7.2 Head and Neck Basic Concepts
Open Resources for Nursing (Open RN)
To perform and document an accurate assessment of the head and neck, it is important to understand their basic anatomy and physiology.
Anatomy
Skull
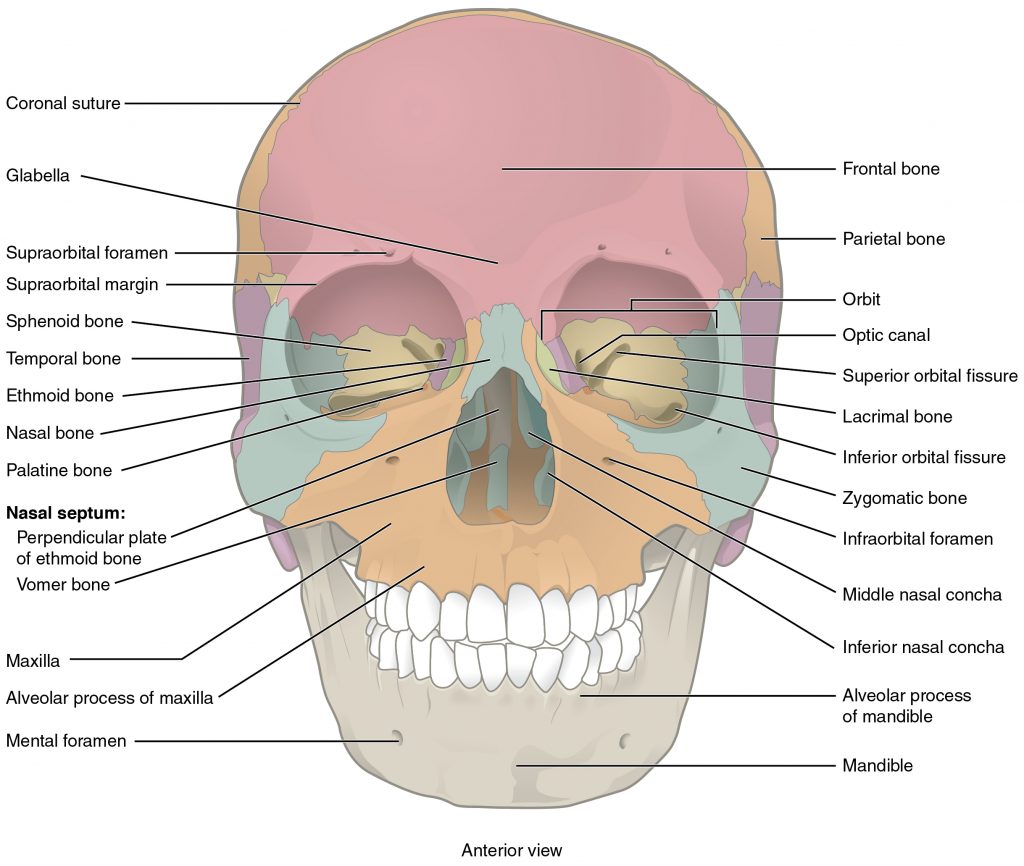
The anterior skull consists of facial bones that provide the bony support for the eyes and structures of the face. This anterior view of the skull is dominated by the openings of the orbits, the nasal cavity, and the upper and lower jaws. See Figure 7.1[1] for an illustration of the skull. The orbit is the bony socket that houses the eyeball and the muscles that move the eyeball. Inside the nasal area of the skull, the nasal cavity is divided into halves by the nasal septum that consists of both bone and cartilage components. The mandible forms the lower jaw and is the only movable bone in the skull. The maxilla forms the upper jaw and supports the upper teeth.[2]
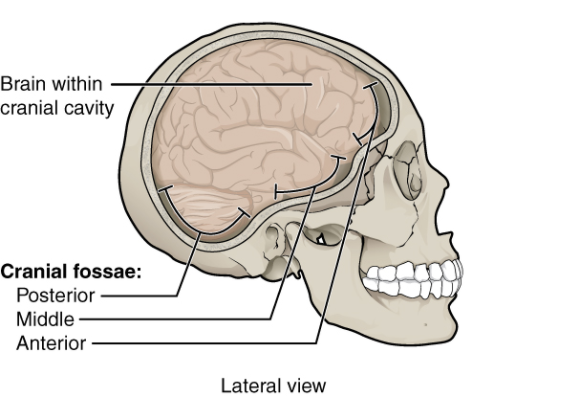
The brain case surrounds and protects the brain that occupies the cranial cavity. See Figure 7.2[3] for an image of the brain within the cranial cavity. The brain case consists of eight bones, including the paired parietal and temporal bones plus the unpaired frontal, occipital, sphenoid, and ethmoid bones.[4]
A suture is an interlocking joint between adjacent bones of the skull and is filled with dense, fibrous connective tissue that unites the bones. In a newborn infant, the pressure from vaginal delivery compresses the head and causes the bony plates to overlap at the sutures, creating a small ridge. Over the next few days, the head expands, the overlapping disappears, and the edges of the bony plates meet edge to edge. This is the normal position for the remainder of the life span and the sutures become immobile.
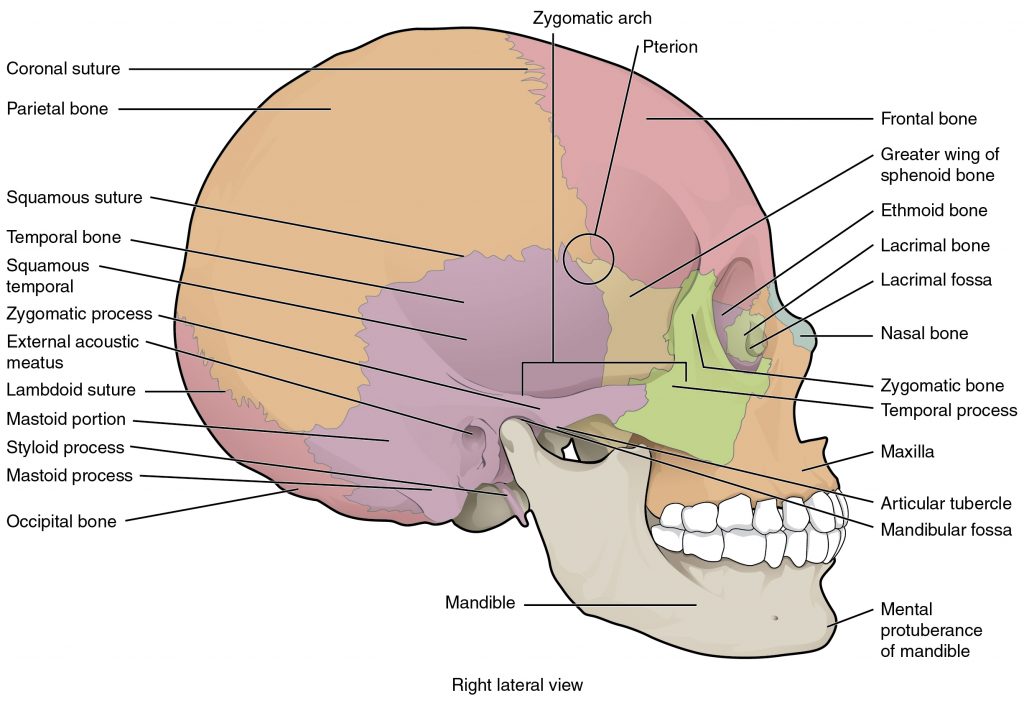
See Figure 7.3[5] for an illustration of two of the sutures, the coronal and squamous sutures, on the lateral view of the head. The coronal suture is seen on the top of the skull. It runs from side to side across the skull and joins the frontal bone to the right and left parietal bones. The squamous suture is located on the lateral side of the skull. It unites the squamous portion of the temporal bone with the parietal bone. At the intersection of the coronal and squamous sutures is the pterion, a small, capital H-shaped suture line region that unites the frontal bone, parietal bone, temporal bone, and greater wing of the sphenoid bone. The pterion is an important clinical landmark because located immediately under it, inside the skull, is a major branch of an artery that supplies the brain. A strong blow to this region can fracture the bones around the pterion. If the underlying artery is damaged, bleeding can cause the formation of a collection of blood, called a hematoma, between the brain and interior of the skull, which can be life-threatening.[6]
Paranasal Sinuses
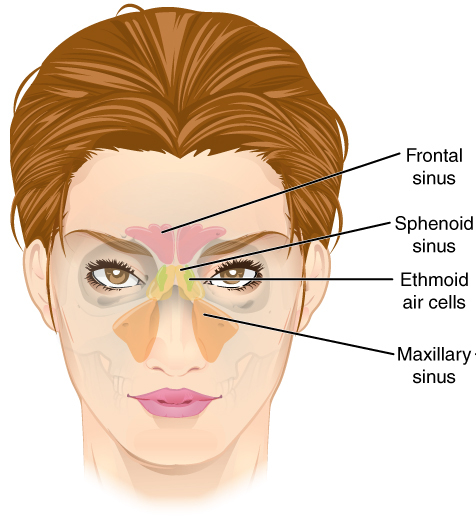
