6.6 Neurological Assessment
Open Resources for Nursing (Open RN)
Now that we have reviewed tests included in a neurological exam, let’s review components of a routine neurological assessment typically performed by registered nurses. The neurological assessment begins by collecting subjective data followed by a physical examination.
Subjective Assessment
Subjective data collection guides the focus of the physical examination. Collect data from the patient using effective communication and pay particular attention to what the patient is reporting, including current symptoms and any history of neurological illness. Ask follow-up questions related to symptoms such as confusion, headache, vertigo, seizures, recent injury or fall, weakness, numbness, tingling, difficulty swallowing (called dysphagia) or speaking (called dysphasia), or lack of coordination of body movements.[1]
See Table 6.10a for sample interview questions to use during the subjective assessment
Table 6.10a Interview Questions Related to Subjective Assessment of Neurological System
| Interview Questions | Follow-up |
|---|---|
| Are you experiencing any current neurological concerns such as headache, dizziness, weakness, numbness, tingling, tremors, loss of balance, or decreased coordination?
Have you experienced any difficulty swallowing or speaking? Have you experienced any recent falls? |
If the patient is seeking care for an acute neurological problem, use the PQRSTU method to further evaluate their chief complaint. The PQRSTU method is described in the “Health History” chapter.
Note: If critical findings of an acute neurological event are actively occurring, such as signs of a stroke, obtain emergency assistance according to agency policy. |
| Have you ever experienced a neurological condition such as a stroke, transient ischemic attack, seizures, or head injury? | Describe the condition(s), date(s), and treatment(s). |
| Are you currently taking any medications, herbs, or supplements for a neurological condition? | Please describe. |
Life Span Considerations
Newborn
At birth, the neurologic system is not fully developed. The brain is still developing, and the newborn’s anterior fontanelle doesn’t close until approximately 18 months of age. The sensory and motor systems gradually develop in the first year of life. The newborn’s sensory system responds to stimuli by crying or moving body parts. Initial motor activity is primitive in the form of newborn reflexes. Additional information about newborn reflexes is provided in the “Assessing Reflexes” section. As the newborn develops, so do the motor and sensory integration. Specific questions to ask parents or caregivers of infants include the following:
- Have you noticed your infant sleeping excessively or having difficulty arousing?
- Has your infant had difficulty feeding, sucking, or swallowing?
Children
Depending on the child’s age and developmental level, they may answer questions independently or the child’s parent/guardian may provide information. Specific questions for children include the following:
- Have you ever had a head injury or a concussion?
- Do you experience headaches? If so, how often?
- Have you had a seizure or convulsion?
- Have you noticed if your child has any problems with walking or balance?
- Have you noticed if your child experiences episodes of not being aware of their environment?
Older Adults
The aging adult experiences a general slowing in nerve conduction, resulting in a slowed motor and sensory interaction. Fine coordination, balance, and reflex activity may be impaired. There may also be a gradual decrease in cerebral blood flow and oxygen use that can cause dizziness and loss of balance. Examples of specific subjective questions for the older adult include the following:
- Have you ever had a head injury or recent fall?
- Do you experience any shaking or tremors of your hands? If so, do they occur more with rest or activity?
- Have you had any weakness, numbness, or tingling in any of your extremities?
- Have you noticed a problem with balance or coordination?
- Do you ever feel lightheaded or dizzy? If so, does it occur with activity or change in position?
Objective Assessment
The physical examination of the neurological system includes assessment of both the central and peripheral nervous systems. A routine neurological exam usually starts by assessing the patient’s mental status followed by evaluation of sensory function and motor function. Comprehensive neurological exams may further evaluate cranial nerve function and deep tendon reflexes. The nurse must be knowledgeable of what is normal or expected for the patient’s age, development, and condition to analyze the meaning of the data that is being collected.
Inspection
Nurses begin assessing a patient’s overall neurological status by observing their general appearance, posture, ability to walk, and personal hygiene in the first few minutes of nurse-patient interaction. For additional information about obtaining an overall impression of a patient’s status while performing an assessment, see the “General Survey” chapter.
Level of orientation is assessed and other standardized tools to evaluate a patient’s mental status may be used, such as the Glasgow Coma Scale (GCS), NIH Stroke Scale, or Mini-Mental State Exam (MMSE). Read more information about these tools under the “Assessing Mental Status” section earlier in this chapter.
