23.2 IV Therapy Basics
Open Resources for Nursing (Open RN)
Primary IV Fluid Infusion
Primary IV fluid infusions are prescribed by health care providers to restore or maintain hydration and electrolyte status within the body. When administering IV fluids to a patient, the nurse must continually monitor the patient’s fluid and electrolyte status to evaluate the effectiveness of the infusion and to avoid potential complications of fluid overload and electrolyte imbalance.
The most commonly used primary IV fluid bag contains 1,000 mL. There are also 500 mL, 250 mL, 100 mL, and 50 mL bags. The size of the primary fluid bag is based on infusion need, patient condition, and age. Most adult patients receive continuous IV fluids with 1,000 mL bags due to the higher drip (gtt) rate. Many other fluid volume bags are used for intermittent infusions or short-term therapy.
For example, for renal dialysis patients, IV bags smaller than 1,000 mL are used because large amounts of continuous fluids are contraindicated due to their renal impairment. Many institutions will hang smaller volume normal saline continuous infusion bags just to serve as an additional reminder that these patients should not receive large amounts of primary fluids. Another example of patients requiring smaller IV bags are pediatric patients who, due to their smaller anatomical size, do not require large primary fluid infusion volumes.
Primary fluids are typically administered using an IV pump. An IV pump is the safest method of administration to ensure specific amounts of fluid are administered. However, there may be situations when IV pumps are not available and nurses administer primary fluids by gravity using drip tubing. Read more about calculating infusion rates in the “Math Calculation” chapter.
Primary fluids are run at consistent infusion rates for a prescribed period of time. For example, a continuous fluid infusion may be ordered at a rate of 125 mL/hour for 24 hours. Continuous fluids may also be ordered to run until the provider gives a follow-up order to discontinue or decrease the fluid rate.
IV primary fluid bags consist of various types of fluid such as 0.9% normal saline, 0.45% (½) normal saline, lactated ringers solution, and dextrose (5%) preparations. They may also contain replacement electrolytes like potassium chloride. The provider will order primary fluids based on the patient’s fluid and electrolyte statuses.
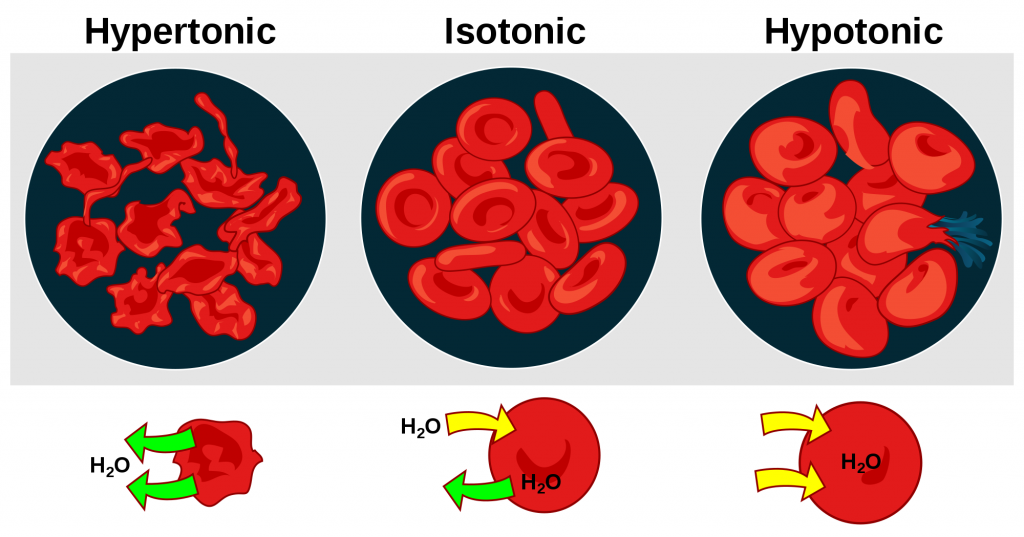
There are three types of intravenous fluid concentrations: isotonic, hypertonic, and hypotonic fluids.
- Isotonic fluids are typically administered for fluid and electrolyte replacement. Isotonic fluids have a similar concentration to the solutes contained in blood, so they do not cause the osmotic movement of fluid into or out of the patient’s individual cells. An example of isotonic fluid is 0.9% normal saline.
- Hypertonic fluids have a higher concentration of solutes than blood. They are typically used in critical care situations to treat hyponatremia and avoid pulmonary edema by relying on osmosis to help remove excess fluid. An example of a hypertonic fluid is dextrose 5% in 0.9% normal saline (D5NS).
