Scope of Practice
1.2 Regulations & Standards
Standards for nursing care are set by several organizations, including the American Nurses Association (ANA), your state’s Nurse Practice Act, agency policies and procedures, federal regulators, and other professional nursing organizations. These standards assure safe, competent care is provided to the public.
ANA Scope and Standards of Practice
The American Nurses Association (ANA) publishes two resources that set standards and guide professional nursing practice in the United States: The Code of Ethics for Nurses and Nursing: Scope and Standards of Practice. The Code of Ethics for Nurses establishes an ethical framework for nursing practice across all roles, levels, and settings. It is discussed in greater detail in the “Legal Considerations and Ethics” subsection of this chapter. The Nursing: Scope and Standards of Practice describes a professional nurse’s scope of practice and defines the who, what, where, when, why, and how of nursing. It also sets 18 standards of professional practice that all registered nurses are expected to perform competently. [1]
The “who” of nursing practice are the nurses who have been educated, titled, and maintain active licensure to practice nursing. The “what” of nursing is the recently revised definition of nursing: “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in recognition of the connection of all humanity.”[2] Simply put, nurses treat human responses to health problems and life processes and advocate for the care of others.
Nursing practice occurs “when” there is a need for nursing knowledge, wisdom, caring, leadership, practice, or education, anytime, anywhere. Nursing practice occurs in any environment “where” there is a health care consumer in need of care, information, or advocacy. The “why” of nursing practice is described as nursing’s response to the changing needs of society to achieve positive health care consumer outcomes in keeping with nursing’s social contract and obligation to society. The “how” of nursing practice is defined as the ways, means, methods, and manners that nurses use to practice professionally.[3] The “how” of nursing is further defined by the standards of practice set by the ANA. There are two sets of standards, the Standards of Professional Nursing Practice and the Standards of Professional Performance.
The Standards of Professional Nursing Practice are “authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.”[4] These standards define a competent level of nursing practice based on the critical thinking model known as the nursing process. The nursing process includes the components of assessment, diagnosis, outcomes identification, planning, implementation, and evaluation.[5] Each of these standards is further discussed in the “Nursing Process” chapter of this book.
The Standards of Professional Performance are 12 additional standards that describe a nurse’s professional behavior, including activities related to ethics, advocacy, respectful and equitable practice, communication, collaboration, leadership, education, scholarly inquiry, quality of practice, professional practice evaluation, resource stewardship, and environmental health. All registered nurses are expected to engage in these professional role activities based on their level of education, position, and role. Registered nurses are accountable for their professional behaviors to themselves, health care consumers, peers, and ultimately to society. [6] The 2021 Standards of Professional Performance are as follows:
- Ethics. The registered nurse integrates ethics in all aspects of practice.
- Advocacy. The registered nurse demonstrates advocacy in all roles and settings.
- Respectful and Equitable Practice. The registered nurse practices with cultural humility and inclusiveness.
- Communication. The registered nurse communicates effectively in all areas of professional practice.
- Collaboration. The registered nurse collaborates with the health care consumer and other key stakeholders.
- Leadership. The registered nurse leads within the profession and practice setting.
- Education. The registered nurse seeks knowledge and competence that reflects current nursing practice and promotes futuristic thinking.
- Scholarly Inquiry. The registered nurse integrates scholarship, evidence, and research findings into practice.
- Quality of Practice. The registered nurse contributes to quality nursing practice.
- Professional Practice Evaluation. The registered nurse evaluates one’s own and others’ nursing practice.
- Resource Stewardship. The registered nurse utilizes appropriate resources to plan, provide, and sustain evidence-based nursing services that are safe, effective, financially responsible, and judiciously used.
- Environmental Health. The registered nurse practices in a manner that advances environmental safety and health.[7]
Years ago, nurses were required to recite the Nightingale pledge to publicly confirm their commitment to maintain the profession’s high ethical and moral values: “I will do all in my power to maintain and elevate the standard of my profession and will hold in confidence all personal matters committed to my keeping and family affairs coming to my knowledge in the practice of my calling, with loyalty will I endeavor to aid the physician in his work, and devote myself to the welfare of those committed to my care.” Although some of the words are outdated, the meaning is clear: Nursing is a calling, not just a job; to answer that call, you must be dedicated to serve your community according to the ANA standards of care and code of ethics.[8]
Nurse Practice Act
In addition to the professional standards of practice and professional performance set by the American Nurses Association, nurses must legally follow regulations set by the Nurse Practice Act and enforced by the Board of Nursing in the state where they are employed. The Board of Nursing is the state-specific licensing and regulatory body that sets standards for safe nursing care and issues nursing licenses to qualified candidates, based on the Nurse Practice Act enacted by that state’s legislature. The Nurse Practice Act establishes regulations for nursing practice within that state and defines the scope of nursing practice. If nurses do not follow the standards and scope of practice set forth by the Nurse Practice Act, they can have their nursing license revoked by the Board of Nursing.