The nurse also assesses a patient’s cerebellar function by observing their gait and balance. See the “Assessing Cerebellar Function” section earlier in chapter for more information.
Auscultation
Auscultation refers to the action of listening to sounds from the heart, lungs, or other organs with a stethoscope as a part of physical examination. Auscultation is not typically performed by registered nurses during a routine neurological assessment. However, advanced practice nurses and other health care providers may auscultate the carotid arteries for the presence of a swishing sound called a bruit. Bruits suggest interference with cerebral blood flow that can cause neurological deficits.
Palpation
Palpation during a physical examination typically refers to the use of touch to evaluate organs for size, location, or tenderness, but palpation during the neurologic physical exam involves using touch to assess sensory function and motor function. Refer to sections on “Assessing Sensory Function,” “Assessing Motor Function,” “Assessing Cranial Nerves,” and “Assessing Reflexes” earlier in this chapter for additional information on how to perform these tests.
See Table 6.10b for a summary of expected and unexpected findings when performing an adult neurological assessment.
Table 6.10b Expected Versus Unexpected Findings on Adult Neurological Assessment
| Assessment | Expected Findings | Unexpected Findings (Document and notify provider if new finding*) |
|---|---|---|
| Inspection | Alert and oriented to person, place, and time
Symmetrical facial expressions Clear and appropriate speech Ability to follow instructions PERRLA (Pupils are equal, round, and reactive to light and accommodation) Cranial nerves all intact Negative Romberg test Sensory function present Cortical functioning (indicated by stereognosis) intact Good balance Coordinated gait with equal arm swing Finger-to-nose, rapid alternating arm movements, and heel-to-shin performance intact Negative pronator drift test Motor strength in upper and lower extremities equal bilaterally Deep tendon reflexes intact |
Not alert and oriented to person, place, and/or time
Asymmetrical facial expressions Garbled speech Inability to follow directions Pupils unequal in size or reactivity Deficits in one or more cranial nerve assessments Positive Romberg test Sensory function impaired in one or more areas Stereognosis not intact Poor balance Shuffled or asymmetrical gait with unequal arm swing Unable to complete finger-to-nose, alternating arm movement, or heel-to-shin tests Positive pronator drift test Unequal strength of upper and/or lower extremities One or more deep tendon reflexes are not reactive
|
| Critical findings to report immediately and/or obtain emergency assistance: | Change in mental status, pupil responsiveness, facial drooping, slurred words or inability to speak, or sudden unilateral loss of motor strength |
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
When assessing a patient’s oxygenation status, it is important for the nurse to have an understanding of the underlying structures of the respiratory system to best understand their assessment findings. Visit the “Respiratory Assessment" chapter for more information about the structures of the respiratory system.
Video Review for Oxygenation Basics
View the TED-Ed Oxygen's Journey video on YouTube[1]
Breathing Mechanics[2]
Gas Exchange[3]
Carbon Dioxide Transport[4]
Assessing Oxygenation Status
A patient’s oxygenation status is routinely assessed using pulse oximetry, referred to as SpO2. SpO2 is an estimated oxygenation level based on the saturation of hemoglobin measured by a pulse oximeter. Because the majority of oxygen carried in the blood is attached to hemoglobin within the red blood cell, SpO2 estimates how much hemoglobin is “saturated” with oxygen. The target range of SpO2 for an adult is 94-98%.[5] For patients with chronic respiratory conditions, such as COPD, the target range for SpO2 is often lower at 88% to 92%. Although SpO2 is an efficient, noninvasive method to assess a patient’s oxygenation status, it is an estimate and not always accurate. For example, if a patient is severely anemic and has a decreased level of hemoglobin in the blood, the SpO2 reading is affected. Decreased peripheral circulation can also cause a misleading low SpO2 level.
