Scope of Practice
1.8 Quality and Evidence-Based Practice
The American Nursing Association (ANA), various professional nursing organizations, and federal agencies continually work to improve the quality of patient care. Nurses must also be individually dedicated to providing quality patient care based on current evidence-based practices.
Quality of Practice
One of the American Nurses Association (ANA) Standards of Professional Practice is “Quality of Practice.” This standard emphasizes that “nursing practice is safe, effective, efficient, equitable, timely, and person-centered.”[1] Quality is defined as, “The degree to which nursing services for healthcare consumers, families, groups, communities, and populations increase the likelihood of desirable outcomes and are consistent with evolving nursing knowledge.”[2] Every nurse is responsible for providing quality care to their patients by following the standards set forth by various organizations, as well as personally incorporating evidence-based practice. Quality is everyone’s responsibility and it takes the entire health care team to ensure that quality care is provided to each and every patient. For example, turning an immobile patient every two hours to prevent pressure injuries requires the dedication of many staff members throughout the day and night. Quality actions can also be formalized on a specific unit, such as the review of data related to patient falls with specific unit-based interventions formally put into place. This commitment to quality practice requires lifelong learning after you have completed your formal nursing education to remain current with new evidence-based practices.
Learning how to provide safe, quality nursing practice begins in nursing school. The Quality and Safety Education for Nurses (QSEN) project encourages future nurses to continuously improve the quality and safety of the health care systems in which they work. The vision of the QSEN project is to “inspire health care professionals to put quality and safety as core values to guide their work.”[3] Nurses and nursing students are expected to participate in quality improvement (QI) initiatives by identifying gaps where change is needed and implementing initiatives to resolve these gaps. Quality improvement is defined as the combined and unceasing efforts of everyone – health care professionals, patients and their families, researchers, payers, planners, and educators – to make the changes that will lead to optimal patient outcomes (health), improved system performance (care), and enhanced professional development (learning).[4] As a nursing student, you can immediately begin to contribute to improving the quality of nursing practice by participating in quality improvement initiatives.
Read more about the QSEN project.
Evidence-Based Practice in Nursing
Evidence-based practice is a component of ANA’s “Scholarly Inquiry” Standard of Professional Practice. Evidence-based practice is defined as, “A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the healthcare consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values.”[5]
Utilizing evidence-based practice means that nurses and nursing students provide patient care based on research studies and clinical expertise and do not just do something “because that’s the way we’ve always done it.” A simple example of nurses promoting evidence-based practice to help patients is using peppermint to relieve nausea. Throughout history, peppermint was used for an upset stomach and to relieve the feeling of nausea. This idea was frequently rejected in the medical field because there was no scientific evidence to support it. However, In 2016, Lynn Bayne and Helen Hawrylack, two nurse researchers, developed a peppermint inhaler for patients to use when they were feeling nauseated and found it was 93% effective in relieving nausea.[6]
Nursing students should implement evidence-based practice as they begin their nursing career by ensuring the resources they use to prepare for patient care are valid and credible. For this reason, hyperlinks to credible and reliable sources are provided throughout this textbook.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association ↵
- QSEN Institute. (n.d.). Project overview. http://qsen.org/about-qsen/project-overview/ ↵
- Batalden, P. B., & Davidoff, F. (2007). What is "quality improvement" and how can it transform healthcare? BMJ Quality & Safety, 16(1), 2–3. https://doi.org/10.1136/qshc.2006.022046 ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- ChristianaCare News. (2016, May 16). Nurse researchers develop peppermint inhaler to relieve post-op nausea. https://news.christianacare.org/2016/05/nurse-researchers-develop-peppermint-inhaler-to-relieve-post-op-nausea/ ↵
Patient Scenario
Mrs. Rosas is a 76-year-old patient admitted to the cardiology floor with an exacerbation of congestive heart failure. The patient’s primary language is Spanish, and she has a limited understanding of English. The patient’s daughter reports that the patient has been experiencing increased swelling in her ankles and increased shortness of breath over the last three weeks. Her daughter also reports that the patient has noted unexplained weight gain. During the admission assessment the nurse attempts to collect additional information related to current symptoms, diet, and history. The patient nods in response to questions and converses quietly in Spanish with her daughter.
Applying the Nursing Process
Assessment: The nurse notes that the patient does not respond to questions appropriately and is unable to converse in English. She defers to her daughter to provide interpretation of questions and relay information.
Based on the assessment information that has been gathered, the following nursing care plan is created for Mrs. Rosas.
Nursing Diagnosis: Impaired Verbal Communication related to cultural incongruence as evidenced by inability to speak the language of the caregiver.
Overall Goal: The patient will use effective communication techniques.
