2.8 Functional Health and Activities of Daily Living
Open Resources for Nursing (Open RN)
Functional health assessment collects data related to the patient’s functioning and their physical and mental capacity to participate in Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs). Activities of Daily Living (ADLs) are daily basic tasks that are fundamental to everyday functioning (e.g., hygiene, elimination, dressing, eating, ambulating/moving). See Figure 2.2[1] for an illustration of ADLs.
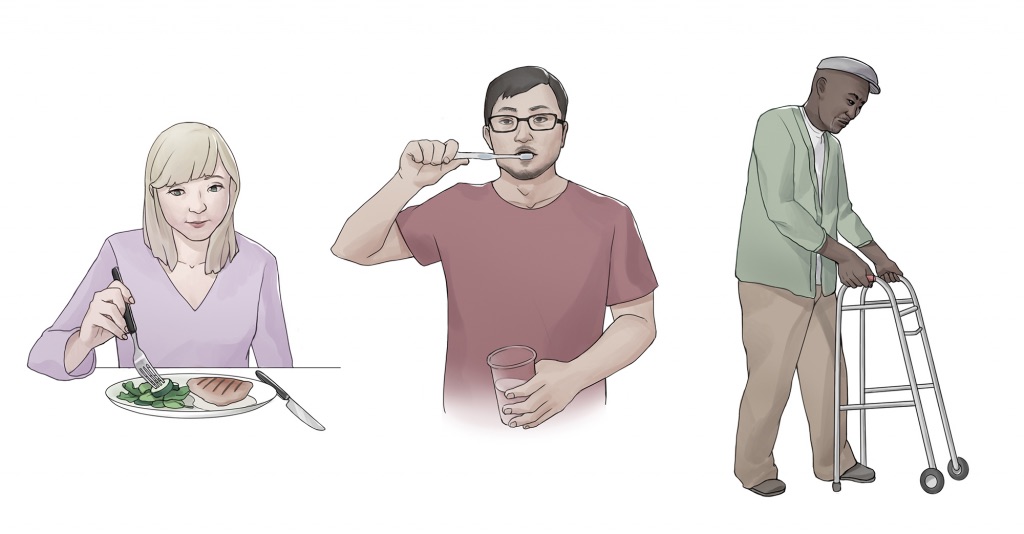
Instrumental Activities of Daily Living (IADL) are more complex daily tasks that allow patients to function independently such as managing finances, paying bills, purchasing and preparing meals, managing one’s household, taking medications, and facilitating transportation. See Figure 2.3[2] for an illustration of IADLs. Assessment of IADLs is particularly important to inquire about with young adults who have just moved into their first place, as well as with older patients with multiple medical conditions and/or disabilities.

Information obtained when assessing functional health provides the nurse a holistic view of a patient’s human response to illness and life conditions. It is helpful to use an assessment framework, such as Gordon’s Functional Health Patterns,[3] to organize interview questions according to evidence-based patterns of human responses. Using this framework provides the patient and their family members an opportunity to identify health-related concerns to the nurse that may require further in-depth assessment. It also verifies patient understanding of conditions so that misperceptions can be clarified. This framework includes the following categories:
- Nutritional-Metabolic: Food and fluid consumption relative to metabolic need
- Elimination: Excretion including bowel and bladder
- Activity-Exercise: Exercise and activity
- Sleep-Rest: Sleep and rest
- Cognitive-Perceptual: Perception and cognition
- Role-Relationship: Roles and relationships
- Sexuality-Reproductive: Reproduction and sexuality
- Coping-Stress Tolerance: Coping and effectiveness of managing stress
- Value-Belief: Values, beliefs, and goals that guide choices and decisions
- Self-Perception and Self-Concept: Self-concept and mood state[4]
- Health Perception-Health Management: A patient’s perception of their health and well-being and how it is managed. This is an umbrella category of all the categories above and underlies performing a health history.
The functional health section can be started by saying, “I would like to ask you some questions about factors that affect your ability to function in your day-to-day life. Feel free to share any health concerns that come to mind during this discussion.” Focused interview questions for each category are included in Table 2.8. Each category is further described below.