The paranasal sinuses are hollow, air-filled spaces located within the skull. See Figure 7.4[7] for an illustration of the sinuses. The sinuses connect with the nasal cavity and are lined with nasal mucosa. They reduce bone mass, lightening the skull, and also add resonance to the voice. When a person has a cold or sinus congestion, the mucosa swells and produces excess mucus that often obstructs the narrow passageways between the sinuses and the nasal cavity. The resulting pressure produces pain and discomfort.[8]
Each of the paranasal sinuses is named for the skull bone that it occupies. The frontal sinus is located just above the eyebrows within the frontal bone. The largest sinus, the maxillary sinus, is paired and located within the right and left maxillary bones just below the orbits. The maxillary sinuses are most commonly involved during sinus infections. The sphenoid sinus is a single, midline sinus located within the body of the sphenoid bone. The lateral aspects of the ethmoid bone contain multiple small spaces separated by very thin, bony walls. Each of these spaces is called an ethmoid air cell.
Anatomy of Nose, Pharynx, and Mouth
See Figure 7.5[9] to review the anatomy of the head and neck. The major entrance and exit for the respiratory system is through the nose. The bridge of the nose consists of bone, but the protruding portion of the nose is composed of cartilage. The nares are the nostril openings that open into the nasal cavity and are separated into left and right sections by the nasal septum. The floor of the nasal cavity is composed of the palate. The hard palate is located at the anterior region of the nasal cavity and is composed of bone. The soft palate is located at the posterior portion of the nasal cavity and consists of muscle tissue. The uvula is a small, teardrop-shaped structure located at the apex of the soft palate. Both the uvula and soft palate move like a pendulum during swallowing, swinging upward to close off the nasopharynx and prevent ingested materials from entering the nasal cavity.[10]
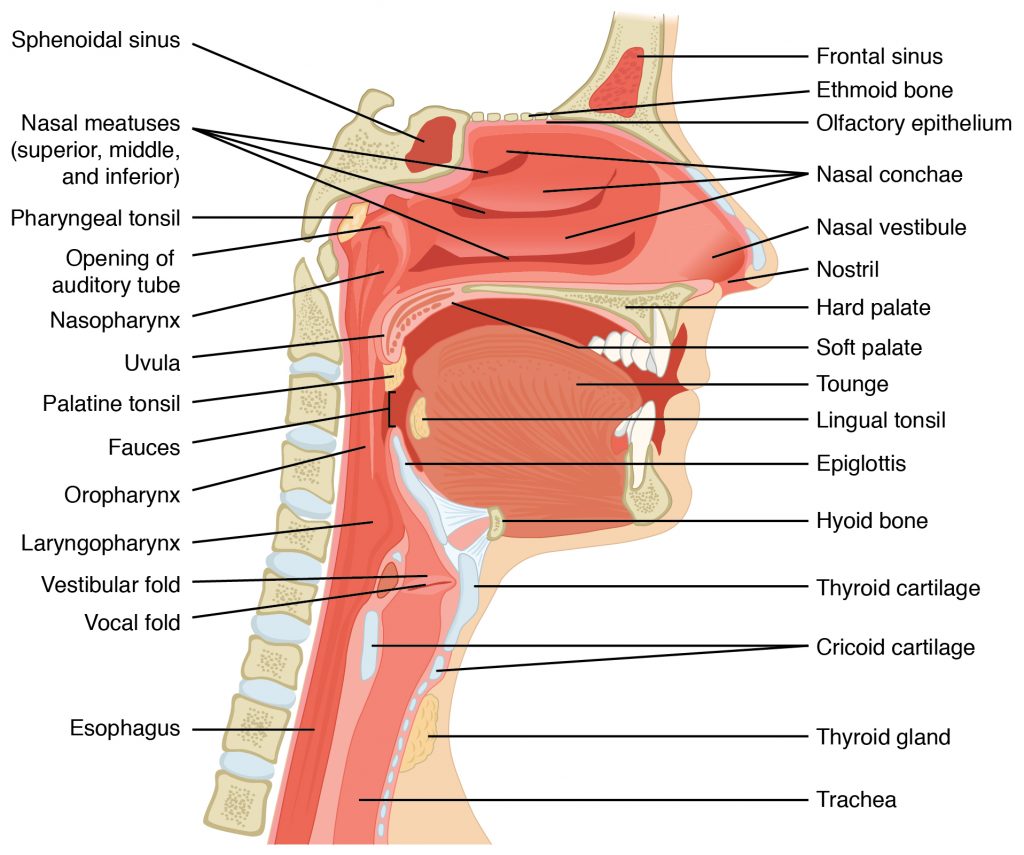
As air is inhaled through the nose, the paranasal sinuses warm and humidify the incoming air as it moves into the pharynx. The pharynx is a tube-lined mucous membrane that begins at the nasal cavity and is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx.[11]
The nasopharynx serves only as an airway. At the top of the nasopharynx is the pharyngeal tonsil, commonly referred to as the adenoids. Adenoids are lymphoid tissue that trap and destroy invading pathogens that enter during inhalation. They are large in children but tend to regress with age and may even disappear.[12]
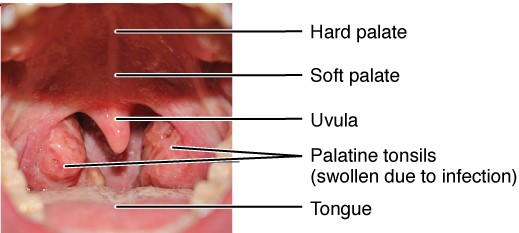
The oropharynx is a passageway for both air and food. The oropharynx is bordered superiorly by the nasopharynx and anteriorly by the oral cavity. The oropharynx contains two sets of tonsils, the palatine and lingual tonsils. The palatine tonsil is located laterally in the oropharynx, and the lingual tonsil is located at the base of the tongue. Similar to the pharyngeal tonsil, the palatine and lingual tonsils are composed of lymphoid tissue and trap and destroy pathogens entering the body through the oral or nasal cavities. See Figure 7.6[13] for an image of the oral cavity and oropharynx with enlarged palatine tonsils.
