20.2 Basic Concepts Related to Wounds
Open Resources for Nursing (Open RN)
Phases of Wound Healing
When skin is injured, there are four phases of wound healing that take place: hemostasis, inflammatory, proliferative, and maturation.[1] See Figure 20.1[2] for an illustration of the phases of wound healing.
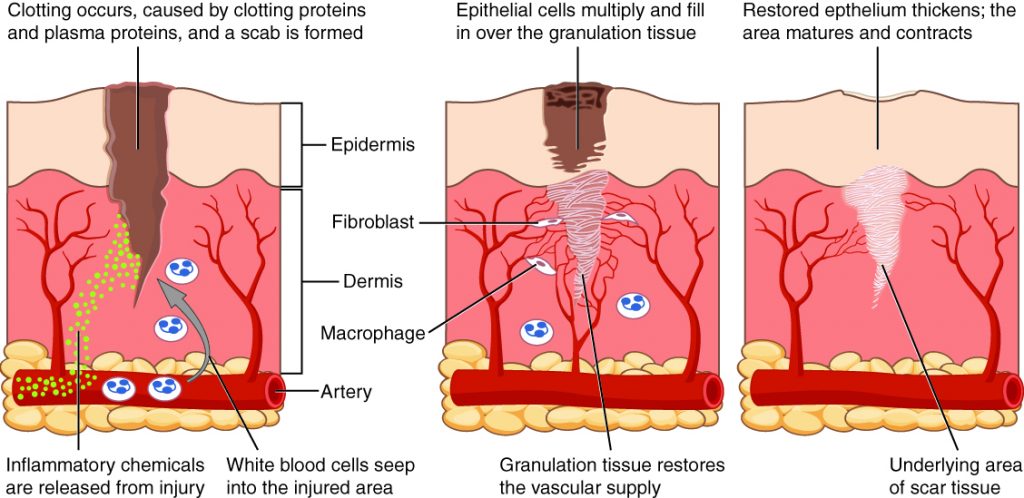
To illustrate the phases of wound healing, imagine that you accidentally cut your finger with a knife as you were slicing an apple. Immediately after the injury occurs, blood vessels constrict and clotting factors are activated. This is referred to as the hemostasis phase. Clotting factors form clots that stop the bleeding and act as a barrier to prevent bacterial contamination. Platelets release growth factors that alert various cells to start the repair process at the wound location. The hemostasis phase lasts up to 60 minutes, depending on the severity of the injury.[3],[4]
After the hemostasis phase, the inflammatory phase begins. Vasodilation occurs so that white blood cells in the bloodstream can move into the wound to start cleaning the wound bed. The inflammatory process appears to the observer as edema (swelling), erythema (redness), and exudate. Exudate is fluid that oozes out of a wound, also commonly called pus.[5],[6]
The proliferative phase begins within a few days after the injury and includes four important processes: epithelialization, angiogenesis, collagen formation, and contraction. Epithelialization refers to the development of new epidermis and granulation tissue. Granulation tissue is new connective tissue with new, fragile, thin-walled capillaries. Collagen is formed to provide strength and integrity to the wound. At the end of the proliferation phase, the wound begins to contract in size.[7],[8]
Capillaries begin to develop within the wound 24 hours after injury during a process called angiogenesis. These capillaries bring more oxygen and nutrients to the wound for healing. When performing dressing changes, it is essential for the nurse to protect this granulation tissue and the associated new capillaries. Healthy granulation tissue appears pink due to the new capillary formation. It is also moist, painless to the touch, and may appear “bumpy.” Conversely, unhealthy granulation tissue is dark red and painful. It bleeds easily with minimal contact and may be covered by shiny white or yellow fibrous tissue referred to as biofilm that must be removed because it impedes healing. Unhealthy granulation tissue is often caused by an infection, so wound cultures should be obtained when infection is suspected. The provider can then prescribe appropriate antibiotic treatment based on the culture results.[9]
During the maturation phase, collagen continues to be created to strengthen the wound. Collagen contributes strength to the wound to prevent it from reopening. A wound typically heals within 4-5 weeks and often leaves behind a scar. The scar tissue is initially firm, red, and slightly raised from the excess collagen deposition. Over time, the scar begins to soften, flatten, and become pale in about nine months.[10]
Types of Wound Healing
There are three types of wound healing: primary intention, secondary intention, and tertiary intention. Healing by primary intention means that the wound is sutured, stapled, glued, or otherwise closed so the wound heals beneath the closure. This type of healing occurs with clean-edged lacerations or surgical incisions, and the closed edges are referred to as approximated. See Figure 20.2[11] for an image of a surgical wound healing by primary intention.