A more specific measurement of oxygen and carbon dioxide in the blood is obtained through an arterial blood gas (ABG). ABG results are often obtained for patients who have deteriorating or unstable respiratory status requiring urgent and emergency treatment. An ABG is a blood sample that is typically drawn from the radial artery by a respiratory therapist, emergency or critical care nurse, or health care provider. ABG results evaluate oxygen, carbon dioxide, pH, and bicarbonate levels. The partial pressure of oxygen in the blood is referred to as PaO2. The normal PaO2 level of a healthy adult is 80 to 100 mmHg. The PaO2 reading is more accurate than a SpO2 reading because it is not affected by hemoglobin levels. The PaCO2 level is the partial pressure of carbon dioxide in the blood. The normal PaCO2 level of a healthy adult is 35-45 mmHg. The normal range of pH level for arterial blood is 7.35-7.45, and the normal range for the bicarbonate (HCO3) level is 22-26. The SaO2 level is also obtained, which is the calculated arterial oxygen saturation level. See Table 11.2a for a summary of normal ranges of ABG values.[6]
Table 11.2a Normal Ranges of ABG Values
| Value | Description | Normal Range |
|---|---|---|
| pH | Acid-base balance of blood | 7.35-7.45 |
| PaO2 | Partial pressure of oxygen | 80-100 mmHg |
| PaCO2 | Partial pressure of carbon dioxide | 35-45 mmHg |
| HCO3 | Bicarbonate level | 22-26 mEq/L |
| SaO2 | Calculated oxygen saturation | 95-100% |
Hypoxia and Hypercapnia
Hypoxia is defined as a reduced level of tissue oxygenation. Hypoxia has many causes, ranging from respiratory and cardiac conditions to anemia. Hypoxemia is a specific type of hypoxia that is defined as decreased partial pressure of oxygen in the blood (PaO2), measured by an arterial blood gas (ABG).
Early signs of hypoxia are anxiety, confusion, and restlessness. As hypoxia worsens, the patient’s level of consciousness and vital signs will worsen, with increased respiratory rate and heart rate and decreased pulse oximetry readings. Late signs of hypoxia include bluish discoloration of the skin and mucous membranes called cyanosis. Cyanosis is most easily seen around the lips and in the oral mucosa. A sign of chronic hypoxia is clubbing, a gradual enlargement of the fingertips (see Figure 11.1[7]). See Table 11.2b for symptoms and signs of hypoxia.[8]

Hypercapnia is an elevated level of carbon dioxide in the blood. This level is measured by the PaCO2 level in an ABG test and is indicated when the PaCO2 level is higher than 45. Hypercapnia is typically caused by hypoventilation or areas of the alveoli that are ventilated but not perfused. In a state of hypercapnia or hypoventilation, there is an accumulation of carbon dioxide in the blood. The increased carbon dioxide causes the pH of the blood to drop, leading to a state of respiratory acidosis. You can read more about respiratory acidosis in the “Fluids and Electrolytes” chapter of the Open RN Nursing Fundamentals book. Patients with hypercapnia can present with tachycardia, dyspnea, flushed skin, confusion, headaches, and dizziness. If the hypercapnia develops gradually over time, such as in a patient with chronic obstructive pulmonary disease (COPD), symptoms may be mild or may not be present at all. Hypercapnia is managed by addressing its underlying cause. A noninvasive positive pressure device such as a BiPAP may provide support to patients who are having trouble breathing normally, but if this is not sufficient, intubation may be required.[9]