Nutrition
The nutritional category includes, but is not limited to, food and fluid intake, usual diet, financial ability to purchase food, time and knowledge to prepare meals, and appetite. This is also an opportune time to engage in health promotion discussions about healthy eating. Be aware of signs for malnutrition and obesity, especially if rapid and excessive weight loss or weight gain have occurred.
Life Span Considerations
When assessing nutritional status, the types of questions asked and the level of detail depend on the developmental age and health of the patient. Family members may also provide important information.
- Infants: Ask parents about using breast milk or formula, amount, frequency, supplements, problems, and introductions of new foods.
- Pregnant women: Include questions about the presence of nausea and vomiting and intake of folic acid, iron, omega-3 fatty acids, vitamin D, and calcium.
- Older adults or patients with disabling illnesses: Inquire about the ability to purchase and cook their food, decreased sense of taste, ability to chew or swallow foods, loss of appetite, and enough fiber and nutrients.[5]
Elimination
Elimination refers to the removal of waste products through the urine and stool. Health care professionals refer to urinating as voiding and stool elimination as having a bowel movement. Familiar terminology may need to be used with patients, such as “pee” and “poop.” Constipation commonly occurs in hospitalized patients, so it is important to assess the date of their last bowel movement and monitor the frequency, color, and consistency of their stool. Assess urine concentration, frequency, and odor, especially if concerned about urinary tract infection, incontinence, or infection. Findings that require further investigation include dysuria (pain or difficulty upon urination), blood in the stool, melena (black, tarry stool), constipation, diarrhea, or excessive laxative use.[6]
Life Span Considerations
When assessing elimination, the types of questions asked and the level of detail depends on the developmental age and health of the patient.
Toddlers: Ask parents or guardians about toilet training. Toilet training takes several months, occurs in several stages, and varies from child to child. It is influenced by culture and depends on physical and emotional readiness, but most children are toilet trained between 18 months and three years.
Older Adults: Constipation and incontinence are common symptoms associated with aging. Additional focused questions may be required to further assess these issues.[7]
Mobility, Activity, and Exercise
Mobility refers to a patient’s ability to move around (e.g., sit up, sit down, stand up, walk). Activity and exercise refer to informal and/or formal activity (e.g., walking, swimming, yoga, strength training). In addition to assessing the amount of exercise, it is also important to assess activity because some people may not engage in exercise but have an active lifestyle (e.g., walk to school or work in a physically demanding job).
Findings that require further investigation include insufficient aerobic exercise and identified risks for falls.[8]
Life Span Considerations
Mobility and activity depend on developmental age and a patient’s health and illness status. With infants, it is important to assess their ability to meet specific developmental milestones at each well-baby visit. Mobility can become problematic for patients who are ill or are aging and can result in self-care deficits. Thus, it is important to assess how a patient’s mobility is affecting their ability to perform ADLs and IADLs.[9]
Sleep and Rest
The sleep and rest category refers to a patient’s pattern of rest and sleep and any associated routines or sleeping medications used. Although it varies for different people and their life circumstances, obtaining eight hours of sleep every night is a general guideline. Findings that require further investigation include disruptive sleep patterns and reliance on sleeping pills or other sedative medications.[10]
Life Span Considerations
Older Adults: Disruption in sleep patterns can be especially troublesome for older adults. Assessing sleep patterns and routines will contribute to collaborative interventions for improved rest.[11]