To read more about the the Wisconsin Board of Nursing, Standards of Practice, and Rules of Conduct, use the hyperlinked PDFs provided below.[9]
Read more details about the Wisconsin Administrative Code and the Board of Nursing.
Read about Wisconsin Standards of Practice for Nurses in Chapter N 6.
Read about Wisconsin Rules of Conduct in Chapter N 7.
Nursing students must understand their scope of practice outlined in their state’s Nurse Practice Act. Nursing students are legally accountable for the quality of care they provide to patients just as nurses are accountable. Students are expected to recognize the limits of their knowledge and experience and appropriately alert individuals in authority regarding situations that are beyond their competency. A violation of the standards of practice constitutes unprofessional conduct and can result in the Board of Nursing denying a license to a nursing graduate.
Employer Policies, Procedures, and Protocols
In addition to professional nursing standards set by the American Nurses Association and the state Nurse Practice Act where they work, nurses and nursing students must also practice according to agency policies, procedures, and protocols. For example, hospitals often set a policy that requires a thorough skin assessment must be completed and documented daily on every patient. If a nurse did not follow this policy and a patient developed a pressure injury, the nurse could be held liable. In addition, every agency has their own set of procedures and protocols that a nurse and nursing student must follow. For example, each agency has specific procedural steps for performing nursing skills, such as inserting urinary catheters. A protocol is defined by the Wisconsin Nurse Practice Act as a “precise and detailed written plan for a regimen of therapy.” For example, agencies typically have a hypoglycemia protocol that nurses automatically implement when a patient’s blood sugar falls below a specific number. The hypoglycemia protocol includes actions such as providing orange juice and rechecking the blood sugar. These agency-specific policies, procedures, and protocols supersede the information taught in nursing school, and nurses and nursing students can be held legally liable if they don’t follow them. Therefore, it is vital for nurses and nursing students to always review and follow current agency-specific procedures, policies, and protocols when providing patient care.
Nurses and nursing students must continue to follow their scope of practice as defined by the Nurse Practice Act in the state they are practicing when following agency policies, procedures, and protocols. Situations have occurred when a nurse or nursing student was asked by an agency to do something outside their defined scope of practice that impaired their nursing license. It is always up to you to protect your nursing license and follow the state’s Nurse Practice Act when providing patient care.
Federal Regulations
In addition to nursing scope of practice and standards being defined by the American Nurses Association, state Nurse Practice Acts, and employer policies, procedures, and protocols, nursing practice is also influenced by federal regulations enacted by agencies such as the Joint Commission and the Centers for Medicare and Medicaid.
The Joint Commission
The Joint Commission is a national organization that accredits and certifies over 20,000 health care organizations in the United States. The mission of The Joint Commission (TJC) is to continuously improve health care for the public by inspiring health care organizations to excel in providing safe and effective care of the highest quality and value.[10] The Joint Commission sets standards for providing safe, high-quality health care.
National Patient Safety Goals
The Joint Commission establishes annual National Patient Safety Goals for various types of agencies based on data regarding current national safety concerns.[11] For example, National Patient Safety Goals for hospitals include the following:
- Identify Patients Correctly
- Improve Staff Communication
- Use Medicines Safely
- Use Alarms Safely
- Prevent Infection
- Identify Patient Safety Risks
- Prevent Mistakes in Surgery
Nurses, nursing students, and other staff members are expected to incorporate actions related to these safety goals into their daily patient care. For example, SBAR (Situation, Background, Assessment, and Recommendation) handoff reporting techniques, bar code scanning equipment, and perioperative team “time-outs” prior to surgery are examples of actions incorporated at agencies based on National Patient Safety Goals. Nursing programs also use National Patient Safety Goals to guide their curriculum and clinical practice expectations. National Patient Safety Goals are further discussed in the “Safety” chapter of this book.