Table 11.2b Symptoms and Signs of Hypoxia
| Signs & Symptoms | Description |
|---|---|
| Restlessness | Patient may become increasingly fidgety, move about the bed, demonstrate signs of anxiety and agitation. Restlessness is an early sign of hypoxia. |
| Tachycardia | An elevated heart rate (above 100 beats per minute in adults) can be an early sign of hypoxia. |
| Tachypnea | An increased respiration rate (above 20 breaths per minute in adults) is an indication of respiratory distress. |
| Shortness of breath (Dyspnea) | Shortness of breath is a subjective symptom of not getting enough air. Depending on severity, dyspnea causes increased levels of anxiety. |
| Oxygen saturation level (SpO2) | Oxygen saturation levels should be above 94% for an adult without an underlying respiratory condition. |
| Use of accessory muscles | Use of neck or intercostal muscles when breathing is an indication of respiratory distress. |
| Noisy breathing | Audible noises with breathing are an indication of respiratory conditions. Assess lung sounds with a stethoscope for adventitious sounds such as wheezing, rales, or crackles. Secretions can plug the airway, thereby decreasing the amount of oxygen available for gas exchange in the lungs. |
| Flaring of nostrils or pursed lip breathing | Flaring is a sign of hypoxia, especially in infants. Pursed-lip breathing is a technique often used in patients with COPD. This breathing technique increases the amount of carbon dioxide exhaled so that more oxygen can be inhaled. |
| Position of patient | Patients in respiratory distress may sit up or lean over by resting arms on their legs to enhance lung expansion. Patients who are hypoxic may not be able to lie flat in bed. |
| Ability of patient to speak in full sentences | Patients in respiratory distress may be unable to speak in full sentences or may need to catch their breath between sentences. |
| Skin color (Cyanosis) | Changes in skin color to bluish or gray are a late sign of hypoxia. |
| Confusion or loss of consciousness (LOC) | This is a worsening sign of hypoxia. |
| Clubbing | Clubbing, a gradual enlargement of the fingertips, is a sign of chronic hypoxia. |
Treating Hypoxia
Acute hypoxia is a medical emergency and should be treated promptly with oxygen therapy. Failure to initiate oxygen therapy when needed can result in serious harm or death of the patient. Although oxygen is considered a medication that requires a prescription, oxygen therapy may be initiated without a physician’s order in emergency situations as part of the nurse’s response to the “ABCs,” a common abbreviation for airway, breathing, and circulation. Most agencies have a protocol in place that allows nurses to apply oxygen in emergency situations. After applying oxygen as needed, the nurse then contacts the provider, respiratory therapist, or rapid response team, depending on the severity of hypoxia. Devices such high flow oxymasks, CPAP, BiPAP, or mechanical ventilation may be initiated by the respiratory therapist or provider to deliver higher amounts of inspired oxygen. Various types of oxygenation devices are further explained in the “Oxygenation Equipment” section.