Cognitive and Perceptual
The cognitive and perceptual category focuses on a person’s ability to collect information from the environment and use it in reasoning and other thought processes. This category includes the following:
- Adequacy of vision, hearing, taste, touch, feeling, and smell
- Any assistive devices used
- Pain level and pain management
- Cognitive functional abilities, such as orientation, memory, reasoning, judgment, and decision-making[12]
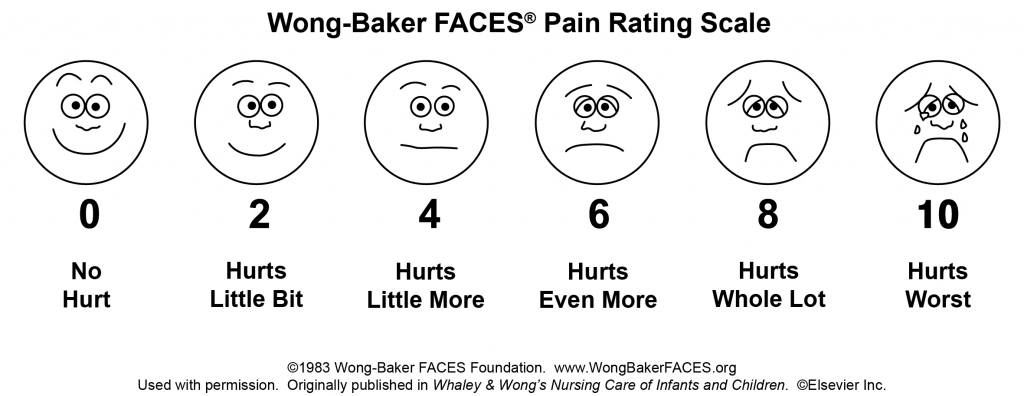
If a patient is experiencing pain, it is important to perform an in-depth assessment using the PQRSTU method described in the “Reason for Seeking Health Care” section of this chapter. It is also helpful to use evidence-based assessment tools when assessing pain, especially for patients who are unable to verbally describe the severity of their pain. See Figure 2.4[13] for an image of the Wong-Baker FACES tool that is commonly used in health care.
Life Span Considerations
Older Adults: Older adults are especially at risk for problems in the cognitive and perceptual category. Be alert for cues that suggest deficits are occurring that have not been previously diagnosed.
Roles – Relationships
Quality of life is greatly influenced by the roles and relationships established with family, friends, and the broader community. Roles often define our identity. For example, a patient may describe themselves as a “mother of an 8 year old.” This category focuses on roles and relationships that may be influenced by health-related factors or may offer support during illness.[14] Findings that require further investigation include indications that a patient does not have any meaningful relationships or has “negative” or abusive relationships in their lives.
Life Span Considerations
Be sensitive to cues when assessing individuals with any of the following characteristics: isolation from family and friends during crisis, language barriers, loss of a significant person or pet, loss of job, significant home care needs, prolonged caregiving, history of abuse, history of substance abuse, or homelessness.[15]
Sexuality – Reproduction
Sexuality and sexual relations are an aspect of health that can be affected by illness, aging, and medication. This category includes a person’s gender identity and sexual orientation, as well as reproductive issues. It involves a combination of emotional connection, physical companionship (holding hands, hugging, kissing) and sexual activity that impact one’s feeling of health.[16]
The Joint Commission has defined terms to use when caring for diverse patients. Gender identity is a person’s basic sense of being male, female, or other gender.[17] Gender expression are characteristics in appearance, personality, and behavior that are culturally defined as masculine or feminine.[18] Sexual orientation is the preferred term used when referring to an individual’s physical and/or emotional attraction to the same and/or opposite gender.[19] LGBT is an acronym standing for the lesbian, gay, bisexual, and transgender population. It is an umbrella term that generally refers to a group of people who are diverse in gender identity and sexual orientation. It is important to provide a safe environment to discuss health issues because the LGBT population experiences higher rates of smoking, alcohol use, substance abuse, HIV and other STD infections, anxiety, depression, suicidal ideation and attempts, and eating disorders as a result of stigma and marginalization.[20]
Life Span Considerations
Although sexuality is frequently portrayed in the media, individuals often consider these topics as private subjects. Use sensitivity when discussing these topics with different age groups across cultural beliefs while maintaining professional boundaries.
Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community.
Coping-Stress Tolerance
Individuals experience stress that can lead to dysfunction if not managed in a healthy manner. Throughout life, healthy and unhealthy coping strategies are learned. Coping strategies are behaviors used to manage anxiety. Effective strategies control anxiety and lead to problem solving but ineffective strategies can lead to abuse of food, tobacco, alcohol, or drugs.[21] Nurses teach and reinforce effective coping strategies.