Secondary intention occurs when the edges of a wound cannot be approximated (brought together), so the wound fills in from the bottom up by the production of granulation tissue. Examples of wounds that heal by secondary intention are pressure injuries and chainsaw injuries. Wounds that heal by secondary infection are at higher risk for infection and must be protected from contamination. See Figure 20.3[12] for an image of a wound healing by secondary intention.

Tertiary intention refers to a wound that has had to remain open or has been reopened, often due to severe infection. The wound is typically closed at a later date when infection has resolved. Wounds that heal by secondary and tertiary intention have delayed healing times and increased scar tissue.
Wound Closures
Lacerations and surgical wounds are typically closed with sutures, staples, or dermabond to facilitate healing by primary intention. See Figure 20.4[13] for an image of sutures, Figure 20.5[14] for an image of staples, and Figure 20.6[15] for an image of a wound closed with dermabond, a type of sterile surgical glue. Based on agency policy, the nurse may remove sutures and staples based on a provider order. See Figure 20.7[16] for an image of a disposable staple remover. See the checklists in the subsections later in this chapter for procedures related to surgical and staple removal.




Common Types of Wounds
There are several different types of wounds. It is important to understand different types of wounds when providing wound care because each type of wound has different characteristics and treatments. Additionally, treatments that may be helpful for one type of wound can be harmful for another type. Common types of wounds include skin tears, venous ulcers, arterial ulcers, diabetic foot wounds, and pressure injuries.[17]
Skin Tears
Skin tears are wounds caused by mechanical forces such as shear, friction, or blunt force. They typically occur in the fragile, nonelastic skin of older adults or in patients undergoing long-term corticosteroid therapy. Skin tears can be caused by the simple mechanical force used to remove an adhesive bandage or from friction as the skin brushes against a surface. Skin tears occur in the epidermis and dermis but do not extend through the subcutaneous layer. The wound bases of skin tears are typically fragile and bleed easily.[18]
Venous Ulcers
Venous ulcers are caused by lack of blood return to the heart causing pooling of fluid in the veins of the lower legs. The resulting elevated hydrostatic pressure in the veins causes fluid to seep out, macerate the skin, and cause venous ulcerations. Maceration refers to the softening and wasting away of skin due to excess fluid. Venous ulcers typically occur on the medial lower leg and have irregular edges due to the maceration. There is often a dark-colored discoloration of the lower legs, due to blood pooling and leakage of iron into the skin called hemosiderin staining. For venous ulcers to heal, compression dressings must be used, along with multilayer bandage systems, to control edema and absorb large amounts of drainage.[19] See Figure 20.8[20] for an image of a venous ulcer.

Arterial Ulcers
Arterial ulcers are caused by lack of blood flow and oxygenation to tissues. They typically occur in the distal areas of the body such as the feet, heels, and toes. Arterial ulcers have well-defined borders with a “punched out” appearance where there is a localized lack of blood flow. They are typically painful due to the lack of oxygenation to the area. The wound base may become necrotic (black) due to tissue death from ischemia. Wound dressings must maintain a moist environment, and treatment must include the removal of necrotic tissue. In severe arterial ulcers, vascular surgery may be required to reestablish blood supply to the area.[21] See Figure 20.9[22] for an image of an arterial ulcer on a patient’s foot.

Diabetic Ulcers
Diabetic ulcers are also called neuropathic ulcers because peripheral neuropathy is commonly present in patients with diabetes. Peripheral neuropathy is a medical condition that causes decreased sensation of pain and pressure, especially in the lower extremities. Diabetic ulcers typically develop on the plantar aspect of the feet and toes of a patient with diabetes due to lack of sensation of pressure or injury. See Figure 20.10[23] for an image of a diabetic ulcer. Wound healing is compromised in patients with diabetes due to the disease process. In addition, there is a higher risk of developing an infection that can reach the bone requiring amputation of the area. To prevent diabetic ulcers from occurring, it is vital for nurses to teach meticulous foot care to patients with diabetes and encourage the use of well-fitting shoes.[24]

Pressure Injuries
Pressure injuries are defined as “localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.”[25] Shear occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue. For example, when a patient slides down in bed, the outer skin remains immobile because it remains attached to the sheets due to friction, but deeper tissue attached to the bone moves as the patient slides down. This opposing movement of the outer layer of skin and the underlying tissues causes the capillaries to stretch and tear, which then impacts the blood flow and oxygenation of the surrounding tissues.