The laryngopharynx is inferior to the oropharynx and posterior to the larynx. It continues the route for ingested material and air until its inferior end where the digestive and respiratory systems diverge. Anteriorly, the laryngopharynx opens into the larynx and posteriorly, it enters the esophagus that leads to the stomach. The larynx connects the pharynx to the trachea and helps regulate the volume of air that enters and leaves the lungs. It also contains the vocal cords that vibrate as air passes over them to produce the sound of a person’s voice. The trachea extends from the larynx to the lungs. The epiglottis is a flexible piece of cartilage that covers the opening of the trachea during swallowing to prevent ingested material from entering the trachea.[14]
Muscles and Nerves of the Head and Neck
Facial Muscles
Several nerves innervate the facial muscles to create facial expressions. See Figure 7.7[15] for an illustration of nerves innervating facial muscles. These nerves and muscles are tested during a cranial nerve exam. See more information about performing a cranial nerve exam in the “Neurological Assessment” chapter.
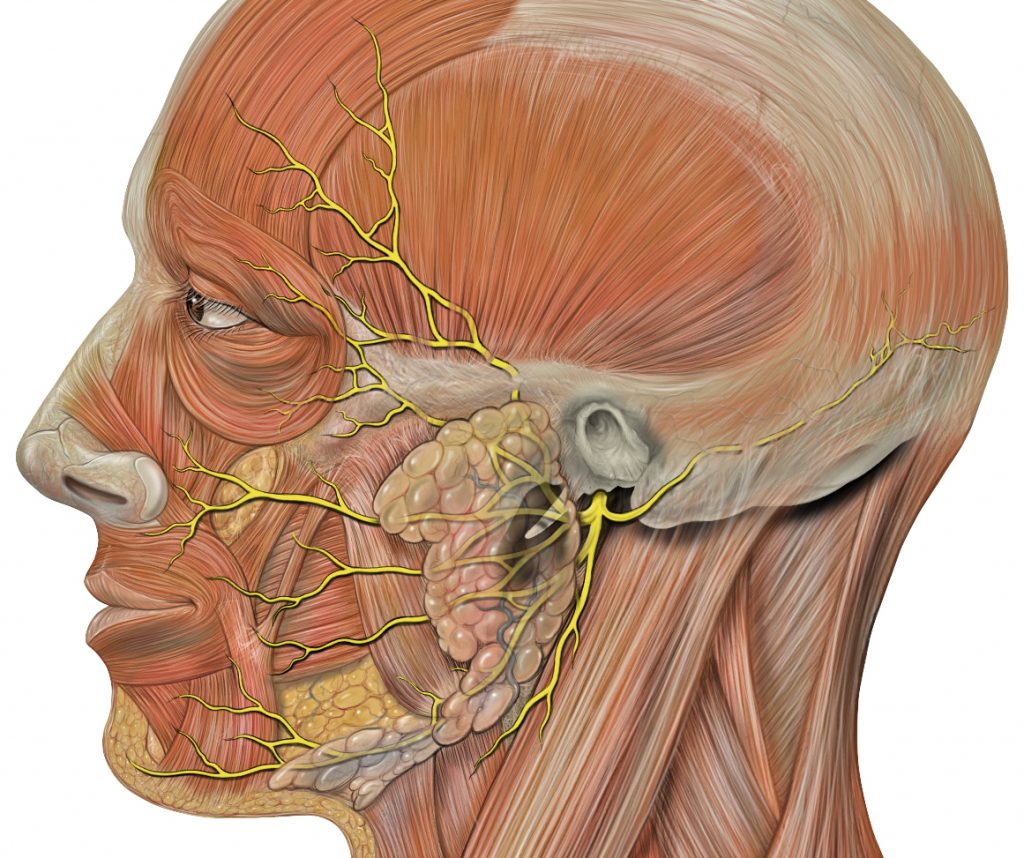
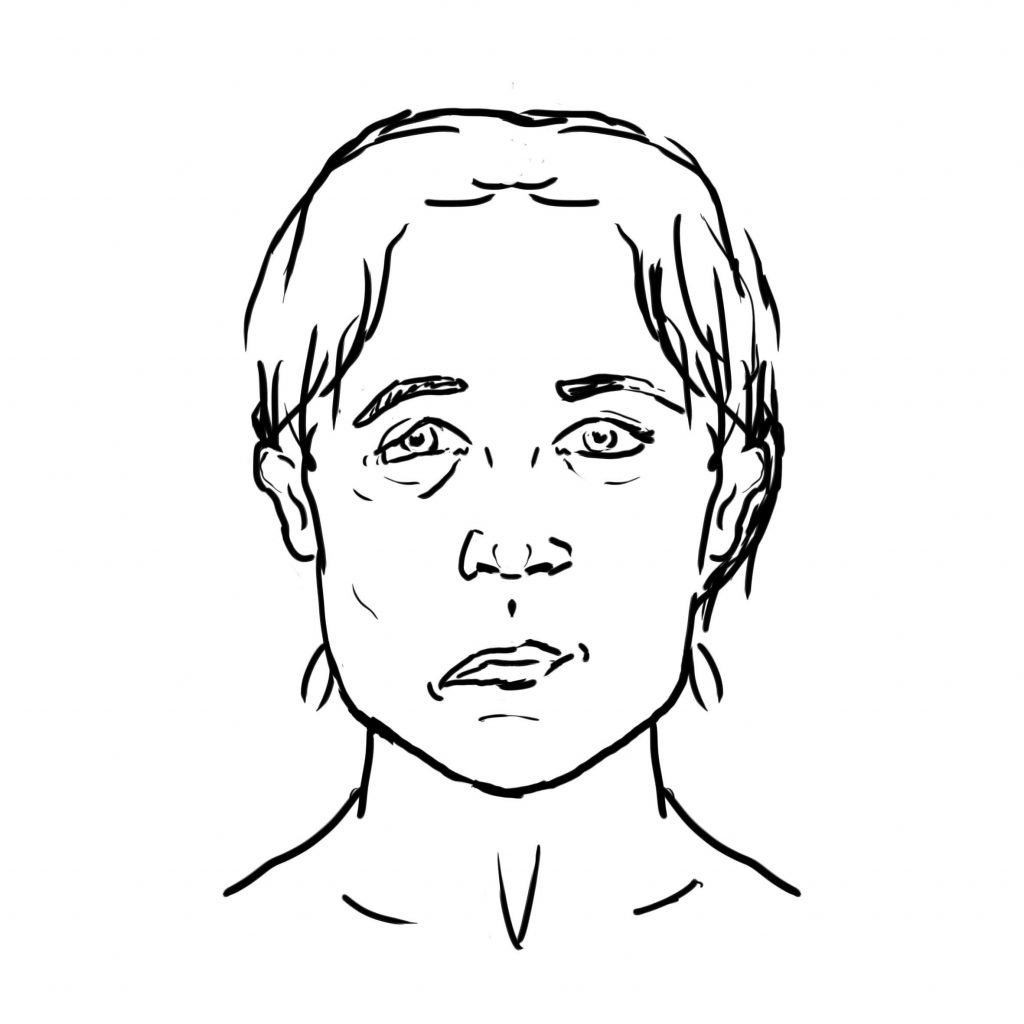
When a patient is experiencing a cerebrovascular accident (i.e., stroke), it is common for facial drooping to occur. Facial drooping is an asymmetrical facial expression that occurs due to damage of the nerve innervating a specific part of the face. See Figure 7.8[16] for an image of facial drooping occurring on the patient’s right side of their face.