Use the hyperlinks provided below to read more about The Joint Commission and National Patient Safety Goals.
Joint Commission Center for Transforming Healthcare
The Joint Commission Center for Transforming Healthcare was developed in 2008 to help agencies develop effective solutions for critical safety problems with a goal to ultimately achieve zero harm to patients. Some of the projects the Center has developed include improved hand hygiene, effective handoff communications, and safe and effective use of insulin. The Center has also been instrumental in creating a focus on a safety culture in health care organizations. A safety culture empowers nurses, nursing students, and other staff members to speak up about their concerns about patient risks and to report errors and near misses, all of which drive improvement in patient care and reduce the incidences of patient harm.[12] Many health care agencies have implemented a safety culture in their workplace and successfully reduced incidences of patient harm. An example of a safety culture action is a nurse or nursing student creating an incident report when an error occurs when administering medication. The incident report is used by the agency to investigate system factors that contribute to errors. To read more about creating a safety culture, use the hyperlink provided below.
Read more about Creating a Safety Culture.
Centers for Medicare & Medicaid Services
The Centers for Medicare & Medicaid Services (CMS) is another federal agency that establishes regulations that affect nursing care. CMS is a part of the U.S. Department of Health and Human Services (HHS) that administers the Medicare program and works in partnership with state governments to administer Medicaid. The CMS establishes and enforces regulations to protect patient safety in hospitals that receive Medicare and Medicaid funding. For example, one CMS regulation states that a hospital’s policies and procedures must require confirmation of specific information before medication is administered to patients. This CMS regulation is often referred to as “checking the rights of medication administration.” You can read more information about checking the rights of medication administration in the “Administration of Enteral Medications” chapter of the Open RN Nursing Skills textbook.[13]
CMS also enforces quality standards in health care organizations that receive Medicare and Medicaid funding. These organizations are reimbursed based on the quality of their patient outcomes. For example, organizations with high rates of healthcare-associated infections (HAI) receive less reimbursement for services they provide. As a result, many agencies have reexamined their policies, procedures, and protocols to promote optimal patient outcomes and maximum reimbursement.
Now that we have discussed various agencies that affect a nurse’s scope and standards of practice, let’s review various types of health care settings where nurses work and members of the health care team.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Bostain, L. (2020, June 25). Nursing professionalism begins with you. American Nurse. https://www.myamericannurse.com/nursing-professionalism-begins-with-you/ ↵
- Wisconsin Administrative Code. (2018). Chapter N 6 standards of practice for registered nurses and licensed practical nurses. https://docs.legis.wisconsin.gov/code/admin_code/n/6.pdf ↵
- The Joint Commission. (n.d.). https://www.jointcommission.org/ ↵
- The Joint Commission. (n.d.). National patient safety goals. https://www.jointcommission.org/standards/national-patient-safety-goals/ ↵
- Joint Commission Center for Transforming Healthcare. (n.d.). Creating a safety culture. https://www.centerfortransforminghealthcare.org/why-work-with-us/video-resources/creating-a-safety-culture ↵
- This work is a derivative of Nursing Skills by Open RN and is licensed under CC BY 4.0 ↵
Professional communication with other members of the health care team is an important component of every nurse’s job. See Figure 2.8[1] for an image illustrating communication between health care team members. Common types of professional interactions include reports to health care team members, handoff reports, and transfer reports.

Reports to Health Care Team Members
Nurses routinely report information to other health care team members, as well as urgently contact health care providers to report changes in patient status.
Standardized methods of communication have been developed to ensure that information is exchanged between health care team members in a structured, concise, and accurate manner to ensure safe patient care. One common format used by health care team members to exchange patient information is ISBARR, a mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back.
-
- Introduction: Introduce your name, role, and the agency from which you are calling.
- Situation: Provide the patient’s name and location, why you are calling, recent vital signs, and the status of the patient.
- Background: Provide pertinent background information about the patient such as admitting medical diagnoses, code status, recent relevant lab or diagnostic results, and allergies.
- Assessment: Share abnormal assessment findings and your evaluation of the current patient situation.
- Request/Recommendations: State what you would like the provider to do, such as reassess the patient, order a lab/diagnostic test, prescribe/change medication, etc.
- Repeat back: If you are receiving new orders from a provider, repeat them to confirm accuracy. Be sure to document communication with the provider in the patient’s chart.