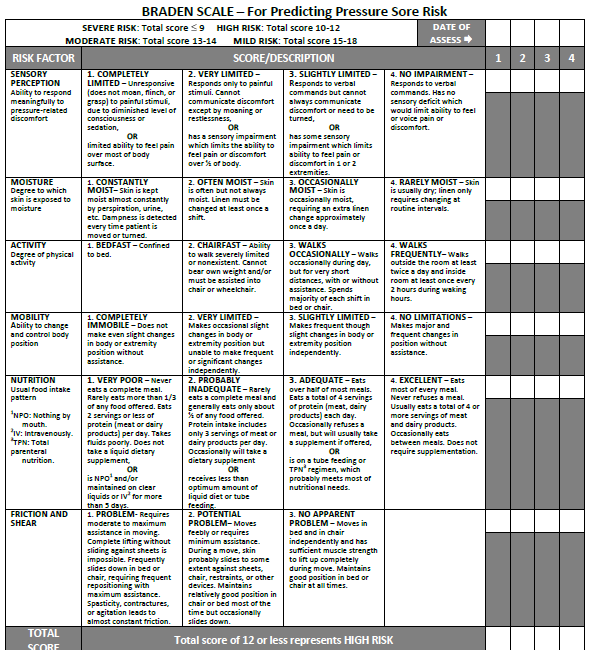
Braden Scale
Several factors place a patient at risk for developing pressure injuries, including nutrition, mobility, sensation, and moisture. The Braden Scale is a tool commonly used in health care to provide an objective assessment of a patient’s risk for developing pressure injuries. See Figure 20.11[26] for an image of a Braden Scale. The six risk factors included on the Braden Scale are sensory perception, moisture, activity, mobility, nutrition, and friction/shear, and these factors are rated on a scale from 1-4 with 1 being “completely limited” to 4 being “no impairment.” The scores from the six categories are added, and the total score indicates a patient’s risk for developing a pressure injury. Ranges of scores indicate mild risk for scores 15-19, moderate risk for scores 13-14, high risk for scores 10-12, and severe risk for scores less than 9. Nurses create care plans using these scores to plan interventions that prevent or treat pressure injuries.
For more information about using the Braden Scale, go to the “Integumentary” chapter of the Open RN Nursing Fundamentals textbook.
Staging
Pressure injuries commonly occur on the sacrum, heels, ischial tuberosity, and coccyx. The 2016 National Pressure Ulcer Advisory Panel (NPUAP) Pressure Injury Staging System now uses the term “pressure injury” instead of pressure ulcer because an injury can occur without an ulcer present. Pressure injuries are staged from 1 through 4 based on the extent of tissue damage. For example, Stage 1 pressure injuries have reddened but intact skin, and Stage 4 pressure injuries have deep, open ulcers affecting underlying tissue and structures such as muscles, ligaments, and tendons. See Figure 20.12[27] for an image of the four stages of pressure injuries.[28] The NPUAP’s definitions of the four stages of pressure injuries are described below:
- Stage 1 pressure injuries are intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred. Nonblanchable erythema is a medical term used to describe skin redness that does not turn white when pressed.