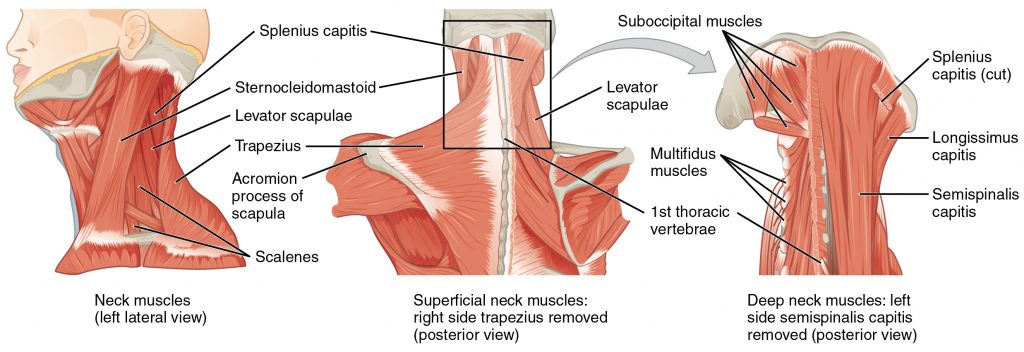
Neck Muscles
The muscles of the anterior neck assist in swallowing and speech by controlling the positions of the larynx and the hyoid bone, a horseshoe-shaped bone that functions as a solid foundation on which the tongue can move. The head, attached to the top of the vertebral column, is balanced, moved, and rotated by the neck muscles. When these muscles act unilaterally, the head rotates. When they contract bilaterally, the head flexes or extends. The major muscle that laterally flexes and rotates the head is the sternocleidomastoid. The trapezius muscle elevates the shoulders (shrugging), pulls the shoulder blades together, and tilts the head backwards. See Figure 7.9[17] for an illustration of the sternocleidomastoid and trapezius muscles.[18]Both of these muscles are tested during a cranial nerve assessment. See more information about cranial nerve assessment in the “Neurological Assessment” chapter.
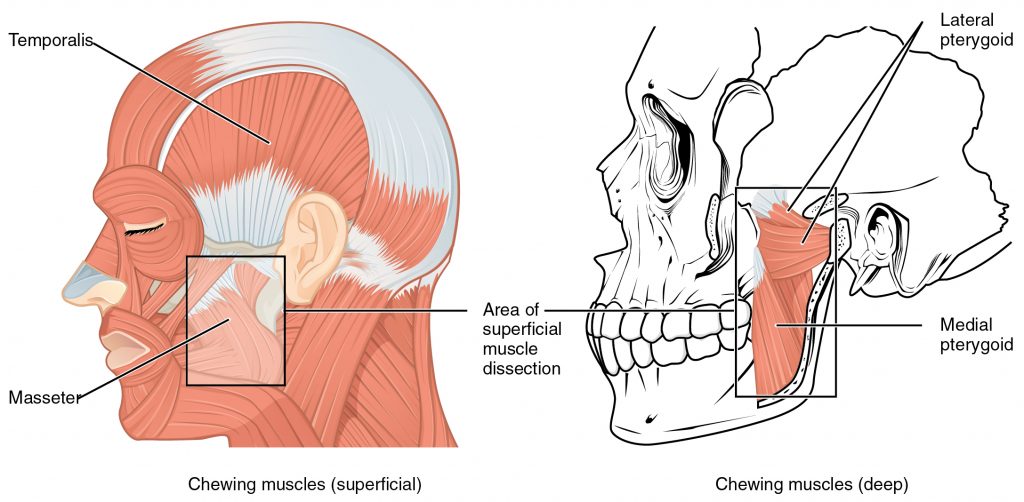
Jaw Muscles
The masseter muscle is the main muscle used for chewing because it elevates the mandible (lower jaw) to close the mouth. It is assisted by the temporalis muscle that retracts the mandible. The temporalis muscle can be felt moving by placing fingers on the patient’s temple as they chew. See Figure 7.10[19] for an illustration of the masseter and temporalis muscles.[20]
Tongue Muscles
Muscles of the tongue are necessary for chewing, swallowing, and speech. Because it is so moveable, the tongue facilitates complex speech patterns and sounds.[21]
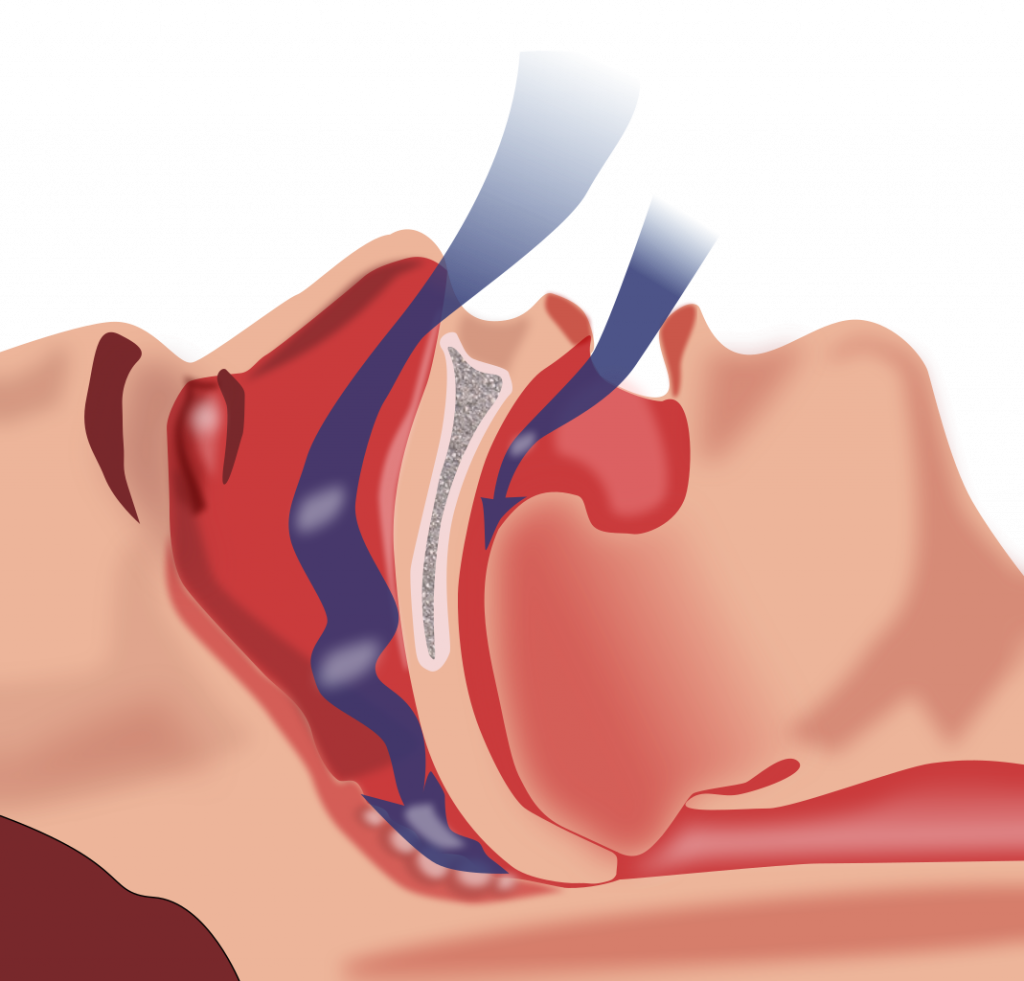
Airway and Unconsciousness
When a patient becomes unconscious and is lying supine, the tongue often moves backwards and blocks the airway. This is why it is important to open the airway when performing CPR by using a chin-thrust maneuver. See Figure 7.11[22] for an image of the tongue blocking the airway. In a similar manner, when a patient is administered general anesthesia during surgery, the tongue relaxes and can block the airway. For this reason, endotracheal intubation is performed during surgery with general anesthesia by placing a tube into the trachea to maintain an open airway to the lungs. After surgery, patients often report a sore or scratchy throat for a few days due to the endotracheal intubation.[23]

Swallowing
Swallowing is a complex process that uses 50 pairs of muscles and many nerves to receive food in the mouth, prepare it, and move it from the mouth to the stomach. Swallowing occurs in three stages. During the first stage, called the oral phase, the tongue collects the food or liquid and makes it ready for swallowing. The tongue and jaw move solid food around in the mouth so it can be chewed and made the right size and texture to swallow by mixing food with saliva. The second stage begins when the tongue pushes the food or liquid to the back of the mouth. This triggers a swallowing response that passes the food through the pharynx. During this phase, called the pharyngeal phase, the epiglottis closes off the larynx and breathing stops to prevent food or liquid from entering the airway and lungs. The third stage begins when food or liquid enters the esophagus and it is carried to the stomach. The passage through the esophagus, called the esophageal phase, usually occurs in about three seconds.[24]
View the following video from Medline Plus on the Swallowing Process:
Dysphagia is the medical term for swallowing difficulties that occur when there is a problem with the nerves or structures involved in the swallowing process.[26] Nurses are often the first to notice signs of dysphagia in their patients that can occur due to a multitude of medical conditions such as a stroke, head injury, or dementia. For more information about the symptoms, screening, and treatment for dysphagia, go to the “Common Conditions of the Head and Neck” section.