Prescription orders for oxygen therapy will include two measurements of oxygen to be delivered - the oxygen flow rate and the fraction of inspired oxygen (FiO2). The oxygen flow rate is the number dialed up on the oxygen flow meter between 1 L/minute and 15 L/minute. Fio2 is the concentration of oxygen the patient inhales. Room air contains 21% oxygen concentration, so the FiO2 for supplementary oxygen therapy will range from 21% to 100% concentration.
In addition to administering oxygen therapy, there are several other interventions the nurse should consider implementing to a hypoxic patient. Additional interventions used to treat hypoxia in conjunction with oxygen therapy are outlined in Table 11.2c.[10]
Table 11.2c Interventions to Manage Hypoxia
| Interventions | Additional Information |
|---|---|
| Raise the Head of the Bed | Raising the head of the bed to high Fowler’s position promotes effective chest expansion and diaphragmatic descent, maximizes inhalation, and decreases the work of breathing. Patients with COPD who are short of breath may gain relief by sitting upright or leaning over a bedside table while in bed. |
| Encourage Enhanced Breathing and Coughing Techniques | Enhanced breathing and coughing techniques such as using pursed-lip breathing, coughing and deep breathing, huffing technique, incentive spirometry, and flutter valves may assist patients to clear their airway while maintaining their oxygen levels. See the following “Enhanced Breathing and Coughing Techniques” section for additional information regarding these techniques. |
| Manage Oxygen Therapy and Equipment | If the patient is already on supplemental oxygen, ensure the equipment is turned on, set at the required flow rate, correctly positioned on the patient, and properly connected to an oxygen supply source. If a portable tank is being used, check the oxygen level in the tank. Ensure the connecting oxygen tubing is not kinked, which could obstruct the flow of oxygen. Feel for the flow of oxygen from the exit ports on the oxygen equipment. In hospitals where medical air and oxygen are used, ensure the patient is connected to the oxygen flow port. Hospitals in America follow the national standard that oxygen flow ports are green and air outlets are yellow. |
| Assess the Need for Respiratory Medications | Pharmacological management is essential for patients with respiratory disease such as asthma, COPD, or severe allergic response. Bronchodilators effectively relax smooth muscles and open airways. Glucocorticoids relieve inflammation and also assist in opening air passages. Mucolytics decrease the thickness of pulmonary secretions so that they can be expectorated more easily. |
| Provide Oral Suctioning if Needed | Some patients may have a weakened cough that inhibits their ability to clear secretions from the mouth and throat. Patients with muscle disorders or those who have experienced a cerebral vascular accident (CVA) are at risk for aspiration pneumonia, which is caused by the accidental inhalation of material from the mouth or stomach. Provide oral suction if the patient is unable to clear secretions from the mouth and pharynx. See the chapter on “Tracheostomy Care and Suctioning” for additional details on suctioning. |
| Provide Pain Relief If Needed | Provide adequate pain relief if the patient is reporting pain. Pain increases anxiety and may inhibit the patient’s ability to take in full breaths. |
| Consider the Side Effects of Pain Medications | A common side effect of pain medication is sedation and respiratory depression. For more information about interventions to manage respiratory depression, see the “Oxygenation” chapter in the Open RN Nursing Fundamentals textbook. |