- Stage 2 pressure injuries are partial-thickness loss of skin with exposed dermis. The wound bed is viable and may appear like an intact or ruptured blister. Stage 2 pressure injuries heal by reepithelialization and not by granulation tissue formation.[29]
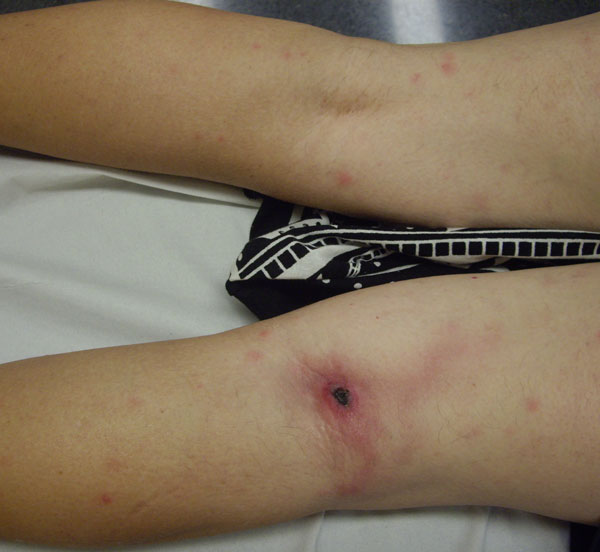
- Stage 3 pressure injuries are full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed. The depth of tissue damage varies by anatomical location. Undermining and tunneling may occur in Stage 3 and 4 pressure injuries. Undermining occurs when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound’s edge. Tunneling refers to passageways underneath the surface of the skin that extend from a wound and can take twists and turns. Slough and eschar may also be present in Stage 3 and 4 pressure injuries. Slough is an inflammatory exudate that is usually light yellow, soft, and moist. Eschar is dark brown/black, dry, thick, and leathery dead tissue. See Figure 20.13 [30] for an image of eschar in the center of the wound. If slough or eschar obscures the wound so that tissue loss cannot be assessed, the pressure injury is referred to as unstageable.[31] In most wounds, slough and eschar must be removed by debridement for healing to occur.
- Stage 4 pressure injuries are full-thickness tissue loss like Stage 3 pressure injuries, but also have exposed cartilage, tendon, ligament, muscle, or bone. Osteomyelitis (bone infection) may be present.[32]

Video Review of Pressure Injuries[33]
Factors Affecting Wound Healing
Multiple factors affect a wound’s ability to heal and are referred to as local and systemic factors. Local factors refer to factors that directly affect the wound, whereas systemic factors refer to the overall health of the patient and their ability to heal. Local factors include localized blood flow and oxygenation of the tissue, the presence of infection or a foreign body, and venous sufficiency. Venous insufficiency is a medical condition where the veins in the legs do not adequately send blood back to the heart, resulting in a pooling of fluids in the legs.[34]
Systemic factors that affect a patient’s ability to heal include nutrition, mobility, stress, diabetes, age, obesity, medications, alcohol use, and smoking.[35] When a nurse is caring for a patient with a wound that is not healing as anticipated, it is important to further assess for the potential impact of these factors:
- Nutrition. Nutritional deficiencies can have a profound impact on healing and must be addressed for chronic wounds to heal. Protein is one of the most important nutritional factors affecting wound healing. For example, in patients with pressure injuries, 30 to 35 kcal/kg of calorie intake with 1.25 to 1.5g/kg of protein and micronutrients supplementation is recommended daily.[36] In addition, vitamin C and zinc deficiency have many roles in wound healing. It is important to collaborate with a dietician to identify and manage nutritional deficiencies when a patient is experiencing poor wound healing.[37]
- Stress. Stress causes an impaired immune response that results in delayed wound healing. Although a patient cannot necessarily control the amount of stress in their life, it is possible to control one’s reaction to stress with healthy coping mechanisms. The nurse can help educate the patient about healthy coping strategies.
- Diabetes. Diabetes causes delayed wound healing due to many factors such as neuropathy, atherosclerosis (a buildup of plaque that obstructs blood flow in the arteries resulting in decreased oxygenation of tissues), a decreased host immune resistance, and increased risk for infection.[38] Read more about neuropathy and diabetic ulcers under the “Types of Wounds” section. Nurses provide vital patient education to patients with diabetes to effectively manage the disease process for improved wound healing.
- Age. Older adults have an altered inflammatory response that can impair wound healing. Nurses can educate patients about the importance of exercise for improved wound healing in older adults.[39]
- Obesity. Obese individuals frequently have wound complications, including infection, dehiscence, hematoma formation, pressure injuries, and venous injuries. Nurses can educate patients about healthy lifestyle choices to reduce obesity in patients with chronic wounds.[40]
- Medications. Medications such as corticosteroids impair wound healing due to reduced formation of granulation tissue.[41] When assessing a chronic wound that is not healing as expected, it is important to consider the side effects of the patient’s medications.
- Alcohol consumption. Research shows that exposure to alcohol impairs wound healing and increases the incidence of infection.[42] Patients with impaired healing of chronic wounds should be educated to avoid alcohol consumption.