Substance Use and Abuse
Alcohol, tobacco products, marijuana, and drugs are often used as ineffective coping strategies. It is important to use a nonjudgmental approach when assessing a patient’s use of substances so they do not feel stigmatized. Substance abuse can affect people of all ages. Make a distinction between use and abuse as you assess frequency of use and patterns of behavior. Substance abuse often causes disruption in everyday function (e.g., loss of employment, deterioration of relationships, or precarious living circumstances) because of dependence on a substance. Action is needed if patients indicate that they have a problem with substance use or show signs of dependence, addiction, or binge drinking.[22]
Life Span Considerations
Some individuals are at increased risk for problems with coping strategies and stress management. Be sensitive to cues when assessing individuals with characteristics such as uncertainty in medical diagnosis or prognosis, financial problems, marital problems, poor job fit, or few close friends and family members.[23]
Value-Belief
This category includes values and beliefs that guide decisions about health care and can also provide strength and comfort to individuals. It is common for a person’s spirituality and values to be influenced by religious faith. A value is an accepted principle or standard of an individual or group. A belief is something accepted as true with a sense of certainty. Spirituality is a way of living that comes from a set of values and beliefs that are important to a person. The Joint Commission asks health care professionals to respect patients’ cultural and personal values, beliefs, and preferences and accommodate patients’ rights to religious and other spiritual services.[24] When performing an assessment, use open-ended questions to allow the patient to share values and beliefs they believe are important. For example, ask, “I am interested in your spiritual and religious beliefs and how they relate to your health. Can you share with me any spiritual beliefs or religious practices that are important to you during your stay?”
Self-Perception and Self-Concept
The focus of this category is on the subjective thoughts, feelings, and attitudes of a patient about themself. Self-concept refers to all the knowledge a person has about themself that makes up who they are (i.e., their identity). Self-esteem refers to a person’s self-evaluation of these items as being worthy or unworthy. Body image is a mental picture of one’s body related to appearance and function. It is best to assess these items toward the end of the interview because you will have already collected data that contributes to an understanding of the patient’s self-concept. Factors that influence a patient’s self-concept vary from person to person and include elements of life they value, such as talents, education, accomplishments, family, friends, career, financial status, spirituality, and religion.[25] The self-perception and self-concept category also focuses on feelings and mood states such as happiness, anxiety, hope, power, anger, fear, depression, and control.[26]
Life Span Considerations
Some individuals are at risk for problems with self-perception and self-concept. Be sensitive to cues when assessing individuals with characteristics such as uncertainty regarding a medical diagnosis or surgery, significant personal loss, history of abuse or neglect, loss of body part or function, or history of substance abuse.[27]
Violence and Trauma
There are many types of violence that a person may experience, including neglect or physical, emotional, mental, sexual, or financial abuse. You are legally mandated to report suspected cases of child abuse or neglect, as well as suspected cases of elder abuse. At any time, if you or the patient is in immediate danger, follow agency policy and procedure.
Trauma results from violence or other distressing events in a life. Collaborative intervention with the patient is required when violence and trauma are identified. People respond in different ways to trauma. It is important to use a trauma-informed approach when caring for patients who have experienced trauma. For example, a patient may respond to the traumatic situation in a way that seems unfitting (such as with laughter, ambivalence, or denial). This does not mean the patient is lying but can be a symptom of trauma. To reduce the effects of trauma, it is important to implement collaborative interventions to support patients who have experienced trauma.[28]
Loss of Body Part
A person can have negative feelings or perceptions about the characteristics, function, or limits of a body part as a result of a medical condition, surgery, trauma, or mental condition. Pay attention to cues, such as neglect of a body part or negative comments about a body part, and use open-ended questions to obtain additional information.
Mental Health
Mental health is frequently underscreened and unaddressed in health care. The mental health of all patients should be assessed, even if they appear well or state they have no mental health concerns so that any changes in condition are quickly noticed and treatment implemented. Mental health includes emotional and psychological symptoms that can affect a patient’s day-to-day ability to function. The World Health Organization (2014) defines mental health as “a state of well-being in which every individual realizes their own potential, can cope with normal stresses of life, can work productively and fruitfully, and is able to make a contribution to their community.”[29] Mental illness includes conditions diagnosed by a health care provider, such as depression, anxiety, addiction, schizophrenia, post-traumatic stress disorder, and others. Mental illness can disrupt everyday functioning and affect a person’s employment, education, and relationships.
