Integumentary
10.3 Wounds
Phases of Wound Healing
When skin is injured, there are four phases of wound healing that take place: hemostasis, inflammatory, proliferative, and maturation. See Figure 10.10[1] for an illustration of wound healing demonstrating hemostasis/inflammation, proliferation, and maturation.
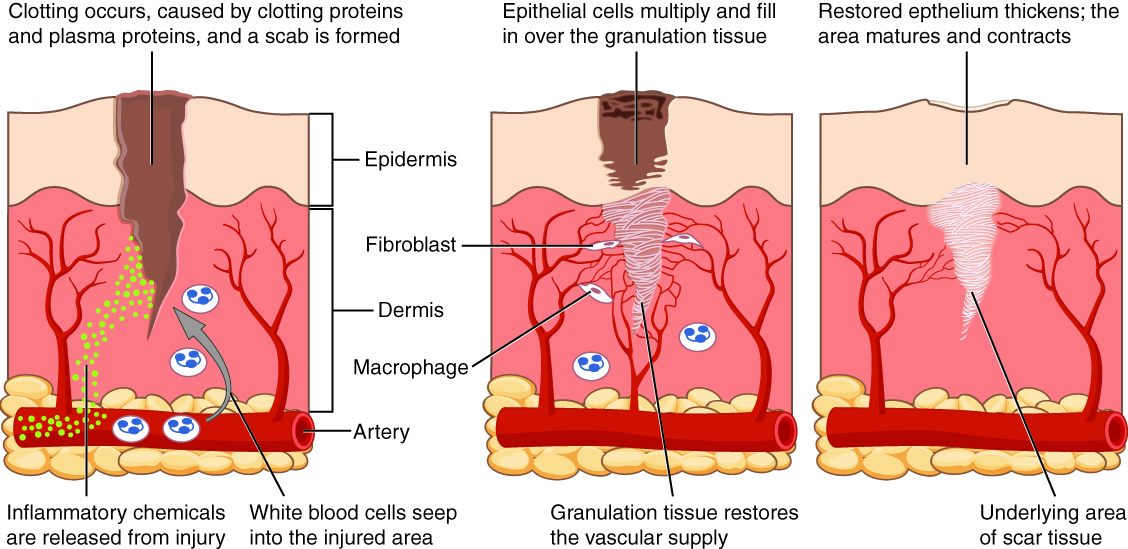
To illustrate the phases of wound healing, imagine that you accidentally cut your finger with a knife as you were slicing an apple for a snack. Immediately after the injury occurs, blood vessels constrict and clotting factors are activated. This is referred to as the hemostasis phase. Clotting factors are released to form clots and to stop the bleeding. Platelets release growth factors that alert various cells to start the repair process at the wound location. The hemostasis phase lasts up to 60 minutes, depending on the severity of the injury.[2],[3]
After the hemostasis phase, the inflammatory phase begins. Vasodilation occurs so that white blood cells in the bloodstream can move to the location of the wound and start cleaning the wound bed. The inflammatory process appears as edema (swelling), erythema (redness), and exudate. Exudate is fluid that oozes out of a wound and is commonly called pus or drainage.[4],[5]
The proliferative phase of wound healing begins within a few days after the injury and includes four important processes: epithelialization, angiogenesis, collagen formation, and contraction. Epithelialization refers to the development of new epidermis and granulation tissue. Granulation tissue is new connective tissue with new, fragile, thin-walled capillaries. Collagen is also formed to provide strength and integrity to the wound. At the end of the proliferation phase, the wound begins to contract in size.[6],[7]
Capillaries begin to develop within the wound 24 hours after injury during a process called angiogenesis. These capillaries bring more oxygen and nutrients to the wound for healing. When performing dressing changes, it is essential for the nurse to protect this granulation tissue and the associated new capillaries. Healthy granulation tissue appears pink due to the new capillary formation. It is moist, painless to the touch, and may appear “bumpy.” Conversely, unhealthy granulation tissue is dark red and painful. It bleeds easily with minimal contact and may be covered by shiny white or yellow fibrous tissue, referred to as biofilm, that must be removed because it impedes healing. Unhealthy granulation tissue is often caused by an infection, so wound cultures should be obtained when infection is suspected.[8]
During the maturation phase, collagen continues to be created to strengthen the wound. Collagen contributes strength to the wound to prevent it from reopening. A wound typically heals within 4-5 weeks and often leaves behind a scar. The scar tissue is initially firm, red, and slightly raised from the excess collagen deposition. Over time, the scar begins to soften, flatten, and become pale in about nine months.[9],[10]
Types of Wound Healing
There are three types of wound healing: primary intention, secondary intention, and tertiary intention. Healing by primary intention means that the wound is sutured, stapled, glued, or otherwise closed so the wound heals beneath the closure. This type of healing occurs with clean-edged lacerations or surgical incisions, and the closed edges are referred to as approximated. See Figure 10.11[11] for an image of a surgical wound healing by primary intention with approximated edges.