- Smoking. Smoking impacts the inflammatory phase of the wound healing process, resulting in poor wound healing and an increased risk of infection.[43] Patients who smoke should be encouraged to stop smoking.
Lab Values Affecting Wound Healing
When a chronic wound is not healing as expected, laboratory test results may provide additional clues regarding the causes of the delayed healing. See Table 20.2 for lab results that offer clues to systemic issues causing delayed wound healing.[44]
Table 20.2 Lab Values Associated with Delayed Wound Healing[45]
| Abnormal Lab Value | Rationale |
|---|---|
| Low hemoglobin | Low hemoglobin indicates less oxygen is transported to the wound site. |
| Elevated white blood cells (WBC) | Increased WBC indicates infection is occurring. |
| Low platelets | Platelets are important during the proliferative phase in the creation of granulation tissue and angiogenesis.[46] |
| Low albumin | Low albumin indicates decreased protein levels. Protein is required for effective wound healing. |
| Elevated blood glucose or hemoglobin A1C | Elevated blood glucose and hemoglobin A1C levels indicate poor management of diabetes mellitus, a disease that impacts wound healing. |
| Elevated serum BUN and creatinine | BUN and creatinine levels are indicators of kidney function, with elevated levels indicating worsening kidney function. Elevated BUN (blood urea nitrogen) levels impact wound healing. |
| Positive wound culture | Positive wound cultures indicate an infection is present and provide additional information including the type and number of bacteria present, as well as identifying antibiotics to which the bacteria is susceptible. The nurse reviews this information when administering antibiotics to ensure the prescribed therapy is effective for the type of bacteria present. |
Wound Complications
In addition to delayed wound healing, several other complications can occur. Three common complications are the development of a hematoma, infection, or dehiscence. These complications should be immediately reported to the health care provider.
Hematoma
A hematoma is an area of blood that collects outside of the larger blood vessels. A hematoma is more severe than ecchymosis (bruising) that occurs when small veins and capillaries under the skin break. The development of a hematoma at a surgical site can lead to infection and incisional dehiscence.[47] See Figure 20.14[48] for an image of a hematoma.

Infection
A break in the skin allows bacteria to enter and begin to multiply. Microbial contamination of wounds can progress from localized infection to systemic infection, sepsis, and subsequent life- and limb-threatening infection. Signs of a localized wound infection include redness, warmth, and tenderness around the wound. Purulent or malodorous drainage may also be present. Signs that a systemic infection is developing and requires urgent medical management include the following:[49]
- Fever over 101 F (38 C)
- Overall malaise (lack of energy and not feeling well)
- Change in level of consciousness/increased confusion
- Increasing or continual pain in the wound
- Expanding redness or swelling around the wound
- Loss of movement or function of the wounded area
Dehiscence
Dehiscence refers to the separation of the edges of a surgical wound. A dehisced wound can appear fully open where the tissue underneath is visible, or it can be partial where just a portion of the wound has torn open. Wound dehiscence is always a risk in a surgical wound, but the risk increases if the patient is obese, smokes, or has other health conditions, such as diabetes, that impact wound healing. Additionally, the location of the wound and the amount of physical activity in that area also increase the chances of wound dehiscence.[50] See Figure 20.15[51] for an image of dehiscence in an abdominal surgical wound in a 50-year-old obese female with a history of smoking and malnutrition.