| Consider Other Devices to Enhance Clearance of Secretions | Chest physiotherapy and specialized devices assist with secretion clearance, such as handheld flutter valves or vests that inflate and vibrate the chest wall. Consider requesting a consultation with a respiratory therapist based on the patient’s situation. |
| Plan Frequent Rest Periods Between Activities | Patients experiencing hypoxia often feel short of breath and fatigue easily. Allow the patient to rest frequently, and space out interventions to decrease oxygen demand in patients whose reserves are likely limited. |
| Consider Other Potential Causes of Dyspnea | If a patient’s level of dyspnea is worsening, assess for other underlying causes in addition to the primary diagnosis. Are there other respiratory, cardiovascular, or hematological conditions such as anemia occurring? Start by reviewing the patient’s most recent hemoglobin and hematocrit lab results. Completing a thorough assessment may reveal abnormalities in these systems to report to the health care provider. |
| Consider Obstructive Sleep Apnea | Patients with obstructive sleep apnea (OSA) are often not previously diagnosed prior to hospitalization. The nurse may notice the patient snores, has pauses in breathing while snoring, or awakens not feeling rested. These signs may indicate the patient is unable to maintain an open airway while sleeping, resulting in periods of apnea and hypoxia. If these apneic periods are noticed but have not been previously documented, the nurse should report these findings to the health care provider for further testing and follow-up. Testing consists of using continuous pulse oximetry while the patient is sleeping to determine if the patient is hypoxic during these episodes and if a CPAP device should be prescribed. See the box below for additional information regarding OSA. |
| Anxiety | Anxiety often accompanies the feeling of dyspnea and can worsen it. Anxiety in patients with COPD is chronically undertreated. It is important for the nurse to address the feelings of anxiety and dyspnea. Anxiety can be relieved by teaching enhanced breathing and coughing techniques, encouraging relaxation techniques, or administering antianxiety medications. |
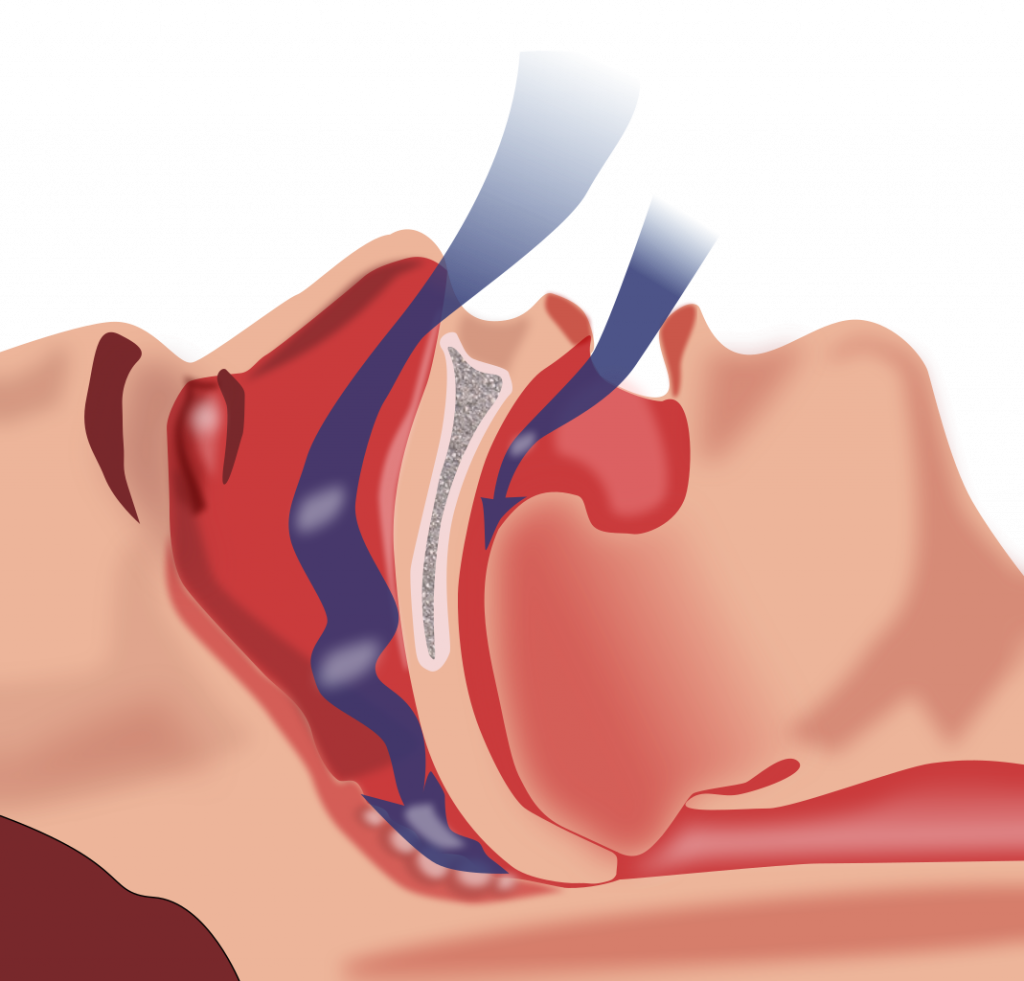
Obstructive Sleep Apnea (OSA) is the most common type of sleep apnea. See Figure 11.2[11] for an illustration of OSA. As soft tissue falls to the back of the throat, it impedes the passage of air (blue arrows) through the trachea and is characterized by repeated episodes of complete or partial obstructions of the upper airway during sleep. The episodes of breathing cessations are called “apneas,” meaning “without breath.” Despite the effort to breathe, apneas are associated with a reduction in blood oxygen saturation due to the obstruction of the airway. Treatment for OSA often includes the use of a CPAP device.
Enhanced Breathing and Coughing Techniques
In addition to oxygen therapy and the interventions listed in Table 11.2c to implement for a patient experiencing dyspnea and hypoxia, there are several techniques a nurse can teach a patient to use to enhance their breathing and coughing. These techniques include pursed-lip breathing, incentive spirometry, coughing and deep breathing, and the huffing technique.
Pursed-Lip Breathing