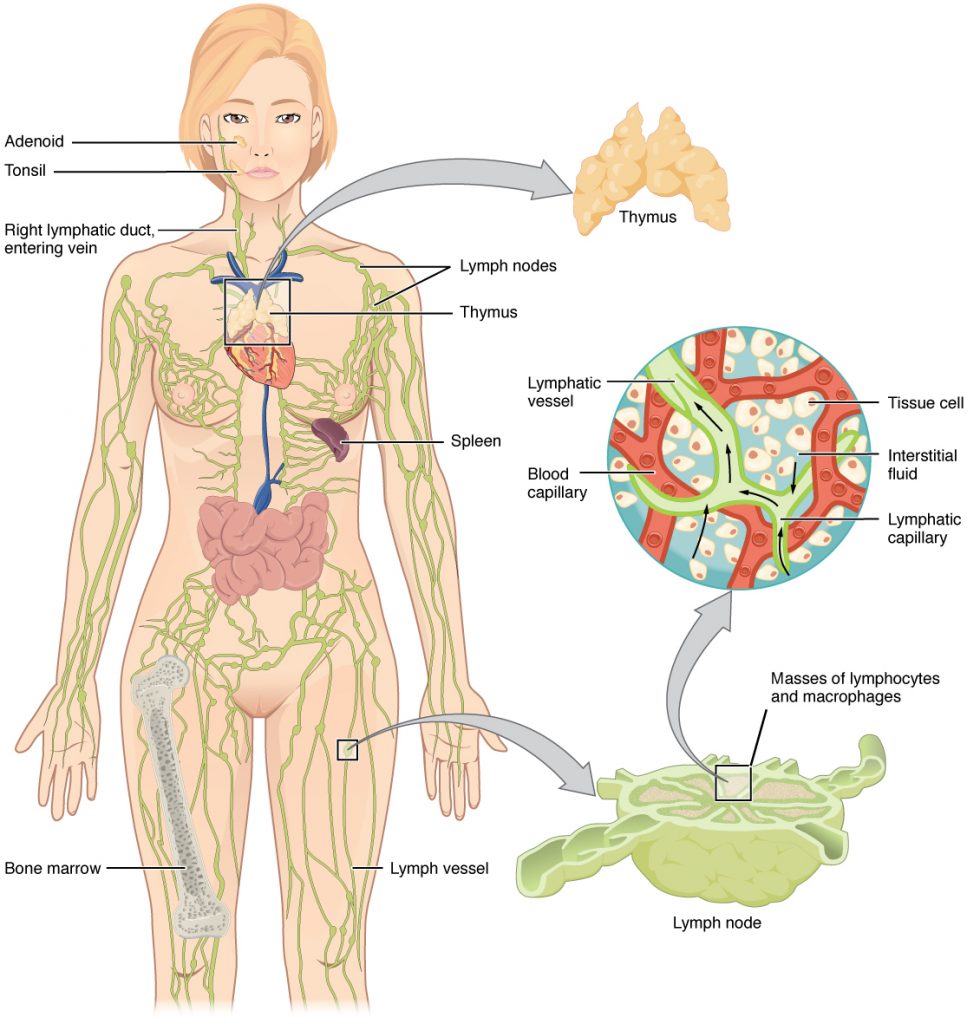
Lymphatic System
The lymphatic system is the system of vessels, cells, and organs that carries excess interstitial fluid to the bloodstream and filters pathogens from the blood through lymph nodes found near the neck, armpits, chest, abdomen, and groin. See Figure 7.12[27] and Figure 7.13[28] for an illustration of the lymph nodes found in the head and neck regions. When a person is fighting off an infection, the lymph nodes in that region become enlarged, indicating an active immune response to infection.[29]
![]“Cervical lymph nodes and level.png” by Mikael Häggström, M.D. is licensed under CC0 1.0 Illustration of lymph nodes in head and neck, with labels](https://nicoletcollege.pressbooks.pub/app/uploads/sites/54/2022/04/Cervical_lymph_nodes_and_levels-1024x551.png)
- “704 Skull -01.jpg” by OpenStax College is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/7-2-the-skull ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is derivative of “727_Cranial_Fossae.jpg” by OpenStax and is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/7-2-the-skull ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “705 Lateral View of Skull-01.jpg” by OpenStax is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/7-2-the-skull ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Paranasal Sinuses ant.jpg” by OpenStax is licensed under CC BY-SA 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/7-2-the-skull ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- "2303 Anatomy of Nose-Pharynx-Mouth-Larynx.jpg” by OpenStax is licensed CC BY 3.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of “2209 Location and Histology of Tonsils.jpg” by OpenStax and is licensed under CC BY 3.0 Access for free at https://openstax.org/books/anatomy-and-physiology/pages/21-1-anatomy-of-the-lymphatic-and-immune-systems ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Head facial nerve branches.jpg” by Patrick J. Lynch, medical illustrator is licensed under CC BY 2.5 ↵
- “Stroke-facial-droop.jpg” by Another-anon-artist-234 is licensed under CC0 1.0 ↵
- “1111 Posterior and Side Views of the Next.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/11-3-axial-muscles-of-the-head-neck-and-back. ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “1108 Muscle that Move the Lower Jaw.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/11-3-axial-muscles-of-the-head-neck-and-back ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Airway closed in an unconscious patient because the head inflexed forward.jpg” by Dr. Lorimer is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- National Institute on Deafness and Other Communication Disorders. (2017, March 6). Dysphagia. https://www.nidcd.nih.gov/health/dysphagia ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M. Inc.; c1997-2021. Swallowing; [Video]. [updated 2019, July 11]. https://medlineplus.gov/ency/anatomyvideos/000126.htm ↵
- National Institute on Deafness and Other Communication Disorders. (2017, March 6). Dysphagia. https://www.nidcd.nih.gov/health/dysphagia ↵
- “2201 Anatomy of the Lymphatic System.jpg” by OpenStax College is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/21-1-anatomy-of-the-lymphatic-and-immune-systems ↵
- “Cervical lymph nodes and level.png” by Mikael Häggström, M.D. is licensed under CC0 1.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
Wound healing that occurs when the edges of a wound cannot be approximated (brought together), so the wound fills in from the bottom up by the production of granulation tissue.