Read an example of an ISBARR report in the following box. A hyperlink is provided to a printable ISBARR reference card.
Sample ISBARR Report From a Nurse to a Health Care Provider
I: “Hello Dr. Smith, this is Jane White, RN from the Med Surg unit.”
S: “I am calling to tell you about Ms. White in Room 210, who is experiencing an increase in pain, as well as redness at her incision site. Her recent vital signs were BP 160/95, heart rate 90, respiratory rate 22, O2 sat 96%, and temperature 38 degrees Celsius. She is stable but her pain is worsening.”
B: “Ms. White is a 65-year-old female, admitted yesterday post hip surgical replacement. She has been rating her pain at 3 or 4 out of 10 since surgery with her scheduled medication, but now she is rating the pain as a 7, with no relief from her scheduled medication of Vicodin 5/325 mg administered an hour ago. She is scheduled for physical therapy later this morning and is stating she won’t be able to participate because of the pain this morning.”
A: “I just assessed the surgical site and her dressing was clean, dry, and intact, but there is 4 cm redness surrounding the incision, and it is warm and tender to the touch. There is moderate serosanguinous drainage. Otherwise, her lungs are clear and her heart rate is regular.”
R: “I am calling to request an order for a CBC and increased dose of pain medication.”
R: “I am repeating back the order to confirm that you are ordering a STAT CBC and an increase of her Vicodin to 10/325 mg.”
View or print an ISBARR reference card
.
Handoff Reports
Handoff reports are defined by The Joint Commission as “a transfer and acceptance of patient care responsibility achieved through effective communication. It is a real-time process of passing patient specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the patient’s care.”[2] In 2017, The Joint Commission issued a sentinel alert about inadequate handoff communication that has resulted in patient harm such as wrong-site surgeries, delays in treatment, falls, and medication errors. Strategies for improving handoff communication have been implemented at agencies across the country.
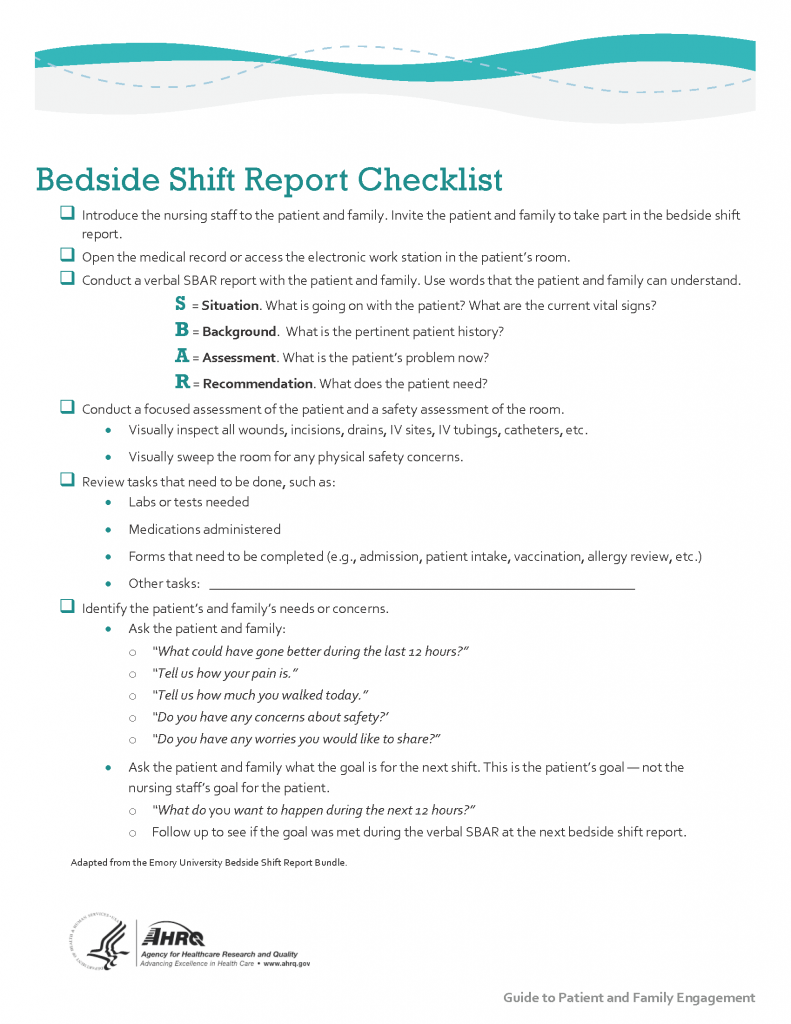
Although many types of nursing shift-to-shift handoff reports have been used over the years, evidence strongly supports that bedside handoff reports increase patient safety, as well as patient and nurse satisfaction, by effectively communicating current, accurate patient information in real time.[3] See Figure 2.9[4] for an image illustrating two nurses participating in a handoff report. Bedside reports typically occur in hospitals and include the patient, along with the off-going and the oncoming nurses in a face-to-face handoff report conducted at the patient's bedside. HIPAA rules must be kept in mind if visitors are present or the room is not a private room. Family members may be included with the patient’s permission. See a sample checklist for a bedside handoff report from the Agency for Healthcare Research and Quality in Figure 2.10.[5] Although a bedside handoff report is similar to an ISBARR report, it contains additional information to ensure continuity of care across nursing shifts. For example, the “assessment” portion of the bedside handoff report includes detailed pertinent data the oncoming nurse needs to know, such as current head-to-toe assessment findings to establish a baseline; information about equipment such as IVs, catheters, and drainage tubes; and recent changes in medications, lab results, diagnostic tests, and treatments.