Secondary intention occurs when the edges of a wound cannot be approximated (brought together), so the wound heals by filling in from the bottom up with the production of granulation tissue. Examples of common wounds that heal by secondary intention are pressure injuries and skin tears. Wounds that heal by secondary infection are at higher risk for infection and must be protected from contamination. See Figure 10.12[12] for an image of a wound healing by secondary intention.
Tertiary intention refers to the healing of a wound that has had to remain open or has been reopened, often due to severe infection. The wound is typically closed at a later date when infection has resolved. Wounds that heal by secondary and tertiary intention have delayed healing times and increased scar tissue.

Types of Wounds
There are many common types of wounds that nurses care for, such as skin tears, venous ulcers, arterial ulcers, diabetic ulcers, and pressure injuries.
Wound Care
Wound care includes assessing and cleansing wounds, performing dressing changes, and implementing interventions to promote wound healing. Assessing wounds and implementing interventions to promote wound healing are further discussed in the “Applying the Nursing Process” section later in this chapter.
- “417 Tissue Repair.jpg” by OpenStax is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs & Manna and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs & Manna and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs & Manna and is licensed under CC BY 4.0 ↵
- McKay, M. (1990). The dermatologic history. In Walker, H. K., Hall, W. D., Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed.). https://www.ncbi.nlm.nih.gov/books/NBK207/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs & Manna and is licensed under CC BY 4.0 ↵
- “Ventriculoperitoneal shunt - surgical wound healing - belly - day 12.jpg” by Hansmuller is licensed under CC BY-SA 4.0 ↵
- “Atrophied skin.png” by sansea2 is licensed under CC BY-SA 3.0 ↵
Answer Key to Chapter 5 Learning Activities
1. Risk factors: hip fracture, morphine pain medication, diminished eyesight and hearing, ambulates with walker, weakness, experience of recent fall.
2. Morse Fall Risk Assessment Scoring:
- History of fall - 25
- Walker - 15
- Weak Gait -10
- Total: 50 - High Risk
3. Interventions to address risk factors:
- Provide adequate lighting and night-light
- Use of half rails
- Encourage rest
- Place articles within reach at bedside
- Use elevated toilet seat in bathroom
- Use assistive devices, glasses and hearing aids
- Obtain orthostatic blood pressures
- Wear shoes or slippers with non-skid soles
4. Potential response: "Mr. Moore, your safety is most important and we need to ensure you do not fall. If you have a bowel movement, we will clean it up. Moving forward, it may be helpful for us to have a commode chair closer to your bedside so we do not need to travel so far if urgency arises."
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 5 Learning Activities
1. Risk factors: hip fracture, morphine pain medication, diminished eyesight and hearing, ambulates with walker, weakness, experience of recent fall.
2. Morse Fall Risk Assessment Scoring:
- History of fall - 25
- Walker - 15
- Weak Gait -10
- Total: 50 - High Risk
3. Interventions to address risk factors:
- Provide adequate lighting and night-light
- Use of half rails
- Encourage rest
- Place articles within reach at bedside
- Use elevated toilet seat in bathroom
- Use assistive devices, glasses and hearing aids
- Obtain orthostatic blood pressures
- Wear shoes or slippers with non-skid soles
4. Potential response: "Mr. Moore, your safety is most important and we need to ensure you do not fall. If you have a bowel movement, we will clean it up. Moving forward, it may be helpful for us to have a commode chair closer to your bedside so we do not need to travel so far if urgency arises."
