22.6 Checklist for Tracheostomy Care and Sample Documentation
Open Resources for Nursing (Open RN)
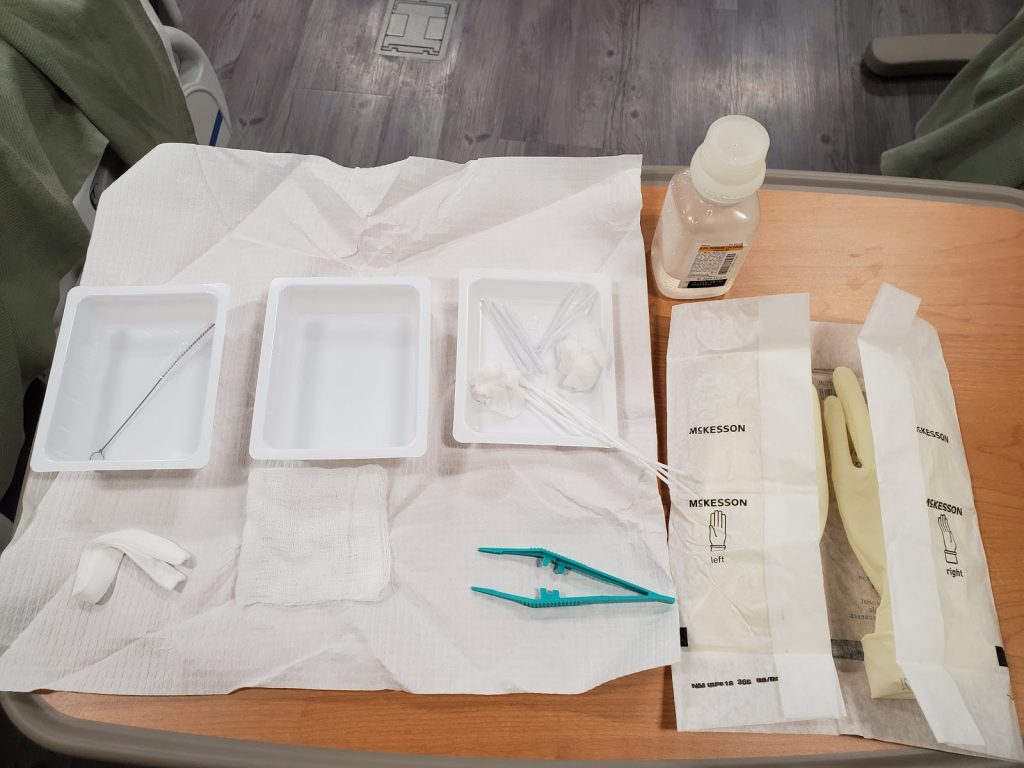
Tracheostomy care is provided on a routine basis to keep the tracheostomy tube’s flange, inner cannula, and surrounding area clean to reduce the amount of bacteria entering the artificial airway and lungs. See Figure 22.9[1] for an image of a sterile tracheostomy care kit.
Replacing and Cleaning an Inner Cannula
The primary purpose of the inner cannula is to prevent tracheostomy tube obstruction. Many sources of obstruction can be prevented if the inner cannula is regularly cleaned and replaced. Some inner cannulas are designed to be disposable, while others are reusable for a number of days. Follow agency policy for inner cannula replacement or cleaning, but as a rule of thumb, inner cannula cleaning should be performed every 12-24 hours at a minimum. Cleaning may be needed more frequently depending on the type of equipment, the amount and thickness of secretions, and the patient’s ability to cough up the secretions.
Changing the inner cannula may encourage the patient to cough and bring mucus out of the tracheostomy. For this reason, the inner cannula should be replaced prior to changing the tracheostomy dressing to prevent secretions from soiling the new dressing. If the inner cannula is disposable, no cleaning is required.[2]
Checklist for Tracheostomy Care With a Reusable Inner Cannula
Use the checklist below to review the steps for completion of “Tracheostomy Care.”
Stoma site should be assessed and a clean dressing applied at least once per shift. Wet or soiled dressings should be changed immediately.[3] Follow agency policy regarding clearing the inner cannula; it should be inspected at least twice daily and cleaned as needed.
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies: bedside table, towel, sterile gloves, pulse oximeter, PPE (i.e., mask, goggles, or face shield), tracheostomy suctioning equipment, bag valve mask (should be located in the room), and a sterile tracheostomy care kit (or sterile cotton-tipped applicators, sterile manufactured tracheostomy split sponge dressing, sterile basin, normal saline, and a disposable inner cannula or a small, sterile brush to clean the reusable inner cannula).
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient and ask if they have any questions.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs.
- Raise the bed to waist level and place the patient in a semi-Fowler’s position.