- Hypotonic fluids have a lower concentration of solutes than blood. The goal of hypotonic fluid administration is to move fluids into a patient’s cells due to osmosis. Hypotonic solutions are commonly used when a patient has severe intracellular dehydration such as during diabetic ketoacidosis. An example of hypotonic fluid is 0.45% normal saline (1/2NS). See Figure 23.1[1] for an example of the effects of the administration of hypertonic, isotonic, and hypotonic IV fluids on a patient’s red blood cells.
Because a patient’s fluid and electrolyte statuses are constantly changing when receiving IV fluids, it is important for the nurse to monitor for signs of fluid or electrolyte imbalances and appropriately notify the health care provider of any concerns. For example, primary fluids may be started at a higher rate of infusion when a patient is receiving nothing by mouth (NPO), but should be tapered as they resume normal diet and fluid intake. It is important for the nurse to continually monitor a patient’s skin turgor, urinary output, lung sounds, and oxygen requirements and to assess for any new edema to offer important insight into their fluid volume status. A nurse must also evaluate the effects of replacement fluids and discuss their ongoing need with the prescribing provider.
Secondary Fluid Infusion
Secondary IV fluid administration is usually an intermittent infusion that infuses at regular intervals (e.g., every 8 hours). This form of IV therapy usually contains medications that are supplied in a smaller infusion bag and mixed with a diluent fluid like saline (e.g., IV antibiotics). Many common preparations come in 25 to 100 mL bags.
Secondary IV therapy is often referred to as “IV piggyback” (IVPB) medication because it is attached to the primary bag of intravenous fluids. In this case, the primary line maintains venous access between drug doses.
It is important to remember that not all IV solutions are compatible with all IV medications. It is vital for the nurse to triple check that the secondary medications/fluids are compatible with primary fluids. If medication and fluids are not compatible, a precipitate may form when the fluids mix within the line, posing a significant health danger for the patient.
IV Administration Equipment
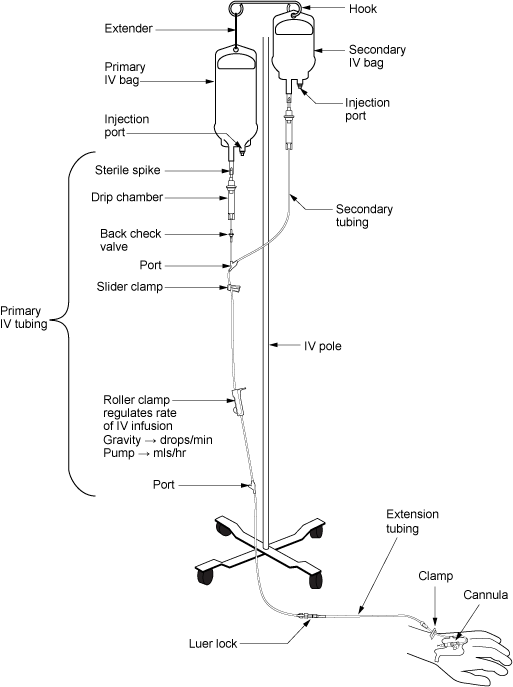
Intravenous (IV) fluids and medications are administered through flexible plastic tubing called an IV administration set. The IV administration set connects the bag of solution to the patient’s IV access site. There are two major types of IV administration sets: primary tubing and secondary tubing. Additionally, IV fluids can be administered by gravity or by infusion pump, and each method requires its own administration set.
Primary and Secondary Administration Sets
Primary IV Administration Sets
Primary IV administration sets are used to infuse continuous or intermittent fluids or medications. Primary IV tubing can be a macro-drip or micro-drip solution set. A macro-drip infusion set delivers 10, 15, or 20 drops per milliliter, whereas a micro-drip infusion set delivers 60 drops per milliliter. The drop factor is located on the packaging of the IV tubing and is important to verify when calculating medication administration rates. Macro-drip sets are used for routine primary infusions for adults. Micro-drip IV tubing is used in pediatric or neonatal care where small amounts of fluids are administered over a long period of time.
Primary IV administration sets consist of the following parts:
Sterile spike: This part of the tubing must be kept sterile as you spike the IV fluid bag.
Drip chamber: The drip chamber allows air to rise out from a fluid so that it is not passed onto the patient. It is also used to calculate the rate at which fluid is administered by gravity (drops per minute). It should be kept ¼ to ½ full of solution.
Backcheck valve: A backcheck valve prevents fluid or medication from travelling up into the primary IV bag.
Access ports: Access ports are used to infuse secondary medications and to administer IV push medications. These may also be referred to as “Y ports.”
Roller clamp: A roller clamp is used to regulate the speed, or stop, an infusion by gravity.
Secondary IV Administration Sets
Secondary IV administration sets are used to intermittently administer a secondary medication, such as an antibiotic, while the primary IV is also running. Secondary IV tubing is shorter in length than primary tubing and is connected to a primary line via an access port or an IV pump. The secondary infusion is hung above the primary infusion and connected at an access port.