![]"618721604-huge" by Rido is used under license from Shutterstock.com. Image showing two nurses discussing a chart both are holding](https://nicoletcollege.pressbooks.pub/app/uploads/sites/55/2022/04/618721604-huge-scaled-1.jpg)
View Sample Information to Include in a Shift Report.
View a video on creating shift reports.[6]
Transfer Reports
Transfer reports are provided by nurses when transferring a patient to another unit or to another agency. Transfer reports contain similar information as bedside handoff reports, but are even more detailed when the patient is being transferred to another agency. Checklists are often provided by agencies to ensure accurate, complete information is shared.
Patient Scenario
Mr. Hernandez is a 47-year-old patient admitted to the neurological trauma floor as the result of a motor vehicle accident two days ago. The patient sustained significant facial trauma in the accident and his jaw is wired shut. His left eye is currently swollen, and he had significant bruising to the left side of his face. The nurse completes a visual assessment and notes that the patient has normal extraocular movement, peripheral vision, and pupillary constriction bilaterally. Additional assessment reveals that Mr. Hernandez also sustained a fracture of the left arm and wrist during the accident. His left arm is currently in a cast and sling. He has normal movement and sensation with his right hand. Mrs. Hernandez is present at the patient’s bedside and has provided additional information about the patient. She reports that Mr. Hernandez’s primary language is Spanish but that he understands English well. He has a bachelor’s degree in accounting and owns his own accounting firm. He has a history of elevated blood pressure, but is otherwise healthy.
The nurse notes that the patient’s jaw is wired and he is unable to offer a verbal response. He does understand English well, has appropriate visual acuity, and is able to move his right hand and arm.
Based on the assessment information that has been gathered, the nurse plans several actions to enhance communication. Adaptive communication devices such as communication boards, symbol cards, or electronic messaging systems will be provided. The nurse will eliminate distractions such as television and hallway noise to decrease sources of additional stimuli in the communication experience.
Sample Documentation
Mr. Hernandez has impaired verbal communication due to facial fracture and inability to enunciate words around his wired jaw. He understands both verbal and written communication. Mr. Hernandez has left sided facial swelling, but no visual impairment. He has a left arm fracture but is able to move and write with his right hand. The patient is supplied with communication cards and marker board. He responds appropriately with written communication and is able to signal his needs.
Patient Scenario
Mr. Hernandez is a 47-year-old patient admitted to the neurological trauma floor as the result of a motor vehicle accident two days ago. The patient sustained significant facial trauma in the accident and his jaw is wired shut. His left eye is currently swollen, and he had significant bruising to the left side of his face. The nurse completes a visual assessment and notes that the patient has normal extraocular movement, peripheral vision, and pupillary constriction bilaterally. Additional assessment reveals that Mr. Hernandez also sustained a fracture of the left arm and wrist during the accident. His left arm is currently in a cast and sling. He has normal movement and sensation with his right hand. Mrs. Hernandez is present at the patient’s bedside and has provided additional information about the patient. She reports that Mr. Hernandez’s primary language is Spanish but that he understands English well. He has a bachelor’s degree in accounting and owns his own accounting firm. He has a history of elevated blood pressure, but is otherwise healthy.