- Verify that there is a backup tracheostomy kit available.
- Don appropriate PPE.
- Perform tracheal suctioning if indicated.
- Remove and discard the trach dressing. Inspect drainage on the dressing for color and amount and note any odor.
- Inspect stoma site for redness, drainage, and signs and symptoms of infection.
- Remove the gloves and perform proper hand hygiene.
- Open the sterile package and loosen the bottle cap of sterile saline.
- Don one sterile glove on the dominant hand.
- Open the sterile drape and place it on the patient’s chest.
- Set up the equipment on the sterile field.
- Remove the cap and pour saline in both basins with ungloved hand (4″-6” above basin).
- Don the second sterile glove.
- Prepare and arrange supplies. Place pipe cleaners, trach ties, trach dressing, and forceps on the field. Moisten cotton applicators and place them in the third (empty) basin. Moisten two 4″ x 4″ pads in saline, wring out, open, and separately place each one in the third basin. Leave one 4″ x 4″ dry.
- With nondominant “contaminated” hand, remove the trach collar (if applicable) and remove (unlock and twist) the inner cannula. If the patient requires continuous supplemental oxygen, place the oxygenation device near the outer cannula or ask a staff member to assist in maintaining the oxygen supply to the patient.
- Place the inner cannula in the saline basin.
- Pick up the inner cannula with your nondominant hand, holding it only by the end usually exposed to air.
- With your dominant hand, use a brush to clean the inner cannula. Place the brush back into the saline basin.
- After cleaning, place the inner cannula in the second saline basin with your nondominant hand and agitate for approximately 10 seconds to rinse off debris. Repeat cleansing with brush as needed.
- Dry the inner cannula with the pipe cleaners and place the inner cannula back into the outer cannula. Lock it into place and pull gently to ensure it is locked appropriately. Reattach the preexisting oxygenation device.
- Clean the stoma with cotton applicators using one on the superior aspect and one on the inferior aspect.
- With your dominant, noncontaminated hand, moisten sterile gauze with sterile saline and wring out excess. Assess the stoma for infection and skin breakdown caused by flange pressure. Clean the stoma with the moistened gauze starting at the 12 o’clock position of the stoma and wipe toward the 3 o’clock position. Begin again with a new gauze square at 12 o’clock and clean toward 9 o’clock. To clean the lower half of the site, start at the 3 o’clock position and clean toward 6 o’clock; then wipe from 9 o’clock to 6 o’clock, using a clean moistened gauze square for each wipe. Continue this pattern on the surrounding skin and tube flange. Avoid using a hydrogen peroxide mixture because it can impair healing.[4]
- Use sterile gauze to dry the area.
- Apply the sterile tracheostomy split sponge dressing by only touching the outer edges.
- Replace trach ties as needed. (The literature overwhelmingly recommends a two-person technique when changing the securing device to prevent tube dislodgement. In the two-person technique, one person holds the trach tube in place while the other changes the securing device). Thread the clean tie through the opening on one side of the trach tube. Bring the tie around the back of the neck, keeping one end longer than the other. Secure the tie on the opposite side of the trach. Make sure that only one finger can be inserted under the tie.
- Remove the old tracheostomy ties.
- Remove gloves and perform proper hand hygiene.
- Provide oral care. Oral care keeps the mouth and teeth not only clean, but also has been shown to prevent hospital-acquired pneumonia.
- Lower the bed to lowest the position. If the patient is on a mechanical ventilator, the head of the bed should be maintained at 30-45 degrees to prevent ventilator-associated pneumonia.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene.
- Document the procedure and related assessment findings. Report any concerns according to agency policy.
Sample Documentation
Sample Documentation of Expected Findings
Tracheostomy care provided with sterile technique. Stoma site free of redness or drainage. Inner cannula cleaned and stoma dressing changed. Patient tolerated the procedure without difficulties.
Sample Documentation of Unexpected Findings
Tracheostomy care provided with sterile technique. Stoma site is erythematous, warm, and tender to palpation. Inner cannula cleaned and stoma dressing changed. Patient tolerated the procedure without difficulties. Dr. Smith notified of change in condition of stoma at 1315 and stated would assess the patient this afternoon.
- “Sterile Tracheostomy Care Kit” by Julie Teeter at Gateway Technical College is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0. ↵
- Nance-Floyd, B. (2011). Tracheostomy care: An evidence-based guide. American Nurse. https://www.myamericannurse.com/tracheostomy-care-an-evidence-based-guide-to-suctioning-and-dressing-changes/ ↵
- Nance-Floyd, B. (2011). Tracheostomy care: An evidence-based guide. American Nurse. https://www.myamericannurse.com/tracheostomy-care-an-evidence-based-guide-to-suctioning-and-dressing-changes/ ↵