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 7 Learning Activities
- Answers to "Activity 1" will be individualized based on the assessment findings that are identified in the data collection with your student peer or simulated patient.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 7 Learning Activities
- Answers to "Activity 1" will be individualized based on the assessment findings that are identified in the data collection with your student peer or simulated patient.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 8 Learning Activities
- Potential interventions to improve breathing pattern and lung capacity include coughing and deep breathing, use of an incentive spirometer, use of an acapella flutter valve to mobilize secretions, increased fluids to thin secretions, frequent ambulation to mobilize secretions, etc.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 6 Learning Activities
Scenario A
1. In the immediate postoperative period, it is important to assess for signs of infection, electrolyte imbalances, confusion related to new medications, and hypoxia.
2. Table 1
| Dementia | Delirium | Depression | |
|---|---|---|---|
| Onset | Vague, insidious onset; symptoms progress slowly | Sudden onset over hours and days with fluctuations | Onset often rapid with identifiable trigger or life event such as bereavement |
| Symptoms | Symptoms may go unnoticed for years. May attempt to hide cognitive problems or may be unaware of them. Often disoriented to time, place, and person. Impaired short-term memory and information processing. Confusion is often worse in the evening (sundowning) | Often disoriented to time, place, and person. Impaired short-term memory loss and information processing. Confusion is often worse in the evening | Obvious at early stages and often worse in the morning. Can include subjective complaints of memory loss |
| Consciousness | Normal | Impaired attention/alertness | Normal |
| Mental State | Possibly labile mood. Consistently decreased cognitive performance | Emotional lability with anxiety, fear, depression, aggression. Variable cognitive performance | Distressed/unhappy. Variable cognitive performance |
| Delusions/Hallucinations | Common | Common | Rare |
| Psychomotor Disturbance | Psychomotor disturbance in later stages | Psychomotor disturbance present - hyperactive, purposeless, or apathetic | Slowed psychomotor status in severe depression |
Based upon the patient's sudden exacerbation of symptoms, she would most likely be exhibiting signs of delirium related to her recent surgery.
3. Interventions include the following:
- Control the environment. Make sure that the room is quiet and well-lit, have clocks or calendars in view, and encourage family members to visit.
- Administer prescribed medications, including those that control aggression or agitation and pain relievers if there is pain.
- Ensure the patient has their glasses, hearing aids, or other assistive devices for communication in place. Lack of assistive sensory devices can worsen delirium.
- Avoid sedatives. Sedatives can worsen delirium.
- Assign the same staff for patient care when possible.
Scenario B
1. Symptoms of moderate Alzheimer’s disease include the following:
- Require assistance with reminders to eat, wash, and use the restroom.
- Lack of recognition of family and friends.
- Behavioral symptoms such as wandering, getting lost, hallucinations, delusions, and repetitive behavior may occur.
- Patients living at home may engage in risky behavior, such as leaving the house in clothing inappropriate for weather conditions or leaving on the stove burners.
2. Additional assessments would include assessing for signs of physical discomfort, changes in the environment that may be contributing to the increased anxiety or confusion, and communication pattern.
3. Strategies for therapeutic response:
- Back off and ask permission before performing care tasks. Use calm, positive statements, slow down, add lighting, and provide reassurance. Offer guided choices between two options when possible. Focus on pleasant events and try to limit stimulation.
- Use effective language. When speaking, try phrases such as, “May I help you? Do you have time to help me? You're safe here. Everything is under control. I apologize. I'm sorry that you are upset. I know it's hard. I will stay with you until you feel better.”
- Listen to the person’s frustration. Find out what may be causing the agitation, and try to understand.
- Check yourself. Do not raise your voice, show alarm or offense, or corner, crowd, restrain, criticize, ignore, or argue with the person. Take care not to make sudden movements out of the person's view.