SMART Expected Outcome: Mrs. Rosas will utilize interpreter services in order to receive information and express needs throughout her hospitalization.
Planning and Implementing Nursing Interventions:
The nurse will provide patient with interpreter services in order to facilitate patient communication. In-person interpreter or language line telephone services will be utilized to ensure that the patient receives information about her care. The nurse will eliminate distractions such as the television, hallway noise, etc., to decrease sources of additional stimuli in the communication experience. The nurse will communicate directly with the patient, utilizing appropriate eye contact, and nonverbal cues to enhance the communication experience.
Sample Documentation
Mrs. Rosas has impaired verbal communication due to limited English proficiency. She requires education regarding cardiac diet, fluid restriction, and exacerbation warning signs. Interpreter services have been utilized to ensure that communication and education needs are appropriate. Mrs. Rosas communicates freely through the interpreter and acknowledges understanding of the education that has been provided.
Evaluation
During the patient’s hospitalization, Mrs. Rosas engages with staff through the use of interpreter services and actively participates in her own care.
After establishing a culturally sensitive environment and performing a cultural assessment, nurses and nursing students can continue to promote culturally responsive care. Culturally responsive care includes creating a culturally safe environment, using cultural negotiation, and considering the impact of culture on patients’ time orientation, space orientation, eye contact, and food choices.
Culturally Safe Environment
A primary responsibility of the nurse is to ensure the environment is culturally safe for the patient. A culturally safe environment is a safe space for patients to interact with the nurse, without judgment or discrimination, where the patient is free to express their cultural beliefs, values, and identity. This responsibility belongs to both the individual nurse and also to the larger health care organization.
Cultural Negotiation
Many aspects of nursing care are influenced by the patient’s cultural beliefs, as well as the beliefs of the health care culture. For example, the health care culture in the United States places great importance on punctuality for medical appointments, yet a patient may belong to a culture that views “being on time” as relative. In some cultures, time is determined simply by whether it is day or night or time to wake up, eat, or sleep. Making allowances or accommodations for these aspects of a patient’s culture is instrumental in fostering the nurse-patient relationship. This accommodation is referred to as cultural negotiation. See Figure 3.6[1] for an image illustrating cultural negotiation. During cultural negotiation, both the patient and nurse seek a mutually acceptable way to deal with competing interests of nursing care, prescribed medical care, and the patient’s cultural needs. Cultural negotiation is reciprocal and collaborative. When a patient’s cultural needs do not significantly or adversely affect their treatment plan, their cultural needs should be accommodated when feasible.
As an example, think about the previous example of a patient for whom a fixed schedule is at odds with their cultural views. Instead of teaching the patient to take a daily medication at a scheduled time, the nurse could explain that the patient should take the medication every day when he gets up. Another example of cultural negotiation is illustrated by a scenario in which the nurse is preparing a patient for a surgical procedure. As the nurse goes over the preoperative checklist, the nurse asks the patient to remove her head covering (hijab). The nurse is aware that personal items should be removed before surgery; however, the patient wishes to keep on the hijab. As an act of cultural negotiation and respect for the patient’s cultural beliefs, the nurse makes arrangements with the surgical team to keep the patient’s hijab in place for the surgical procedure and covering the patient’s hijab with a surgical cap.

Decision-Making
Health care culture in the United States mirrors cultural norms of the country, with an emphasis on individuality, personal freedom, and self-determination. This perspective may conflict with a patient whose cultural background values group decision-making and decisions made to benefit the group, not necessarily the individual. As an example, in the 2019 film The Farewell, a Chinese-American family decides to not tell the family matriarch she is dying of cancer and only has a few months left to live. The family keeps this secret from the woman in the belief that the family should bear the emotional burden of this knowledge, which is a collectivistic viewpoint in contrast to American individualistic viewpoint.