Wound healing that occurs when a wound must remain open or has been reopened, often due to severe infection.
Wounds caused by mechanical forces, typically in the nonelastic skin of older adults.
Ulcers caused by the pooling of fluid in the veins of the lower legs when the valves are not working properly, causing fluid to seep out, macerate the skin, and cause an ulcer.
Ulcers caused by lack of blood flow and oxygenation to tissues and typically occur in the distal areas of the body such as the feet, heels, and toes.
Wound drainage that is clear, thin, watery plasma.
(black) due to tissue death from ischemia.
Ulcers that typically develop on the plantar aspect of the feet and toes of patients with diabetes due to lack of sensation of pressure or injury.
Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.
A mechanical force that occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue.
Inflammatory exudate that is light yellow, soft, and moist and must be removed for wound healing to occur.
If slough or eschar obscures the wound so that tissue loss cannot be assessed.
A medical condition where the veins in the legs do not adequately send blood back to the heart, resulting in a pooling of fluids in the legs that can cause venous ulcers.
Wound drainage that is fresh bleeding.
Wound exudate contains serous drainage with small amounts of blood present.
The separation of the edges of a surgical wound.
The skin around the outer edges of a wound.
An area of hardened tissue.
The removal of non-viable tissue in a wound.
A device used with special foam dressings and suctioning to remove fluid and decrease air pressure around a wound to assist in healing.
Devices that provide a fine mist using oxygen or compressed air to transport the medication from a nebulizer cup into the mouth and into the lungs as the patient breathes normally through a mask or pipe device
When assessing a patient’s oxygenation status, it is important for the nurse to have an understanding of the underlying structures of the respiratory system to best understand their assessment findings. Visit the “Respiratory Assessment" chapter for more information about the structures of the respiratory system.
Video Review for Oxygenation Basics
View the TED-Ed Oxygen's Journey video on YouTube[1]
Breathing Mechanics[2]
Gas Exchange[3]
Carbon Dioxide Transport[4]
Assessing Oxygenation Status
A patient’s oxygenation status is routinely assessed using pulse oximetry, referred to as SpO2. SpO2 is an estimated oxygenation level based on the saturation of hemoglobin measured by a pulse oximeter. Because the majority of oxygen carried in the blood is attached to hemoglobin within the red blood cell, SpO2 estimates how much hemoglobin is “saturated” with oxygen. The target range of SpO2 for an adult is 94-98%.[5] For patients with chronic respiratory conditions, such as COPD, the target range for SpO2 is often lower at 88% to 92%. Although SpO2 is an efficient, noninvasive method to assess a patient’s oxygenation status, it is an estimate and not always accurate. For example, if a patient is severely anemic and has a decreased level of hemoglobin in the blood, the SpO2 reading is affected. Decreased peripheral circulation can also cause a misleading low SpO2 level.
A more specific measurement of oxygen and carbon dioxide in the blood is obtained through an arterial blood gas (ABG). ABG results are often obtained for patients who have deteriorating or unstable respiratory status requiring urgent and emergency treatment. An ABG is a blood sample that is typically drawn from the radial artery by a respiratory therapist, emergency or critical care nurse, or health care provider. ABG results evaluate oxygen, carbon dioxide, pH, and bicarbonate levels. The partial pressure of oxygen in the blood is referred to as PaO2. The normal PaO2 level of a healthy adult is 80 to 100 mmHg. The PaO2 reading is more accurate than a SpO2 reading because it is not affected by hemoglobin levels. The PaCO2 level is the partial pressure of carbon dioxide in the blood. The normal PaCO2 level of a healthy adult is 35-45 mmHg. The normal range of pH level for arterial blood is 7.35-7.45, and the normal range for the bicarbonate (HCO3) level is 22-26. The SaO2 level is also obtained, which is the calculated arterial oxygen saturation level. See Table 11.2a for a summary of normal ranges of ABG values.[6]
Table 11.2a Normal Ranges of ABG Values
| Value | Description | Normal Range |
|---|---|---|
| pH | Acid-base balance of blood | 7.35-7.45 |
| PaO2 | Partial pressure of oxygen | 80-100 mmHg |
| PaCO2 | Partial pressure of carbon dioxide | 35-45 mmHg |
| HCO3 | Bicarbonate level | 22-26 mEq/L |
| SaO2 | Calculated oxygen saturation | 95-100% |
Hypoxia and Hypercapnia
Hypoxia is defined as a reduced level of tissue oxygenation. Hypoxia has many causes, ranging from respiratory and cardiac conditions to anemia. Hypoxemia is a specific type of hypoxia that is defined as decreased partial pressure of oxygen in the blood (PaO2), measured by an arterial blood gas (ABG).