It is helpful to begin this component of a mental health assessment with a statement such as, “Mental health is an important part of our lives, so I ask all patients about their mental health and any concerns or questions they may have.”[30] Be attentive of critical findings that require intervention. For example, if a patient talks about feeling hopeless or depressed, it is important to screen for suicidal thinking. Begin with an open-ended question, such as, “Have you ever felt like hurting yourself?” If the patient responds with a “Yes,” then progress with specific questions that assess the immediacy and the intensity of the feelings. For example, you may say, “Tell me more about that feeling. Have you been thinking about hurting yourself today? Have you put together a plan to hurt yourself?” When assessing for suicidal thinking, be aware that a patient most at risk is someone who has a specific plan about self-harm and can specify how and when they will do it. They are particularly at risk if planning self-harm within the next 48 hours. The age of the patient is not a factor in this determination of risk. If you believe the patient is at high risk, do not leave the patient alone. Collaborate with them regarding an immediate plan for emergency care.[31]
Health Perception-Health Management
Health perception-health management is an umbrella term encompassing all of the categories described above, as well as environmental health.
Environmental Health
Environmental health refers to the safety of a patient’s physical environment, also called a social determinant of health. Examples of environmental health include, but are not limited to, exposure to violence in the home or community; air pollution; and availability of grocery stores, health care providers, and public transportation. Findings that require further investigation include a patient living in unsafe environments.[32]
See Table 2.8 for sample focused questions for all categories related to functional health.[33]
Table 2.8 Focused Interview Questions for Functional Health Categories[34]
Begin this section by saying, “I would like to ask you some questions about factors that affect your ability to function in your day-to-day life. Feel free to share any health concerns that come to mind during this discussion.”
| Category | Focused Questions |
|---|---|
| Nutrition | Tell me about your diet.
What foods do you usually eat? What fluids do you usually drink every day? What have you eaten in the last 24 hours? Is this typical of your usual eating pattern? Tell me about your appetite. Have you had any changes in your appetite? Do you have any goals related to your nutrition? Do you have any financial concerns about purchasing food? Are you able to prepare the meals you want to eat? |
| Elimination | When was your last bowel movement?
Do you have any problems with constipation, diarrhea, or incontinence? Do you take laxatives or stool softeners? Do you have any problems urinating, such as frequent urination or burning on urination? Do you ever experience leaking or dribbling of urine? |
| Mobility, Activity, and Exercise | Tell me about your ability to move around.
Do you have any problems sitting up, standing up, or walking? Do you use any mobility aids (e.g., cane, walker, wheelchair)? Tell me about the activity and/or exercise in which you engage. What type? How frequent? For how long? |
| Sleep and Rest | Tell me about your sleep routine. How many hours of sleep do you usually get?
Do you feel rested when you awaken? Do you do anything to wind down before you go to bed (e.g., watch TV, read)? Do you take any sleeping medication? Do you take any naps during the day? |
| Cognitive and Perceptual | Are you having any pain?
Note: If present, use the PQRSTU method to further assess pain. Are you having any issues with seeing, hearing, smelling, tasting, or feeling things? Have you noticed any changes in memory or problems concentrating? Have you noticed any changes in the ability to make decisions? What is the easiest way for you to learn (e.g., written materials, explanations, or learning-by-doing)? |
| Roles and Relationships | Tell me about the most influential relationships in your life with family and friends.
How do these relationships influence your day-to-day life, health, and illness? Who are the people with whom you talk to when you require support or are struggling in your life? Do you have family or others dependent on you? Have you had any recent losses of someone important to you, a pet, or a job? Do you feel safe in your current relationship? |
| Sexuality-Reproduction | The expression of love and caring in a sexual relationship and creation of family are often important aspects in a person’s life. Do you have any concerns about your sexual health?
Tell me about the ways that you ensure your safety when engaging in intimate and sexual practices. |
| Coping-Stress | Tell me about the stress in your life.