4. Medications may include the following:
- Donepezil (Aricept), approved to treat all stages of Alzheimer’s disease
- Galantamine (Razadyne), approved for mild-to-moderate stages
- Rivastigmine (Exelon), approved for mild-to-moderate stages
- Memantine (Namenda) and a combination of memantine and donepezil (Namzaric) are by approved the FDA for treatment of moderate to severe Alzheimer’s.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 9 Learning Activities
- Based upon Ms. Jamison's current vital signs and presenting condition, one would suspect the patient is septic. Her current vital signs reflect an elevated temperature > 100.4 and a tachycardic heart rate. Additionally, based upon the patient's history, one would suspect she has an unresolved urinary tract infection.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 8 Learning Activities
- Potential interventions to improve breathing pattern and lung capacity include coughing and deep breathing, use of an incentive spirometer, use of an acapella flutter valve to mobilize secretions, increased fluids to thin secretions, frequent ambulation to mobilize secretions, etc.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 9 Learning Activities
- Based upon Ms. Jamison's current vital signs and presenting condition, one would suspect the patient is septic. Her current vital signs reflect an elevated temperature > 100.4 and a tachycardic heart rate. Additionally, based upon the patient's history, one would suspect she has an unresolved urinary tract infection.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 6 Learning Activities
Scenario A
1. In the immediate postoperative period, it is important to assess for signs of infection, electrolyte imbalances, confusion related to new medications, and hypoxia.
2. Table 1
| Dementia | Delirium | Depression | |
|---|---|---|---|
| Onset | Vague, insidious onset; symptoms progress slowly | Sudden onset over hours and days with fluctuations | Onset often rapid with identifiable trigger or life event such as bereavement |
| Symptoms | Symptoms may go unnoticed for years. May attempt to hide cognitive problems or may be unaware of them. Often disoriented to time, place, and person. Impaired short-term memory and information processing. Confusion is often worse in the evening (sundowning) | Often disoriented to time, place, and person. Impaired short-term memory loss and information processing. Confusion is often worse in the evening | Obvious at early stages and often worse in the morning. Can include subjective complaints of memory loss |
| Consciousness | Normal | Impaired attention/alertness | Normal |
| Mental State | Possibly labile mood. Consistently decreased cognitive performance | Emotional lability with anxiety, fear, depression, aggression. Variable cognitive performance | Distressed/unhappy. Variable cognitive performance |
| Delusions/Hallucinations | Common | Common | Rare |
| Psychomotor Disturbance | Psychomotor disturbance in later stages | Psychomotor disturbance present - hyperactive, purposeless, or apathetic | Slowed psychomotor status in severe depression |
Based upon the patient's sudden exacerbation of symptoms, she would most likely be exhibiting signs of delirium related to her recent surgery.
3. Interventions include the following:
- Control the environment. Make sure that the room is quiet and well-lit, have clocks or calendars in view, and encourage family members to visit.
- Administer prescribed medications, including those that control aggression or agitation and pain relievers if there is pain.
- Ensure the patient has their glasses, hearing aids, or other assistive devices for communication in place. Lack of assistive sensory devices can worsen delirium.
- Avoid sedatives. Sedatives can worsen delirium.
- Assign the same staff for patient care when possible.
Scenario B
1. Symptoms of moderate Alzheimer’s disease include the following:
- Require assistance with reminders to eat, wash, and use the restroom.
- Lack of recognition of family and friends.
- Behavioral symptoms such as wandering, getting lost, hallucinations, delusions, and repetitive behavior may occur.
- Patients living at home may engage in risky behavior, such as leaving the house in clothing inappropriate for weather conditions or leaving on the stove burners.
2. Additional assessments would include assessing for signs of physical discomfort, changes in the environment that may be contributing to the increased anxiety or confusion, and communication pattern.
3. Strategies for therapeutic response:
- Back off and ask permission before performing care tasks. Use calm, positive statements, slow down, add lighting, and provide reassurance. Offer guided choices between two options when possible. Focus on pleasant events and try to limit stimulation.
- Use effective language. When speaking, try phrases such as, “May I help you? Do you have time to help me? You're safe here. Everything is under control. I apologize. I'm sorry that you are upset. I know it's hard. I will stay with you until you feel better.”
- Listen to the person’s frustration. Find out what may be causing the agitation, and try to understand.
- Check yourself. Do not raise your voice, show alarm or offense, or corner, crowd, restrain, criticize, ignore, or argue with the person. Take care not to make sudden movements out of the person's view.
4. Medications may include the following:
- Donepezil (Aricept), approved to treat all stages of Alzheimer’s disease
- Galantamine (Razadyne), approved for mild-to-moderate stages
- Rivastigmine (Exelon), approved for mild-to-moderate stages
- Memantine (Namenda) and a combination of memantine and donepezil (Namzaric) are by approved the FDA for treatment of moderate to severe Alzheimer’s.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 10 Learning Activities
- It would be helpful to assess the sacral area to identify the stage the pressure injury. It would also be helpful to assess Mr. Johns' albumin level to properly identify nutritional inadequacies and protein levels for wound healing.