Secondary fluids should always be “piggybacked” into primary infusion lines to ensure that the correct amount of medication is infused. By piggybacking a medication, the solution from the primary fluid line is used to prime the secondary tubing. However, if a secondary infusion is run as a primary fluid, there is a risk of losing some of the secondary medication when priming the line, which results in less medication being administered. Loss of medication is considered a medication error because the patient received less active medication than prescribed.
See Figure 23.2[2] for an illustration of the set up of a primary and secondary tubing for administration of fluids and a secondary medication by gravity. See Figure 23.3[3] for an example of an IV infusion pump.

IV Administration
When initiating or changing an IV bag of fluids or medications, it is important to remember these items:
- IV fluids are a medication. Verify physician orders and check that the patient does not have an allergy to this medication. Perform the six rights of medication administration three times as you would when giving any other medication. Check the type of fluid and the expiration date, and verify the fluid is free of discoloration and sediment. Check the expiration date when obtaining a new tubing administration set.
- Examine the bag to ensure that the bag itself is intact and not leaking. There may be moisture on the inside of the plastic IV bag storage container; this is normal.
- Verify the infusion rate of IV fluids is appropriate based on the patient’s age, size, preexisting medical conditions, and prescribed indication. If a manual calculation is needed to set the IV flow rate, calculate the rate and double-check the calculated rate with another registered nurse.
- IV tubing administration sets require routine replacement to prevent infection. Follow agency policy regarding initiating tubing change before initiating a new bag of fluid or medications.
- If administration set tubing is present, trace the tubing from the patient to its point of origin to make sure that you’re accessing the correct port.
- Assess the IV site. Inspect for redness, swelling, or tenderness that can be a sign of irritation, inflammation, or infection.
- Ensure the IV site is patent when initiating new fluid or medication. Aspirate for blood return and flush the IV catheter according to agency policy.
Complications of IV Therapy
While monitoring a patient receiving IV fluids, it is important to assess for potential complications such as infiltration, extravasation, phlebitis, or infection. If these conditions occur, promptly notify the provider for treatment; the IV catheter will need to be removed and replaced at an alternative site, and additional medication may be prescribed.
Infiltration occurs when the tip of the catheter slips out of the vein. The catheter passes through the wall of the vein, or the blood vessel wall allows part of the fluid to infuse into the surrounding tissue, resulting in the leakage of IV fluids into the surrounding tissue. Infiltration may cause pain, swelling, and skin that is cool to the touch. If you are concerned an IV is infiltrated, follow your facility policy and, as a general guideline, discontinue the site and relocate the IV. If the infiltration is severe, you may consider the application of a compress in addition to elevating the affected limb. Check your institution’s policy regarding which type of compress (warm or cold) should be applied.[4],[5] Additionally, clinical pharmacists can also be helpful resources for determining the appropriate type of infiltration treatment.
Extravasation refers to infiltration of damaging intravenous medications, such as chemotherapy, into the extravascular tissue around the site of infusion. Extravasation causes tissue injury, and depending on the medication, site, and length of exposure, it can cause tissue death, which is also referred to as necrosis. If detected early, extravasation may be treated with medications that help avoid the complication of necrosis.
Phlebitis is inflammation of a vein. Phlebitis of superficial veins can occur due to trauma to the vein during insertion of the IV catheter. It can cause redness and tenderness along the vein and can lead to infection if not treated appropriately. Treatment may include warm compresses and nonsteroidal anti-inflammatory medications.
Infection can occur whenever the skin barrier is broken by the insertion of an IV catheter. Signs of infection include redness, warmth, tenderness, and possible fever. Vascular catheter–associated infection is considered a hospital-acquired condition because it can be prevented using best practices. Be sure to follow evidence-based infection prevention practices, such as performing hand hygiene, performing a vigorous mechanical scrub of needleless connectors, limiting catheter access, and following sterile no-touch technique during intravenous infusion to reduce the risk of vascular catheter–associated infection.
- “Osmotic pressure on blood cells diagram.svg“ by LadyofHats is in the Public Domain ↵
- “intravenous_equipment_labels-2.png” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/8-2-types-of-iv-therapy/ ↵
- “DSC_0738-e1443533768679-678x1024.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/8-2-types-of-iv-therapy/ ↵
- Drugs.com [Internet]. IV Infiltration. © 2000-2020 [updated 3 February, 2020; cited 7 August, 2020]. https://www.drugs.com/cg/iv-infiltration-aftercare-instructions.html ↵
- AMN Healthcare Education Services. (2015). Know the difference: Infiltration versus extravasation. https://www.rn.com/nursing-news/know-the-difference-infiltration-vs-extravasation/ ↵