Early signs of hypoxia are anxiety, confusion, and restlessness. As hypoxia worsens, the patient’s level of consciousness and vital signs will worsen, with increased respiratory rate and heart rate and decreased pulse oximetry readings. Late signs of hypoxia include bluish discoloration of the skin and mucous membranes called cyanosis. Cyanosis is most easily seen around the lips and in the oral mucosa. A sign of chronic hypoxia is clubbing, a gradual enlargement of the fingertips (see Figure 11.1[7]). See Table 11.2b for symptoms and signs of hypoxia.[8]

Hypercapnia is an elevated level of carbon dioxide in the blood. This level is measured by the PaCO2 level in an ABG test and is indicated when the PaCO2 level is higher than 45. Hypercapnia is typically caused by hypoventilation or areas of the alveoli that are ventilated but not perfused. In a state of hypercapnia or hypoventilation, there is an accumulation of carbon dioxide in the blood. The increased carbon dioxide causes the pH of the blood to drop, leading to a state of respiratory acidosis. You can read more about respiratory acidosis in the “Fluids and Electrolytes” chapter of the Open RN Nursing Fundamentals book. Patients with hypercapnia can present with tachycardia, dyspnea, flushed skin, confusion, headaches, and dizziness. If the hypercapnia develops gradually over time, such as in a patient with chronic obstructive pulmonary disease (COPD), symptoms may be mild or may not be present at all. Hypercapnia is managed by addressing its underlying cause. A noninvasive positive pressure device such as a BiPAP may provide support to patients who are having trouble breathing normally, but if this is not sufficient, intubation may be required.[9]
Table 11.2b Symptoms and Signs of Hypoxia
| Signs & Symptoms | Description |
|---|---|
| Restlessness | Patient may become increasingly fidgety, move about the bed, demonstrate signs of anxiety and agitation. Restlessness is an early sign of hypoxia. |
| Tachycardia | An elevated heart rate (above 100 beats per minute in adults) can be an early sign of hypoxia. |
| Tachypnea | An increased respiration rate (above 20 breaths per minute in adults) is an indication of respiratory distress. |
| Shortness of breath (Dyspnea) | Shortness of breath is a subjective symptom of not getting enough air. Depending on severity, dyspnea causes increased levels of anxiety. |
| Oxygen saturation level (SpO2) | Oxygen saturation levels should be above 94% for an adult without an underlying respiratory condition. |
| Use of accessory muscles | Use of neck or intercostal muscles when breathing is an indication of respiratory distress. |
| Noisy breathing | Audible noises with breathing are an indication of respiratory conditions. Assess lung sounds with a stethoscope for adventitious sounds such as wheezing, rales, or crackles. Secretions can plug the airway, thereby decreasing the amount of oxygen available for gas exchange in the lungs. |
| Flaring of nostrils or pursed lip breathing | Flaring is a sign of hypoxia, especially in infants. Pursed-lip breathing is a technique often used in patients with COPD. This breathing technique increases the amount of carbon dioxide exhaled so that more oxygen can be inhaled. |
| Position of patient | Patients in respiratory distress may sit up or lean over by resting arms on their legs to enhance lung expansion. Patients who are hypoxic may not be able to lie flat in bed. |
| Ability of patient to speak in full sentences | Patients in respiratory distress may be unable to speak in full sentences or may need to catch their breath between sentences. |
| Skin color (Cyanosis) | Changes in skin color to bluish or gray are a late sign of hypoxia. |
| Confusion or loss of consciousness (LOC) | This is a worsening sign of hypoxia. |
| Clubbing | Clubbing, a gradual enlargement of the fingertips, is a sign of chronic hypoxia. |
Treating Hypoxia
Acute hypoxia is a medical emergency and should be treated promptly with oxygen therapy. Failure to initiate oxygen therapy when needed can result in serious harm or death of the patient. Although oxygen is considered a medication that requires a prescription, oxygen therapy may be initiated without a physician’s order in emergency situations as part of the nurse’s response to the “ABCs,” a common abbreviation for airway, breathing, and circulation. Most agencies have a protocol in place that allows nurses to apply oxygen in emergency situations. After applying oxygen as needed, the nurse then contacts the provider, respiratory therapist, or rapid response team, depending on the severity of hypoxia. Devices such high flow oxymasks, CPAP, BiPAP, or mechanical ventilation may be initiated by the respiratory therapist or provider to deliver higher amounts of inspired oxygen. Various types of oxygenation devices are further explained in the “Oxygenation Equipment” section.
Prescription orders for oxygen therapy will include two measurements of oxygen to be delivered - the oxygen flow rate and the fraction of inspired oxygen (FiO2). The oxygen flow rate is the number dialed up on the oxygen flow meter between 1 L/minute and 15 L/minute. Fio2 is the concentration of oxygen the patient inhales. Room air contains 21% oxygen concentration, so the FiO2 for supplementary oxygen therapy will range from 21% to 100% concentration.
In addition to administering oxygen therapy, there are several other interventions the nurse should consider implementing to a hypoxic patient. Additional interventions used to treat hypoxia in conjunction with oxygen therapy are outlined in Table 11.2c.[10]
Table 11.2c Interventions to Manage Hypoxia
| Interventions | Additional Information |
|---|---|
| Raise the Head of the Bed | Raising the head of the bed to high Fowler’s position promotes effective chest expansion and diaphragmatic descent, maximizes inhalation, and decreases the work of breathing. Patients with COPD who are short of breath may gain relief by sitting upright or leaning over a bedside table while in bed. |
| Encourage Enhanced Breathing and Coughing Techniques | Enhanced breathing and coughing techniques such as using pursed-lip breathing, coughing and deep breathing, huffing technique, incentive spirometry, and flutter valves may assist patients to clear their airway while maintaining their oxygen levels. See the following “Enhanced Breathing and Coughing Techniques” section for additional information regarding these techniques. |
| Manage Oxygen Therapy and Equipment | If the patient is already on supplemental oxygen, ensure the equipment is turned on, set at the required flow rate, correctly positioned on the patient, and properly connected to an oxygen supply source. If a portable tank is being used, check the oxygen level in the tank. Ensure the connecting oxygen tubing is not kinked, which could obstruct the flow of oxygen. Feel for the flow of oxygen from the exit ports on the oxygen equipment. In hospitals where medical air and oxygen are used, ensure the patient is connected to the oxygen flow port. Hospitals in America follow the national standard that oxygen flow ports are green and air outlets are yellow. |
| Assess the Need for Respiratory Medications | Pharmacological management is essential for patients with respiratory disease such as asthma, COPD, or severe allergic response. Bronchodilators effectively relax smooth muscles and open airways. Glucocorticoids relieve inflammation and also assist in opening air passages. Mucolytics decrease the thickness of pulmonary secretions so that they can be expectorated more easily. |
| Provide Oral Suctioning if Needed | Some patients may have a weakened cough that inhibits their ability to clear secretions from the mouth and throat. Patients with muscle disorders or those who have experienced a cerebral vascular accident (CVA) are at risk for aspiration pneumonia, which is caused by the accidental inhalation of material from the mouth or stomach. Provide oral suction if the patient is unable to clear secretions from the mouth and pharynx. See the chapter on “Tracheostomy Care and Suctioning” for additional details on suctioning. |
| Provide Pain Relief If Needed | Provide adequate pain relief if the patient is reporting pain. Pain increases anxiety and may inhibit the patient’s ability to take in full breaths. |
| Consider the Side Effects of Pain Medications | A common side effect of pain medication is sedation and respiratory depression. For more information about interventions to manage respiratory depression, see the “Oxygenation” chapter in the Open RN Nursing Fundamentals textbook. |
| Consider Other Devices to Enhance Clearance of Secretions | Chest physiotherapy and specialized devices assist with secretion clearance, such as handheld flutter valves or vests that inflate and vibrate the chest wall. Consider requesting a consultation with a respiratory therapist based on the patient’s situation. |
| Plan Frequent Rest Periods Between Activities | Patients experiencing hypoxia often feel short of breath and fatigue easily. Allow the patient to rest frequently, and space out interventions to decrease oxygen demand in patients whose reserves are likely limited. |
| Consider Other Potential Causes of Dyspnea | If a patient’s level of dyspnea is worsening, assess for other underlying causes in addition to the primary diagnosis. Are there other respiratory, cardiovascular, or hematological conditions such as anemia occurring? Start by reviewing the patient’s most recent hemoglobin and hematocrit lab results. Completing a thorough assessment may reveal abnormalities in these systems to report to the health care provider. |
| Consider Obstructive Sleep Apnea | Patients with obstructive sleep apnea (OSA) are often not previously diagnosed prior to hospitalization. The nurse may notice the patient snores, has pauses in breathing while snoring, or awakens not feeling rested. These signs may indicate the patient is unable to maintain an open airway while sleeping, resulting in periods of apnea and hypoxia. If these apneic periods are noticed but have not been previously documented, the nurse should report these findings to the health care provider for further testing and follow-up. Testing consists of using continuous pulse oximetry while the patient is sleeping to determine if the patient is hypoxic during these episodes and if a CPAP device should be prescribed. See the box below for additional information regarding OSA. |
| Anxiety | Anxiety often accompanies the feeling of dyspnea and can worsen it. Anxiety in patients with COPD is chronically undertreated. It is important for the nurse to address the feelings of anxiety and dyspnea. Anxiety can be relieved by teaching enhanced breathing and coughing techniques, encouraging relaxation techniques, or administering antianxiety medications. |
Obstructive Sleep Apnea (OSA) is the most common type of sleep apnea. See Figure 11.2[11] for an illustration of OSA. As soft tissue falls to the back of the throat, it impedes the passage of air (blue arrows) through the trachea and is characterized by repeated episodes of complete or partial obstructions of the upper airway during sleep. The episodes of breathing cessations are called “apneas,” meaning “without breath.” Despite the effort to breathe, apneas are associated with a reduction in blood oxygen saturation due to the obstruction of the airway. Treatment for OSA often includes the use of a CPAP device.