The nurse notes that the patient’s jaw is wired and he is unable to offer a verbal response. He does understand English well, has appropriate visual acuity, and is able to move his right hand and arm.
Based on the assessment information that has been gathered, the nurse plans several actions to enhance communication. Adaptive communication devices such as communication boards, symbol cards, or electronic messaging systems will be provided. The nurse will eliminate distractions such as television and hallway noise to decrease sources of additional stimuli in the communication experience.
Sample Documentation
Mr. Hernandez has impaired verbal communication due to facial fracture and inability to enunciate words around his wired jaw. He understands both verbal and written communication. Mr. Hernandez has left sided facial swelling, but no visual impairment. He has a left arm fracture but is able to move and write with his right hand. The patient is supplied with communication cards and marker board. He responds appropriately with written communication and is able to signal his needs.
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Practice what you have learned in this chapter by completing these learning activities. When accessing the online activities that contain videos, it is best to use Google Chrome or Firefox browsers.
1. To test understanding of these terms, try an online quiz:
Therapeutic Communication Techniques vs. Non-therapeutic Communication Techniques Quizlet
2. Consider the following scenario and describe actions that you might take to facilitate the patient communication experience.
You are caring for Mr. Curtis, an 87-year-old patient newly admitted to the medical surgical floor with a hip fracture. You are preparing to complete his admission history and need to collect relevant health information and complete a physical exam. You approach the room, knock at the door, complete hand hygiene, and enter. Upon entry, you see Mr. Curtis is in bed surrounded by multiple family members. The television is on in the background and you also note the sound of meal trays being delivered in the hallway.
Based on the described scenario, what actions might be implemented to aid in your communication with Mr. Curtis?
Aphasia: A communication disorder that results from damage to portions of the brain that are responsible for language.
Assertive communication: A way to convey information that describes the facts, the sender’s feelings, and explanations without disrespecting the receiver’s feelings. This communication is often described as using “I” messages: “I feel…,” “I understand…,” or “Help me to understand…”
Bedside nurse handoff report: A handoff report in hospitals that involves patients, their family members, and both the off-going and the incoming nurses. The report is performed face to face and conducted at the patient's bedside.
Broca's aphasia: A type of aphasia where patients understand speech and know what they want to say, but frequently speak in short phrases that are produced with great effort. People with Broca's aphasia typically understand the speech of others fairly well. Because of this, they are often aware of their difficulties and can become easily frustrated.
Charting by exception: A type of documentation where a list of “normal findings” is provided and nurses document assessment findings by confirming normal findings and writing brief documentation notes for any abnormal findings.
DAR: A type of documentation often used in combination with charting by exception. DAR stands for Data, Action, and Response. Focused DAR notes are brief, and each note is focused on one patient problem for efficiency in documenting, as well as for reading.
Electronic Health Record (EHR): A digital version of a patient’s paper chart. EHRs are real-time, patient-centered records that make information available instantly and securely to authorized users.
Global aphasia: A type of aphasia that results from damage to extensive portions of the language areas of the brain. Individuals with global aphasia have severe communication difficulties and may be extremely limited in their ability to speak or comprehend language. They may be unable to say even a few words or may repeat the same words or phrases over and over again. They may have trouble understanding even simple words and sentences.
Handoff report: A process of exchanging vital patient information, responsibility, and accountability between the off-going and incoming nurses in an effort to ensure safe continuity of care and the delivery of best clinical practices.
ISBARR: A mnemonic for the format of professional communication among health care team members that includes Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back.
Minimum Data Set (MDS): A federally mandated assessment tool used in skilled nursing facilities to track a patient’s goal achievement, as well as to coordinate the efforts of the health care team to optimize the resident’s quality of care and quality of life.
Narrative note: A type of documentation that chronicles all of the patient’s assessment findings and nursing activities that occurred throughout the shift.
Nontherapeutic responses: Responses to patients that block communication, expression of emotion, or problem-solving.
Progressive relaxation: Types of relaxation techniques that focus on reducing muscle tension and using mental imagery to induce calmness.
Relaxation breathing: A breathing technique used to reduce anxiety and control the stress response.
SOAPIE: A mnemonic for a type of documentation that is organized by six categories: Subjective, Objective, Assessment, Plan, Interventions, and Evaluation.