Pursed-lip breathing is a technique that allows people to control their oxygenation and ventilation. The technique requires a person to inspire through the nose and exhale through the mouth at a slow controlled flow. See Figure 11.3[12] for an illustration of pursed-lip breathing. This type of exhalation gives the person a puckered or pursed appearance. By prolonging the expiratory phase of respiration, a small amount of positive end-expiratory pressure (PEEP) is created in the airways that helps to keep them open so that more air can be exhaled, thus reducing air trapping that occurs in some conditions such as COPD. Pursed-lip breathing often relieves the feeling of shortness of breath, decreases the work of breathing, and improves gas exchange. People also regain a sense of control over their breathing while simultaneously increasing their relaxation.[13]

View the COPD Foundation's YouTube video to learn more about pursed-lip breathing:
Breathing Techniques[14]
Incentive Spirometry
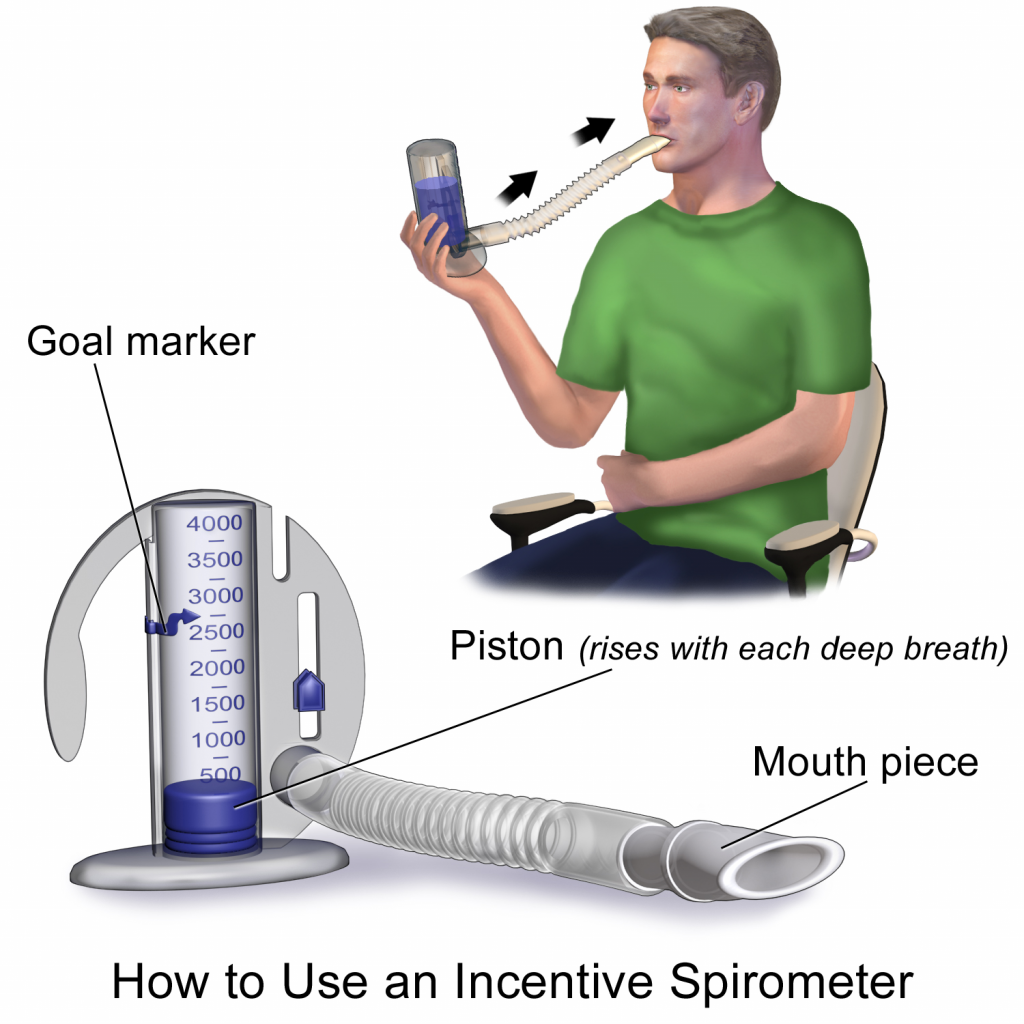
An incentive spirometer is a medical device often prescribed after surgery to prevent and treat atelectasis. Atelectasis occurs when alveoli become deflated or filled with fluid and can lead to pneumonia. See Figure 11.4[15] for an image of a patient using an incentive spirometer. While sitting upright, the patient should breathe in slowly and deeply through the tubing with the goal of raising the piston to a specified level. The patient should attempt to hold their breath for 5 seconds, or as long as tolerated, and then rest for a few seconds. This technique should be repeated by the patient 10 times every hour while awake.[16] The nurse may delegate this intervention to unlicensed assistive personnel, but the frequency in which it is completed and the volume achieved should be documented and monitored by the nurse.
Coughing and Deep Breathing
Teaching the coughing and deep breathing technique is similar to incentive spirometry but no device is required. The patient is encouraged to take deep, slow breaths and then exhale slowly. After each set of breaths, the patient should cough. This technique is repeated 3 to 5 times every hour.
Huffing Technique
The huffing technique is helpful for patients who have difficulty coughing. Teach the patient to inhale with a medium-sized breath and then make a sound like “Ha” to push the air out quickly with the mouth slightly open.
Vibratory PEP Therapy
Vibratory Positive Expiratory Pressure (PEP) therapy uses handheld devices such as “flutter valves” or “Acapella” devices for patients who need assistance in clearing mucus from their airways. These devices (see Figure 11.5[17]) require a prescription and are used in collaboration with a respiratory therapist or advanced health care provider. To use Vibratory PEP therapy, the patient should sit up, take a deep breath, and blow into the device. A flutter valve within the device creates vibrations that help break up the mucus so the patient can cough it up and spit it out. Additionally, a small amount of positive end-expiratory pressure (PEEP) is created in the airways that helps to keep them open so that more air can be exhaled.

Visit NHS University Hospitals Plymouth Physiotherapy's "Acapella" video on YouTube to review using a flutter valve device[18]
A state of being free of disease-causing microorganisms.
To put on equipment for personal protection, such as gloves or a gown.