Have you experienced a recent loss in your life that has impacted you? How do you cope with stress? |
| Values-Belief | I am interested in your spiritual and religious beliefs and how they relate to your health. Can you share with me any spiritual beliefs or religious practices that are important to you? |
| Self-Perception and Self-Concept |
Tell me what makes you who you are. How would you describe yourself? Have you noticed any changes in how you view your body or the things you can do? Are these a problem for you? Have you found yourself feeling sad, angry, fearful, or anxious? What helps you to feel better when this happens? Have you ever used any tobacco products (e.g., cigarettes, pipes, vaporizers, hookah)? If so, how much? How much alcohol do you drink every week? Have you used cannabis products? If so, how often do you use them? Have you ever used drugs or prescription drugs that were not prescribed for you? If so, what type? Have you ever felt you had a problem with any of these substances because they affected your daily life? If so, tell me more. Do you want to quit any of these substances? Many patients have experienced violence or trauma in their lives. Have you experienced any violence or trauma in your life? How has it affected you? Would you like to talk with someone about it?
|
| Health Perception – Health Management |
Tell me about how you take care of yourself and manage your home. Have you had any falls in the past six months? Do you have enough finances to pay your bills and purchase food, medications, and other needed items? Do you have any current or future concerns about being able to function independently? Tell me about where you live. Do you have any concerns about safety in your home or neighborhood? Tell me about any factors in your environment that may affect your health. Do you have any concerns about how your environment is affecting your health? |
- "ADL-1024x534.jpg" by unknown is licensed under CC BY-SA 4.0. Access for free at https://ecampusontario.pressbooks.pub/healthassessment/chapter/functional-health/ ↵
- "iADL-1024x494.jpg" by unknown is licensed under CC BY-SA 4.0. Access for free at https://ecampusontario.pressbooks.pub/healthassessment/chapter/functional-health/ ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F.A. Davis Company ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0. ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F.A. Davis Company. ↵
- Wong-Baker FACES Foundation (2020). Wong-Baker FACES® Pain Rating Scale. ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- The Joint Commission. (2011). Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/health-equity/lgbtfieldguide_web_linked_verpdf.pdf downloaded from https://www.jointcommission.org/resources/patient-safety-topics/health-equity/#t=_Tab_StandardsFAQs&sort=relevancy ↵
- The Joint Commission. (2011). Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/health-equity/lgbtfieldguide_web_linked_verpdf.pdf downloaded from https://www.jointcommission.org/resources/patient-safety-topics/health-equity/#t=_Tab_StandardsFAQs&sort=relevancy ↵
- The Joint Commission. (2011). Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/health-equity/lgbtfieldguide_web_linked_verpdf.pdf downloaded from https://www.jointcommission.org/resources/patient-safety-topics/health-equity/#t=_Tab_StandardsFAQs&sort=relevancy ↵
- The Joint Commission. (2011). Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/health-equity/lgbtfieldguide_web_linked_verpdf.pdf downloaded from https://www.jointcommission.org/resources/patient-safety-topics/health-equity/#t=_Tab_StandardsFAQs&sort=relevancy ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- The Joint Commission. (2018). The source, 16(1). https://store.jcrinc.com/assets/1/14/ts_16_2018_01.pdf ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0. ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
The function of receiving information about the environment. The major senses are taste, smell, touch, sight, and hearing.
Drooping of the eyelid.
Double vision (i.e., seeing two images of a single object).
Difficulty speaking.
A swishing sound heard upon auscultation.
A decreased level of consciousness with a score of less than 8 on the Glasgow Coma Scale.
Nostril openings into the nasal cavity.
The action of both eyes moving inward as they focus on a close object using near vision.
The ability of the eye to adjust from near vision to far vision. Pupils constrict at near vision and dilate at far vision.
Lower jaw bone.
A reflex demonstrated by the fanning of toes with the great toe pointed toward the back (dorsum) of the foot. In adults, the Babinski response is considered abnormal and an indication of motor neuron disease.
The bony socket that houses the eyeball and muscles that move the eyeball.
The partial or complete loss of strength, movement, or control of a muscle or group of muscles within a body part that can be caused by brain or spinal injury.
Bone that forms the upper jaw and supports the upper teeth.
Eight bones that protect the brain in the cranial cavity.
A tube lined with mucous membrane that begins at the nasal cavity and is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx.
The middle region of the pharynx bordered superiorly by the nasopharynx and anteriorly by the oral cavity that is a passageway for air and ingested material.