Wound dehiscence can occur suddenly, especially in abdominal wounds when the patient is coughing or straining. Evisceration is a rare but severe surgical complication when dehiscence occurs and the abdominal organs protrude out of the incision. Signs of impending dehiscence include redness around the wound margins and increasing drainage from the incision. The wound will also likely become increasingly painful. Suture breakage can be a sign that the wound has minor dehiscence or is about to dehisce.[52]
To prevent wound dehiscence, surgical patients must follow all post-op instructions carefully. The patient must move carefully and protect the skin from being pulled around the wound site. They should also avoid tensing the muscles surrounding the wound and avoid heavy lifting as advised.[53]

- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “417 Tissue Repair.jpg” by OpenStax College is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0. ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0. ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Alhajj, Bansal, and Goyal and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- “Ventriculoperitoneal shunt - surgical wound healing - belly - day 12.jpg” by Hansmuller is licensed under CC BY-SA 4.0 ↵
- “Atrophied skin.png” by sansea2 is licensed under CC BY-SA 3.0 ↵
- “Wound closed with surgical sutures.jpg” by Wikip2011 is licensed under CC BY-SA 3.0 ↵
- “Surgical staples1.jpg” by Llywrch is licensed under CC BY-SA 2.5 ↵
- “Incision wound on child's arm, closed with Dermabond.jpg” by ragesoss is licensed under CC BY-SA 3.0 ↵
- “Not quite scissors - TROML - 1366” by Clint Budd is licensed under CC BY 2.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- “Úlceras_antes_da_cirurgia.JPG” by Nini00 is licensed under CC BY-SA 3.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- “Arterial ulcer peripheral vascular disease.jpg” by Jonathan Moore is licensed under CC BY 3.0 ↵
- “Diabetic Planta ulcer.jpg” by Dr. Lorimer is licensed under CC BY-SA 4.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://journals.lww.com/jwocnonline/Fulltext/2016/11000/Revised_National_Pressure_Ulcer_Advisory_Panel.3.aspx ↵
- The Braden Scale, from Prevention Plus, is included on the basis of Fair Use. ↵
- “Wound stage.jpg” by Babagolzadeh is licensed under CC BY-SA 3.0 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- "Inoculation_eschar_Rickettsia_sibirica_mongolitimonae_infection.jpg" by José M. Ramos , Isabel Jado, Sergio Padilla, Mar Masiá, Pedro Anda, and Félix Gutiérrez is licensed under CC0 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- RegisteredNurseRN. (2018, March 7). Pressure ulcers (injuries) stages, prevention, assessment | Stage 1, 2, 3, 4 unstageable NCLEX. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/MDtPik1UE6k ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Grey, J. E., Enoch, S., & Harding, K. G. (2006). Wound assessment. BMJ (Clinical research ed.), 332(7536), 285–288. https://doi.org/10.1136/bmj.332.7536.285 ↵
- Grey, J. E., Enoch, S., & Harding, K. G. (2006). Wound assessment. BMJ (Clinical research ed.), 332(7536), 285–288. https://doi.org/10.1136/bmj.332.7536.285 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah is licensed under CC BY 4.0 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/won.0000000000000281 ↵
- “Ankle swell and internal bleeding” by Glen Bowman is licensed under CC BY-SA 2.0 ↵
- WoundSource. (2016, October 19). 8 signs of wound infection. https://www.woundsource.com/blog/8-signs-wound-infection ↵
- WoundSource. (2018, March 28). Complications in chronic wound healing and associated interventions. https://www.woundsource.com/blog/complications-in-chronic-wound-healing-and-associated-interventions ↵
- “Bogota bag.png” by Suarez-Grau, J. M., Guadalajara Jurado, J. F., Gómez Menchero, J., Bellido Luque, J. A. is licensed under CC BY 4.0 ↵
- WoundSource. (2018, March 28). Complications in chronic wound healing and associated interventions. https://www.woundsource.com/blog/complications-in-chronic-wound-healing-and-associated-interventions ↵
- WoundSource. (2018, March 28). Complications in chronic wound healing and associated interventions. https://www.woundsource.com/blog/complications-in-chronic-wound-healing-and-associated-interventions ↵
When tablets are prescribed for a patient, the dosage of the tablets supplied is often different from the prescription, and nurses must calculate the number of tablets to administer. Dimensional analysis can be used to calculate the number of tablets to administer. Let’s practice using dimensional analysis using a practice problem.
Practice Problem: Tablet Dosage
Jane Doe recently had her prescription changed by her provider from Carvedilol 6.25 mg twice daily to Carvedilol 25 mg once daily. Jane shows you her prescription bottle (see Figure 5.7[1]) and asks, “How many pills can I take every day so I can use up what I have before purchasing another refill?” How many 6.25 mg tablets will you instruct Jane to take based on the new prescribed dose of Carvedilol 25 mg once daily?
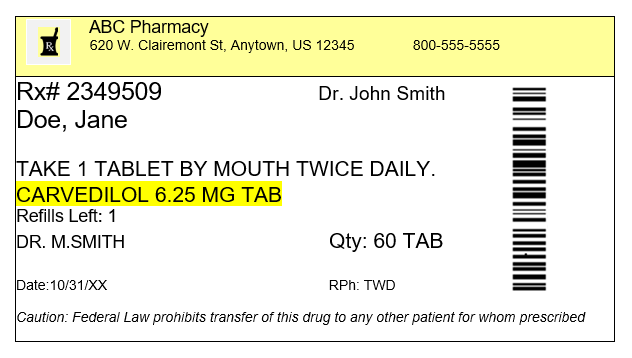
Solve this question by using dimensional analysis.