- Individual factors that increase vulnerability to pressure injury development include weakness, diminished sensation (related to his stroke), diminished mobility, frequent incontinence, decreased nutritional intake, etc.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 12 Learning Activities
Scenario A
A nurse is caring for a patient who has been hospitalized after undergoing hip-replacement surgery. The patient complains of not sleeping well and feels very drowsy during the day.
1. The patient may be experiencing pain that is disrupting the sleep pattern. Additionally, the inpatient hospital settings may present unintended interruptions such as assessment and vital sign collection. Measures should be taken to create a quiet, therapeutic environment and minimize interruptions during sleeping hours.
2. The nurse should assess the patient’s pain level, general comfort, and self-reported feeling of restfulness upon awakening. The nurse should also carefully examine the patient’s rest pattern by asking questions regarding length of rest, period of wakefulness, and intervals with which these occur throughout the day.
3. The patient will have uninterrupted rest of six hours each night during their hospitalization.
4. The nurse should consider pain medication intervention and strategies to create a therapeutic and restful environment. This includes minimizing interruption overnight, clustering care and interventions, limiting noise or distractions, etc. The nurse should also consider if sleep aids are needed while being mindful of the impact of these medication aids in relation to fall risk. The nurse should also take measures to advocate for quiet periods for the patient.
5. The nurse would determine the effectiveness of interventions by monitoring the patient’s level of alertness throughout the daytime hours, self-reported level of energy, and ability to participate in therapy and care activities.
Scenario B
A nurse is assigned to work rotating shifts and develops difficulty sleeping.
1. Rotating shifts impact an individual’s sleep pattern because of the disruption to one’s circadian rhythm.
2. Symptoms of insomnia include lying awake for a long time before falling asleep, sleeping for only short periods, waking up too early in the morning and not being able to get back to sleep, waking up feeling unrested, difficulty focusing on tasks, irritability, anxiousness, and depression.
3. Healthy sleep habits include the following:
- Sleep in a cool, quiet place. Avoid artificial light from the TV or electronic devices, as this can disrupt your sleep-wake cycle.
- Go to sleep and wake up around the same times each day, even on the weekends. If you can, avoid night shifts, irregular schedules, or other things that may disrupt your sleep schedule.
- Avoid caffeine, nicotine, and alcohol close to bedtime.
- Get regular physical activity during the daytime (at least 5 to 6 hours before going to bed).
- Avoid daytime naps, especially in the afternoon.
- Eat meals on a regular schedule and avoid late-night dinners to maintain a regular sleep-wake cycle.
- Limit how much fluid you drink close to bedtime.
- Learn new ways to manage stress.
- Avoid certain over-the-counter and prescription medicines that can disrupt sleep (for example, some cold and allergy medicines).
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 11 Learning Activities
Patient Scenario Colon Cancer & Pain Management
1. What additional assessments (subjective and objective) will you perform on Joe?
Additional assessments include a full respiratory, abdominal, and pain assessment. It is important to include Joe’s subjective statements related to these systems, as well as observable findings. It would be important to collect information related to lung sounds, observed breathing effort, color of sputum, reports of shortness of breath, etc. Additionally, the patient should be assessed for guarding, grimace, self-report of pain, etc. The patient may not be getting out of bed and ambulating due to pain, but the lack of ambulation is causing additional problems for the patient. With the colon resection and lack of ambulation, it would also be important to determine the patient’s bowel function. Abdominal sounds, ability to pass flatus, last bowel movement, signs of nausea, etc., are all important for determining bowel motility.
2. List the top three priority nursing diagnoses for Joe.
Potential priority diagnoses for Joe might include the following:
- Ineffective Breathing Pattern
- Acute Pain
- Impaired Mobility
- Activity Intolerance
- Constipation
3. Joe states, “I don’t want to use morphine. I am afraid I will become addicted to it like my friend did after he came home from the war.” How will you respond to therapeutically address his concerns, yet also teach Joe about good pain management?
It would be important to dispel myths for the patient regarding pain management and addiction. Joe should receive education that the use of opioids is appropriate for the treatment of acute surgical pain in the short-term. He should receive instruction that by omitting the use of pain medications, his pain response has led to decreased mobility, which is causing respiratory complications for him.