Enhanced Breathing and Coughing Techniques
In addition to oxygen therapy and the interventions listed in Table 11.2c to implement for a patient experiencing dyspnea and hypoxia, there are several techniques a nurse can teach a patient to use to enhance their breathing and coughing. These techniques include pursed-lip breathing, incentive spirometry, coughing and deep breathing, and the huffing technique.
Pursed-Lip Breathing
Pursed-lip breathing is a technique that allows people to control their oxygenation and ventilation. The technique requires a person to inspire through the nose and exhale through the mouth at a slow controlled flow. See Figure 11.3[12] for an illustration of pursed-lip breathing. This type of exhalation gives the person a puckered or pursed appearance. By prolonging the expiratory phase of respiration, a small amount of positive end-expiratory pressure (PEEP) is created in the airways that helps to keep them open so that more air can be exhaled, thus reducing air trapping that occurs in some conditions such as COPD. Pursed-lip breathing often relieves the feeling of shortness of breath, decreases the work of breathing, and improves gas exchange. People also regain a sense of control over their breathing while simultaneously increasing their relaxation.[13]

View the COPD Foundation's YouTube video to learn more about pursed-lip breathing:
Breathing Techniques[14]
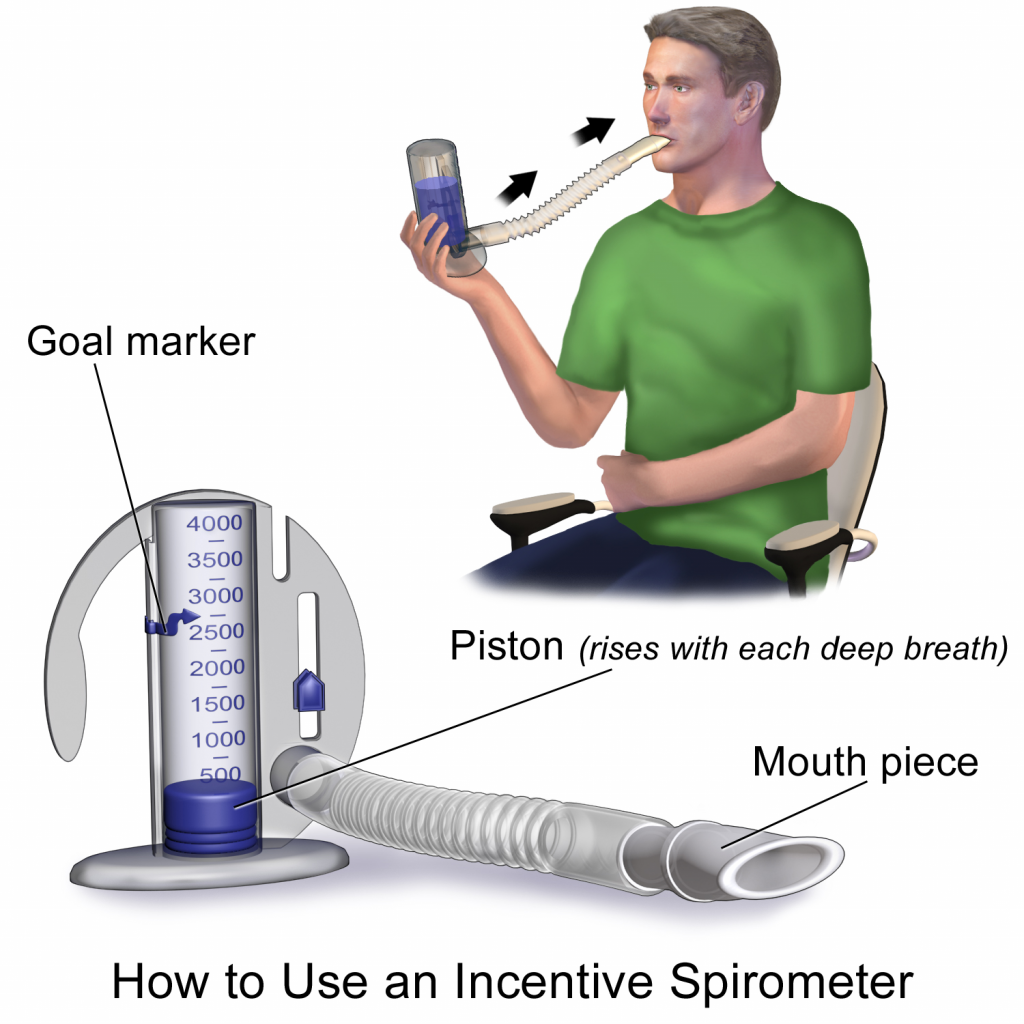
Incentive Spirometry
An incentive spirometer is a medical device often prescribed after surgery to prevent and treat atelectasis. Atelectasis occurs when alveoli become deflated or filled with fluid and can lead to pneumonia. See Figure 11.4[15] for an image of a patient using an incentive spirometer. While sitting upright, the patient should breathe in slowly and deeply through the tubing with the goal of raising the piston to a specified level. The patient should attempt to hold their breath for 5 seconds, or as long as tolerated, and then rest for a few seconds. This technique should be repeated by the patient 10 times every hour while awake.[16] The nurse may delegate this intervention to unlicensed assistive personnel, but the frequency in which it is completed and the volume achieved should be documented and monitored by the nurse.
Coughing and Deep Breathing
Teaching the coughing and deep breathing technique is similar to incentive spirometry but no device is required. The patient is encouraged to take deep, slow breaths and then exhale slowly. After each set of breaths, the patient should cough. This technique is repeated 3 to 5 times every hour.
Huffing Technique
The huffing technique is helpful for patients who have difficulty coughing. Teach the patient to inhale with a medium-sized breath and then make a sound like “Ha” to push the air out quickly with the mouth slightly open.
Vibratory PEP Therapy
Vibratory Positive Expiratory Pressure (PEP) therapy uses handheld devices such as “flutter valves” or “Acapella” devices for patients who need assistance in clearing mucus from their airways. These devices (see Figure 11.5[17]) require a prescription and are used in collaboration with a respiratory therapist or advanced health care provider. To use Vibratory PEP therapy, the patient should sit up, take a deep breath, and blow into the device. A flutter valve within the device creates vibrations that help break up the mucus so the patient can cough it up and spit it out. Additionally, a small amount of positive end-expiratory pressure (PEEP) is created in the airways that helps to keep them open so that more air can be exhaled.

Visit NHS University Hospitals Plymouth Physiotherapy's "Acapella" video on YouTube to review using a flutter valve device[18]
A blood glucose reading less than 70 associated with symptoms such as irritability, shakiness, hunger, weakness, or confusion.