Therapeutic communication: The purposeful, interpersonal information transmitting process through words and behaviors based on both parties’ knowledge, attitudes, and skills, which leads to patient understanding and participation.
Therapeutic communication techniques: Techniques that encourage patients to explore feelings, problem solve, and cope with responses to medical conditions and life events.
Verbal communication: Exchange of information using words understood by the receiver.
Learning Objectives
- Reflect upon personal and cultural values, beliefs, biases, and heritage[7]
- Embrace diversity, equity, inclusivity, health promotion, and health care for individuals of diverse geographic, cultural, ethnic, racial, gender, and spiritual backgrounds across the life span[8]
- Demonstrate respect, equity, and empathy in actions and interactions with all health care consumers[9]
- Participate in life-long learning to understand cultural preferences, worldviews, choices, and decision-making processes of diverse patients[10]
- Protect patient dignity
- Demonstrate principles of patient-centered care and cultural humility
- Make adaptations to patient care to reduce health disparities
- Adhere to the Patient's Bill of Rights
- Identify strategies to advocate for patients
- Use evidence-based practices
No matter who we are or where we come from, every person belongs to a culture. The impact of culture on a person’s health is profound because it affects many health beliefs, such as perceived causes of illness, ways to prevent illness, and acceptance of medical treatments. Culturally responsive care integrates these cultural beliefs into an individual's health care. Culturally responsive care is intentional and promotes trust and rapport with patients. At its heart, culturally responsive care is patient-centered care. The American Nurses Association (ANA) states, "The art of nursing is demonstrated by unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care."[11]
Nurses provide holistic care when incorporating their patients’ physical, mental, spiritual, cultural, and social needs into their health care (referred to as holism). As a nursing student, you are undertaking a journey of developing cultural competency with an attitude of cultural humility as you learn how to provide holistic care to your patients. Cultural competency is a lifelong process of applying evidence-based nursing in agreement with the cultural values, beliefs, worldview, and practices of patients to produce improved patient outcomes.[12],[13],[14] Cultural humility is defined by the American Nurses Association as, "A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot know everything about other cultures, and approach learning about other cultures as a life-long goal and process.[15] The bottom line is you will improve the quality of your nursing care by understanding, respecting, and responding to a patient's experiences, values, beliefs, and preferences.[16]
This chapter will focus on developing culturally competency and cultural humility and providing culturally responsive care.
Learning Objectives
- Reflect upon personal and cultural values, beliefs, biases, and heritage[17]
- Embrace diversity, equity, inclusivity, health promotion, and health care for individuals of diverse geographic, cultural, ethnic, racial, gender, and spiritual backgrounds across the life span[18]
- Demonstrate respect, equity, and empathy in actions and interactions with all health care consumers[19]
- Participate in life-long learning to understand cultural preferences, worldviews, choices, and decision-making processes of diverse patients[20]
- Protect patient dignity
- Demonstrate principles of patient-centered care and cultural humility
- Make adaptations to patient care to reduce health disparities
- Adhere to the Patient's Bill of Rights
- Identify strategies to advocate for patients
- Use evidence-based practices
No matter who we are or where we come from, every person belongs to a culture. The impact of culture on a person’s health is profound because it affects many health beliefs, such as perceived causes of illness, ways to prevent illness, and acceptance of medical treatments. Culturally responsive care integrates these cultural beliefs into an individual's health care. Culturally responsive care is intentional and promotes trust and rapport with patients. At its heart, culturally responsive care is patient-centered care. The American Nurses Association (ANA) states, "The art of nursing is demonstrated by unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care."[21]
Nurses provide holistic care when incorporating their patients’ physical, mental, spiritual, cultural, and social needs into their health care (referred to as holism). As a nursing student, you are undertaking a journey of developing cultural competency with an attitude of cultural humility as you learn how to provide holistic care to your patients. Cultural competency is a lifelong process of applying evidence-based nursing in agreement with the cultural values, beliefs, worldview, and practices of patients to produce improved patient outcomes.[22],[23],[24] Cultural humility is defined by the American Nurses Association as, "A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot know everything about other cultures, and approach learning about other cultures as a life-long goal and process.[25] The bottom line is you will improve the quality of your nursing care by understanding, respecting, and responding to a patient's experiences, values, beliefs, and preferences.[26]
This chapter will focus on developing culturally competency and cultural humility and providing culturally responsive care.