4. What are common side effects of opioids and how will you plan to manage these side effects for Joe?
Common side effects of opioids are decreased respiratory rate, decreased bowel motility, increased lethargy, etc. Of significant concern for Joe is the potential impact of the opioid on his bowel function. The surgical intervention and lack of mobility have already placed him at risk for constipation. It will be important for the patient to resume a sufficient bowel regimen with adequate fluids, ambulation, stool softeners, high fiber foods, and laxatives if needed.
5. Emotional issues could also be affecting Joe’s perception of pain. What will you further physically assess and therapeutically address?
With Joe’s diagnosis of colon cancer, there can be many personal coping challenges that the patient is experiencing. It is important to encourage Joe to verbalize his feelings related to his diagnosis and understand what resources might best help facilitate his individual coping.
6. After providing patient education about morphine and the PCA pump, you check on Joe later in the day and notice he has had five injections and 15 attempts in the past hour. What further assessments will you perform?
It will be important to assess the insertion site where the pain medication is infusing to be certain that the tubing is not kinked and that the medication is actually reaching the patient. Additionally, Joe should receive education about use of the pump and guidelines regarding self-administration to ensure he understands the administration parameters appropriately. He should also have a thorough pain assessment completed, and the nurse should collect information to report to the prescribing physician regarding the use of medication and patient response.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 11 Learning Activities
Patient Scenario Colon Cancer & Pain Management
1. What additional assessments (subjective and objective) will you perform on Joe?
Additional assessments include a full respiratory, abdominal, and pain assessment. It is important to include Joe’s subjective statements related to these systems, as well as observable findings. It would be important to collect information related to lung sounds, observed breathing effort, color of sputum, reports of shortness of breath, etc. Additionally, the patient should be assessed for guarding, grimace, self-report of pain, etc. The patient may not be getting out of bed and ambulating due to pain, but the lack of ambulation is causing additional problems for the patient. With the colon resection and lack of ambulation, it would also be important to determine the patient’s bowel function. Abdominal sounds, ability to pass flatus, last bowel movement, signs of nausea, etc., are all important for determining bowel motility.
2. List the top three priority nursing diagnoses for Joe.
Potential priority diagnoses for Joe might include the following:
- Ineffective Breathing Pattern
- Acute Pain
- Impaired Mobility
- Activity Intolerance
- Constipation
3. Joe states, “I don’t want to use morphine. I am afraid I will become addicted to it like my friend did after he came home from the war.” How will you respond to therapeutically address his concerns, yet also teach Joe about good pain management?
It would be important to dispel myths for the patient regarding pain management and addiction. Joe should receive education that the use of opioids is appropriate for the treatment of acute surgical pain in the short-term. He should receive instruction that by omitting the use of pain medications, his pain response has led to decreased mobility, which is causing respiratory complications for him.
4. What are common side effects of opioids and how will you plan to manage these side effects for Joe?
Common side effects of opioids are decreased respiratory rate, decreased bowel motility, increased lethargy, etc. Of significant concern for Joe is the potential impact of the opioid on his bowel function. The surgical intervention and lack of mobility have already placed him at risk for constipation. It will be important for the patient to resume a sufficient bowel regimen with adequate fluids, ambulation, stool softeners, high fiber foods, and laxatives if needed.
5. Emotional issues could also be affecting Joe’s perception of pain. What will you further physically assess and therapeutically address?
With Joe’s diagnosis of colon cancer, there can be many personal coping challenges that the patient is experiencing. It is important to encourage Joe to verbalize his feelings related to his diagnosis and understand what resources might best help facilitate his individual coping.
6. After providing patient education about morphine and the PCA pump, you check on Joe later in the day and notice he has had five injections and 15 attempts in the past hour. What further assessments will you perform?
It will be important to assess the insertion site where the pain medication is infusing to be certain that the tubing is not kinked and that the medication is actually reaching the patient. Additionally, Joe should receive education about use of the pump and guidelines regarding self-administration to ensure he understands the administration parameters appropriately. He should also have a thorough pain assessment completed, and the nurse should collect information to report to the prescribing physician regarding the use of medication and patient response.
Answers to interactive elements are given within the interactive element.

