 Learning Activities
1. These questions can be asked to gain insight into the patient's personal spiritual beliefs:
F--Faith or beliefs: What are your spiritual beliefs? Do you consider yourself spiritual? What things do you believe in that give meaning to life?
I--Importance and influence: Is faith/spirituality important to you? How has your illness and/or hospitalization affected your personal practices /beliefs?
C--Community: Are you connected with a faith center in the community? Does it provide support/comfort for you during times of stress? Is there a person/group/leader who supports/assists you in your spirituality?
A--Address: What support can we provide to support your spiritual beliefs/practices?
Answers to interactive elements are given within the interactive element.