Space Orientation
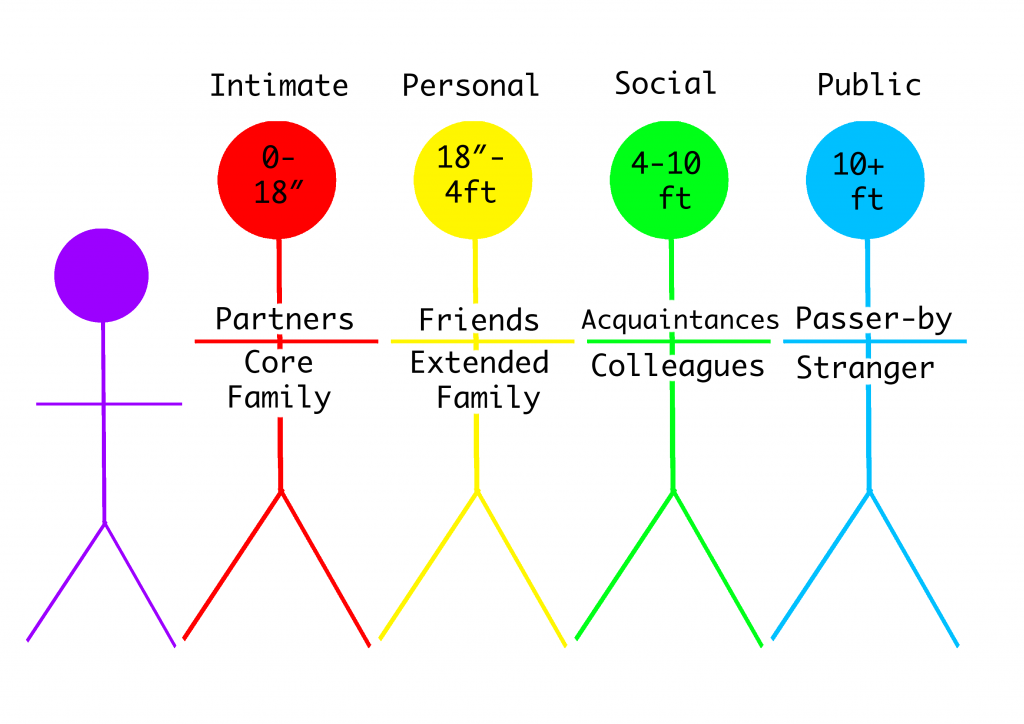
The amount of space that a person surrounds themselves with to feel comfortable is influenced by culture. (Read more about space orientation in the "Communication" chapter.) See Figure 3.7[2] for an image illustrating space orientation. For example, for some people, it would feel awkward to stand four inches away from another person while holding a social conversation, but for others a small personal space is expected when conversing with another.[3]There are times when a nurse must enter a patient’s intimate or personal space, which can cause emotional distress for some patients. The nurse should always ask for permission before entering a patient’s personal space and explain why and what is about to happen.
Patients may also be concerned about their modesty or being exposed. A patient may deal with the violation of their space by removing themselves from the situation, pulling away, or closing their eyes. The nurse should recognize these cues for what they are, an expression of cultural preference, and allow the patient to assume a position or distance that is comfortable for them.
Similar to cultural influences on personal space, touch is also culturally determined. This has implications for nurses because it may be inappropriate for a male nurse to provide care for a female patient and vice versa. In some cultures, it is also considered rude to touch a person’s head without permission.
Eye Contact
Eye contact is also a culturally mediated behavior. See Figure 3.8[4] for an image of eye contact. In the United States, direct eye contact is valued when communicating with others, but in some cultures, direct eye contact is interpreted as being rude or bold. Rather than making direct eye contact, a patient may avert their eyes or look down at the floor to show deference and respect to the person who is speaking. The nurse should notice these cultural cues from the patient and mirror the patient’s behaviors when possible.
Food Choices
Culture plays a meaningful role in the dietary practices and food choices of many people. Food is used to celebrate life events and holidays. Most cultures have staple foods, such as bread, pasta, or rice and particular ways of preparing foods. See Figure 3.9[5] for an image of various food choices. Special foods are prepared to heal and to cure or to demonstrate kinship, caring, and love. For example, in the United States, chicken noodle soup is often prepared and provided to family members who are ill.
Conversely, certain foods and beverages (such as meat and alcohol) are forbidden in some cultures. Nurses should accommodate or negotiate dietary requests of their patients, knowing that food holds such an important meaning to many people.

Summary
In summary, there are several steps in the journey of becoming a culturally competent nurse with cultural humility who provides culturally responsive care to patients. As you continue in your journey of developing cultural competency, keep the summarized points in the following box in mind.
Summary of Developing Cultural Competency
- Cultural competence is an ongoing process for nurses and takes dedication, time, and practice to develop.
- Pursuing the goal of cultural competence in nursing and other health care disciplines is a key strategy in reducing health care disparities.
- Culturally competent nurses recognize that culture functions as a source of values and comfort for patients, their families, and communities.
- Culturally competent nurses intentionally provide patient-centered care with sensitivity and respect for culturally diverse populations.
- Misunderstandings, prejudices, and biases on the part of the health care provider interfere with the patient’s health outcomes.
- Culturally competent nurses negotiate care with a patient so that is congruent with the patient’s cultural beliefs and values.
- Nurses should examine their own biases, ethnocentric views, and prejudices so as not to interfere with the patient’s care.
- Nurses who respect and understand the cultural values and beliefs of their patients are more likely to develop positive, trusting relationships with their patients.