1. Start by identifying the goal unit for which you are solving, which is a tablet (tab) in this scenario:
[latex]{Tab}~=[/latex]
2. Set up the first fraction with tab in the numerator to match the goal unit. From the prescription bottle, we know that one of the supplied tablets has a concentration of 6.25 mg, so plug in 1 in the numerator and 6.25 mg in the denominator:
[latex]{Tab}~=~\frac{1~tab}{6.25~mg}[/latex]
3. Set up the second fraction with the intent to cross out mg, so place mg in the numerator. By reviewing the prescription, we know the new dosage prescribed is 25 mg, so plug in 25 in the numerator, and 1 in the denominator to cross off units:
[latex]{Tab}~=~\frac{1~tab}{6.25~mg}~x~\frac{25~mg}{1}[/latex]
4. Cross out mg diagonally:
[latex]{Tab}~=~\frac{1~tab}{6.25~\cancel{mg}}~x~\frac{25~\cancel{mg}}[/latex]
5. Multiply across the numerators and denominators, and then divide the final fraction to solve the problem:
[latex]{Tab}~=~\frac{1~tab}{6.25~\cancel{mg}}~x~\frac{25~\cancel{mg}}{1}~=~{4~tabs}[/latex]
Modules 1.5 - 1.7
Please practice tablet dosage calculations with the following interactive learning activity.
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Mr. Jones is a 76-year-old patient admitted to the medical surgical floor with complications of a nonhealing foot ulcer. Mr. Jones has a history of diabetes, hypertension, and COPD. He has a BMI of 29. His daily medications include metformin, Lisinopril, and prednisone. His wife has recently passed away and he lives alone.
- Based upon what is known about Mr. Jones, what factors might be contributing to his nonhealing wound?
- What other factors that influence wound healing might be important to assess with Mr. Jones?
(black) due to tissue death from ischemia.
Use the checklist below to review the steps for completion of “Rectal Medication Administration” using a rectal suppository.[6]
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
Follow Steps 1 through 12 in the "Checklist for Oral Medication Administration."
- If possible, have the patient defecate prior to rectal medication administration.
- Ensure that you have water-soluble lubricant available for medication administration.
- Explain the procedure to the patient. If a patient prefers to self-administer the suppository/enema, give specific instructions to the patient on correct procedure.
- Raise the bed to working height:
- Position the patient on left side with the upper leg flexed over the lower leg toward the waist (Sims position).
- Provide privacy and drape the patient with only the buttocks and anal area exposed.
- Place a drape underneath the patient’s buttocks.
- Apply clean, nonsterile gloves.
- Assess the patient for diarrhea or active rectal bleeding.
- Remove the wrapper from the suppository/tip of enema and lubricate the rounded tip of the suppository and index finger of the dominant hand with lubricant. If administering an enema, lubricate the tip of the enema.
- Separate the buttocks with the nondominant hand and, using the gloved index finger of dominant hand, insert the suppository (rounded tip toward patient) into the rectum toward the umbilicus while having the patient take a deep breath, exhale through the mouth, and relax the anal sphincter. Insert the suppository against the rectal mucosa for optimal absorption, about 3 to 4 inches for an adult and 1 to 2 inches for a child. Do not insert the suppository into feces. If administering an enema, expel the air from the enema and then insert the tip of the enema into the rectum toward the umbilicus while having the patient take a deep breath, exhale through the mouth, and relax the anal sphincter. Roll the plastic bottle from bottom to tip until all solution has entered the rectum and colon. Remove the bottle.
- Monitor the patient for signs of dizziness. Unintended vagal stimulation may occur, resulting in bradycardia in some patients. Be aware that the rectal route may not be suitable for certain cardiac conditions.
- When administering a suppository, ask the patient to remain on side for 5 to 10 minutes.
- When administering an enema, ask the patient to retain the enema until the urge to defecate is strong, usually about 5 to 15 minutes.
- Discard gloves by turning them inside out before disposing them. Discard used supplies as per agency policy and perform hand hygiene.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene.
- Document medication administration and the related assessment findings. Report any unexpected findings according to agency policy.
- Evaluate the patient's response to the medication within the appropriate time frame.

